Beyond the "Fatty Liver": How MASLD Signals a Global Metabolic Crisis (Diabetes, Obesity, & CVD)
Think you just have a 'fatty liver'? Discover why MASLD is actually a signal of global metabolic disharmony, linking liver health to diabetes, obesity, and heart disease in this research guide
METABOLISM
Dr. T.S. Didwal, M.D.(Internal Medicine)
12/18/202512 min read
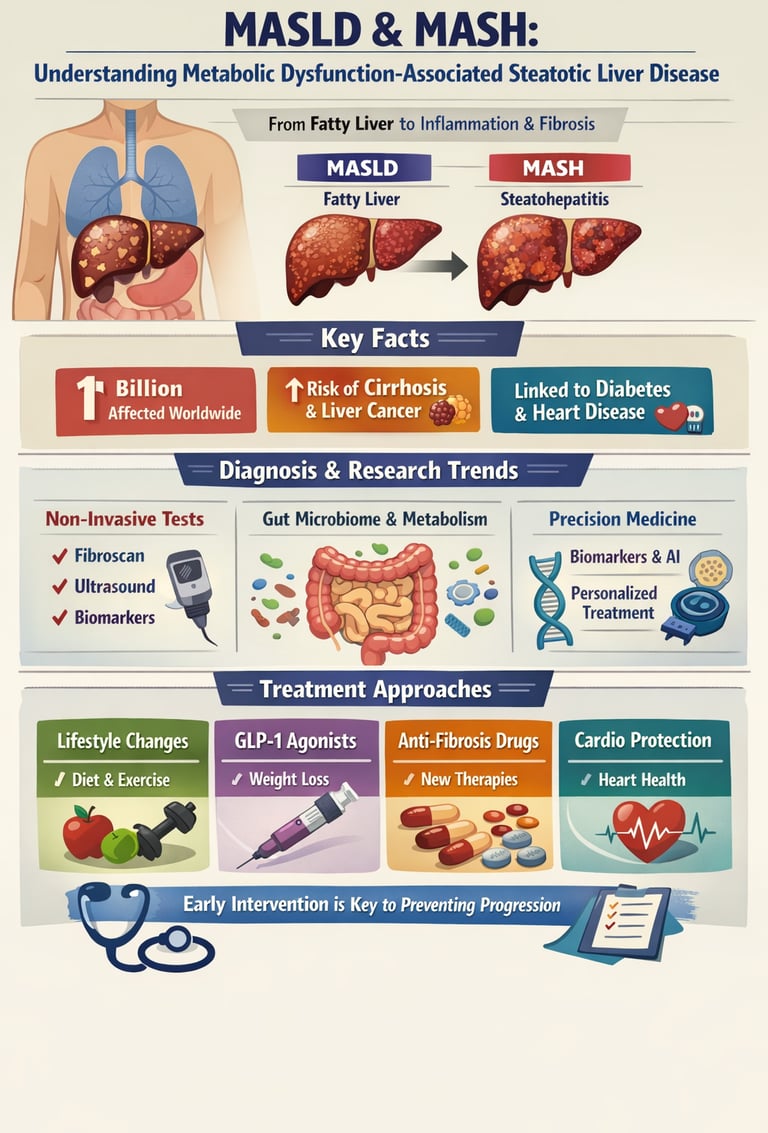
Metabolic dysfunction-associated steatotic liver disease (MASLD), formerly known as non-alcoholic fatty liver disease (NAFLD), represents one of the most pressing health challenges of our time. With an estimated prevalence affecting over a billion people worldwide, MASLD has quietly become the leading cause of chronic liver disease globally. But what exactly is this condition, and why should you care about it?
Imagine your liver as a silent sentinel, the master conductor managing energy for your entire body. For decades, we referred to its most common ailment simply as "fatty liver," viewing it as an isolated storage issue—a minor glitch in an otherwise healthy system. But as we move through 2025, our perspective has shifted dramatically. We now recognize Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD) not as a localized problem, but as the loudest alarm in a global metabolic crisis.
MASLD is the "ground zero" of metabolic disharmony. It is a clear signal that the delicate balance between your heart, blood sugar, and weight has fallen out of sync. When the liver struggles with fat, it triggers a systemic ripple effect of inflammation, fueling the progression of type 2 diabetes and cardiovascular disease. This guide explores the interconnected metabolic spectrum, helping you move beyond the "fatty" label to restore harmony to your body’s most vital rhythms.
Clinical Pearls
1. The "10% Rule" for Liver Reversal
In the world of MASLD, the number 10 is more than just a digit; it’s a therapeutic target. While losing any amount of weight helps reduce fat in the liver (steatosis), clinical evidence shows that losing 10% of your total body weight is the threshold required to actually reverse liver scarring (fibrosis) and clear the inflammation seen in MASH. Think of your liver as a sponge: modest weight loss squeezes out the "water" (fat), but 10% loss starts to repair the sponge's actual fibers.
2. The Liver is a "Window" to the Heart
A crucial pearl for patients is that MASLD is rarely a "liver-only" condition. Scientists now view the liver as a metabolic sentinel. If there is fat in the liver, it is a high-probability predictor of plaque in the coronary arteries. In fact, patients with MASLD are statistically more likely to experience a cardiovascular event (like a heart attack) before they ever reach the stage of liver failure. Treating the liver is, in essence, a primary strategy for protecting the heart.
3. The "Silent Alarm" of the Gut-Liver Axis
Your gut and liver are "best friends" connected by a direct blood line called the portal vein. When the gut microbiome becomes imbalanced (dysbiosis), the intestinal barrier becomes "leaky." This allows bacterial toxins to travel directly to the liver, fueling inflammation.
Patient Perspective: Eating high-fiber foods and probiotics isn't just for digestion; it acts as a "filter" that prevents toxic biological mail from being delivered to your liver’s front door.
4. MASH: The Invisible Transition
The most dangerous phase of the disease is the transition from MASLD (simple fat) to MASH (fat plus inflammation). This transition is "silent" because the liver itself doesn't have pain-sensing nerves. You cannot feel your liver becoming inflamed. This is why modern medicine has shifted toward Non-Invasive Tests (NITs), like the FibroScan or specialized blood panels, which acts as a "metabolic sonar" to detect inflammation that a standard physical exam would miss.
5. The "Lean MASLD" Paradox
A common misconception is that you must be "overweight" to have a fatty liver. "Lean MASLD" occurs in individuals with a healthy Body Mass Index (BMI) who have a genetic predisposition or a high percentage of visceral fat (fat stored around the internal organs). This highlights that metabolic health is about function, not just appearance. Even if the scale looks good, high sugar intake and low activity can still cause the liver to store "toxic fat."
MASLD and MASH: Understanding Metabolic Dysfunction-Associated Steatotic Liver Disease
What is MASLD? Understanding the Basics
MASLD occurs when fat accumulates in the liver (hepatic steatosis) in individuals without significant alcohol consumption. Unlike its predecessor name, the term "metabolic dysfunction-associated" emphasizes the underlying metabolic abnormalities driving the condition rather than simply the presence of fat in the liver (Huang et al., 2025).
The progression from MASLD to MASH (metabolic dysfunction-associated steatohepatitis) marks a critical turning point. While MASLD represents simple steatosis, MASH involves inflammation and hepatocellular injury, significantly increasing the risk of cirrhosis and liver failure. Understanding this distinction is crucial for determining treatment urgency and managing long-term health outcomes.
Research Advances in Diagnosis: What Recent Studies Show
1. Diagnostic Innovations and Personalized Approaches
Wang et al. (2024) provide cutting-edge insights into the diagnosis and treatment of MASLD and MASH in their analysis, published in the Annals of Medicine. The researchers emphasize that traditional diagnostic methods are evolving, with noninvasive diagnostic techniques now at the forefront of clinical practice.
Key takeaway: Rather than relying solely on liver biopsy—an invasive procedure—modern diagnosis utilizes imaging studies like ultrasound, elastography, and biomarker panels. These emerging diagnostic tools can detect hepatic fibrosis, assess disease severity, and help identify patients at highest risk of progression to advanced liver disease.
2. The Microbiome-Insulin Resistance Connection
Dua and colleagues (2025) explore a fascinating intersection in Frontiers in Medicine: the relationship between gut microbiome composition, insulin resistance, and MASLD development. This research highlights how dysbiosis (imbalance in gut bacteria) creates a perfect storm for metabolic dysfunction, with the gut-liver axis playing a fundamental role in disease pathogenesis (Dua et al., 2025).
When the intestinal barrier becomes compromised, bacterial metabolites and lipopolysaccharides trigger systemic inflammation, worsening both insulin resistance and liver fat accumulation. Furthermore, patients with MASLD and concurrent diabetes show particularly accelerated disease progression.
Key takeaway: The interplay of gut microbiome, insulin resistance, and diabetes suggests that therapeutic interventions targeting gut health—such as probiotics, dietary modifications, and lifestyle interventions—may represent promising avenues for MASLD prevention and management.
3. Metabolic Dysfunction and Systemic Implications
In a landmark review published in the New England Journal of Medicine, Targher, Valenti, and Byrne (2025) provide comprehensive coverage of metabolic dysfunction–associated steatotic liver disease and its systemic complications. The authors emphasize that MASLD is not simply a liver condition but a manifestation of broader metabolic disease (Targher et al., 2025).
These researchers highlight that patients with MASLD face significantly elevated risks for cardiovascular disease, chronic kidney disease, and type 2 diabetes mellitus. The condition represents what they term a "metabolic syndrome of the liver"—a condition requiring holistic, multidisciplinary management.
Key takeaway: Treating MASLD requires addressing underlying metabolic dysfunction comprehensively, including management of dyslipidemia, hypertension, obesity, and impaired glucose tolerance. A siloed approach focusing only on liver health will inevitably miss critical opportunities for preventing systemic complications.
4. MASLD as an Evolving Epidemic
Lake-Bakaar (2025) contextualizes MASLD within the broader landscape of modern medicine in the Journal of Clinical Medicine. The author presents new perspectives on an evolving epidemic, noting that the prevalence of MASLD correlates directly with rising rates of obesity and metabolic syndrome across developed and developing nations alike
This perspective piece emphasizes that without urgent intervention at the population level, MASLD prevalence will continue to climb, straining healthcare systems and creating enormous disease burden. The author advocates for both clinical innovations and public health initiatives aimed at metabolic disease prevention.
Key takeaway: Understanding MASLD requires recognizing it as an epidemic driven by modifiable lifestyle factors, making prevention strategies and early detection programs essential public health priorities.
5. Pathophysiology and Clinical Pearls
Girish and John (2025) provide an excellent clinical overview in their StatPearls entry, covering the pathophysiology, noninvasive diagnostics, and clinical management of MASLD. Their comprehensive summary emphasizes that MASLD development involves a complex interplay of genetics, lifestyle factors, and metabolic derangements
The authors detail how hepatic lipid accumulation initiates a cascade of events: increased hepatic oxidative stress, mitochondrial dysfunction, and endoplasmic reticulum stress. These cellular mechanisms then trigger inflammation, progressive fibrosis, and potentially irreversible liver damage.
Key takeaway: Modern understanding of MASLD pathophysiology has moved beyond simple "two-hit" models to recognize complex, multifactorial disease mechanisms that demand sophisticated, personalized treatment approaches.
6. Personalized Diagnostics and Biomarker Discovery
Tantu and colleagues (2025) advance the field through their work on pathophysiology, noninvasive diagnostics, and emerging personalized treatments published in npj Gut Liver. Their research highlights how biomarker discovery and machine learning algorithms are enabling truly personalized diagnostic and prognostic approaches (Tantu et al., 2025).
Rather than one-size-fits-all diagnostics, these researchers show how genomic profiling, proteomic analysis, and metabolomic assessments can identify subgroups of patients with distinct disease patterns and treatment responses. This represents a paradigm shift toward precision medicine in MASLD management.
Key takeaway: The future of MASLD diagnosis lies in personalized diagnostic algorithms that integrate multiple data streams, enabling clinicians to tailor interventions precisely to individual patient biology.
The Latest Evidence: What Every Patient Should Know
Understanding Disease Mechanism and Systemic Risk
Huang and colleagues (2025) provide an authoritative summary in Nature Reviews Disease Primers, establishing that MASLD in adults represents far more than isolated liver pathology. Their comprehensive review synthesizes current evidence showing that metabolic dysfunction-associated steatotic liver disease fundamentally alters multiple organ systems (Huang et al., 2025).
The authors emphasize that MASLD serves as a marker of systemic metabolic disease, predicting not only progression to cirrhosis and hepatocellular carcinoma but also cardiovascular events, renal dysfunction, and metabolic complications. This systemic perspective demands that clinical management extends beyond hepatology into primary care, cardiology, and endocrinology.
Key takeaway: Patients with MASLD require comprehensive metabolic assessment and multidisciplinary care addressing all facets of metabolic dysfunction, not just liver-specific markers.
Biomarkers and Disease Progression
Zhang and colleagues (2025) conducted sophisticated analysis using weighted gene co-expression network analysis and machine learning to identify disease progression biomarkers in metabolic associated steatotic liver disease. Published in Journal of Translational Medicine, this research reveals specific molecular signatures that predict which MASLD patients will progress to advanced liver disease (Zhang et al., 2025).
These progression biomarkers enable clinicians to stratify patients by risk level, allowing for intensive surveillance and early intervention in high-risk individuals. The identification of specific gene networks involved in fibrosis progression also suggests novel therapeutic targets.
Key takeaway: Machine learning-informed biomarker panels represent the future of MASLD risk stratification, enabling preventive strategies focused on patients with the greatest need for intervention.
Cardiovascular Complications in Younger Populations
Perhaps most alarming, Chung and colleagues (2025) demonstrate in Scientific Reports that metabolic dysfunction-associated steatotic liver disease increases cardiovascular disease risk in young adults (Chung et al., 2025). Their research reveals that MASLD is no longer primarily a condition of aging populations—younger adults are increasingly affected and face substantial cardiovascular mortality risk.
This finding challenges the assumption that MASLD can be safely observed in younger patients. Instead, young adults with MASLD warrant aggressive cardiovascular risk assessment and intervention, potentially including pharmacotherapy to prevent myocardial infarction and stroke.
Key takeaway: Age is not protective against MASLD complications. Young adults with this condition require comprehensive cardiovascular risk assessment and aggressive preventive management to avoid premature mortality.
Treatment Advances: From Lifestyle to Pharmacotherapy
Foundational Approach: Lifestyle Modification
All reviewed studies emphasize that lifestyle intervention remains the cornerstone of MASLD management. Weight loss of 5-10% through caloric restriction and structured exercise programs can significantly improve hepatic steatosis. More substantial weight loss (>10%) demonstrates benefits for liver inflammation and fibrosis, sometimes achieving complete histological resolution of MASH.
Emerging Pharmacological Treatments
The research landscape reveals several promising therapeutic agents:
GLP-1 Receptor Agonists: These medications improve insulin sensitivity, promote weight loss, and reduce hepatic inflammation. Several large trials are evaluating their role in MASLD and MASH treatment.
Thiazolidinediones: Improve insulin resistance and hepatic fibrosis in select patient populations, though concerns about weight gain and side effects limit broader application.
Antioxidants and Anti-inflammatory Agents: Multiple agents targeting oxidative stress and inflammatory pathways show promise in early-stage research.
Fibrosis-Targeting Therapies: Novel agents directly addressing hepatic fibrosis represent a major research focus, with several agents moving through clinical trials.
Key takeaway: While no FDA-approved MASLD-specific pharmacotherapy currently exists, the pipeline includes multiple promising agents targeting distinct disease mechanisms, with approval likely within the coming years.
Frequently Asked Questions About MASLD
Q: How common is MASLD? A: MASLD affects approximately 25-30% of the global population, making it the most common chronic liver disease worldwide. Prevalence rises to 50-75% among patients with obesity or type 2 diabetes.
Q: Can MASLD be cured? A: While complete resolution is possible with substantial weight loss and metabolic improvement, many patients require ongoing management. Early detection and aggressive intervention offer the best prognosis for preventing progression to cirrhosis and liver failure.
Q: What lifestyle changes matter most? A: Weight loss through combined caloric restriction and aerobic exercise, improved diet quality emphasizing whole grains and reduced refined carbohydrates, limiting alcohol consumption, and managing diabetes and hypertension all significantly impact disease progression.
Q: Should everyone be screened for MASLD? A: Screening is particularly important for individuals with metabolic syndrome, obesity, type 2 diabetes, or dyslipidemia. Current guidelines recommend considering screening in these high-risk populations.
Q: How often should MASLD patients see specialists? A: This depends on disease severity. Patients with advanced fibrosis or cirrhosis require frequent monitoring (every 3-6 months), while those with simple steatosis may need annual assessment. Discuss individualized monitoring with your healthcare provider.
Q: Are probiotics and supplements helpful? A: While some research suggests potential benefits of specific probiotic strains and antioxidants, evidence remains preliminary. Always discuss supplements with your healthcare provider before starting, as some may interact with medications or worsen liver function.
Q: Can MASLD lead to liver cancer? A: Yes, patients with advanced MASLD progressing to cirrhosis face increased risk of hepatocellular carcinoma. Regular surveillance through imaging and biomarkers becomes essential once cirrhosis develops.
Call to Action: Take Control of Your Liver Health Today
If you're concerned about MASLD risk or have been diagnosed with this condition, the time to act is now. The latest research provides unprecedented opportunities for preventing disease progression and achieving metabolic health.
Start by scheduling an evaluation with your primary care physician to assess your risk for MASLD through appropriate screening. If you have metabolic syndrome, obesity, prediabetes, or type 2 diabetes, testing becomes particularly important.
Commit to lifestyle transformation: Begin with modest weight loss goals (5-10%), increase physical activity to 150 minutes weekly of moderate exercise, and adopt a Mediterranean or whole-food plant-based diet emphasizing fiber and minimizing refined carbohydrates.
Seek specialized care if needed: If standard interventions don't achieve targets or if you have evidence of advanced fibrosis, consultation with a hepatologist experienced in MASLD management can help you access cutting-edge therapies and enroll in clinical trials evaluating emerging treatments.
Stay informed: The MASLD landscape is rapidly evolving. Remain engaged with your healthcare team about new developments, and don't hesitate to discuss clinical trial participation if standard approaches haven't achieved your goals.
Your liver health directly impacts your longevity and quality of life. The evidence is clear: early detection, aggressive metabolic optimization, and multidisciplinary management of MASLD can prevent progression to devastating complications and restore metabolic health. The time to act is now.
Conclusion
The era of dismissing "fatty liver" as a minor concern is over. As we navigate the health landscape of 2025, we now recognize MASLD (Metabolic Dysfunction-Associated Steatotic Liver Disease) as the central hub of a global metabolic crisis. This isn't just about liver fat; it is a profound state of metabolic disharmony that serves as an early warning system for type 2 diabetes, obesity, and cardiovascular disease.
Research now confirms that the liver is the "master conductor" of your metabolic orchestra. When it falls out of tune, the ripple effects are felt in every major organ system. The good news? This spectrum is highly responsive to intervention. By targeting liver health through intentional lifestyle shifts—aiming for that critical 10% weight loss and supporting the gut-liver axis—you aren't just "fixing your liver." You are restoring harmony to your entire body, reducing heart risk, and reclaiming your metabolic future.
The Takeaway: Don’t wait for symptoms that may never arrive. Treat MASLD as the "silent alarm" it is. Early detection today is the key to preventing the metabolic complications of tomorrow.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Individual circumstances vary, and treatment decisions should always be made in consultation with qualified healthcare professionals.
Related Articles
Improve Leptin & Adiponectin: Science-Based Guide to Metabolic Health | DR T S DIDWAL
The Best Dietary Fat Balance for Insulin Sensitivity, Inflammation, and Longevity | DR T S DIDWAL
High Triglyceride Levels: 5 New Facts to Help You Lower Your Risk | DR T S DIDWAL
Lower Blood Pressure Naturally: Evidence-Based Exercise Guide for Metabolic Syndrome | DR T S DIDWAL
Movement Snacks: How VILPA Delivers Max Health Benefits in Minutes | DR T S DIDWAL
The BMI Paradox: Why "Normal Weight" People Still Get High Blood Pressure | DR T S DIDWAL
How Insulin Resistance Accelerates Cardiovascular Aging | DR T S DIDWAL
The Metabolic Triad: Why Diabetes, Obesity & CVD Are One Epidemic | DR T S DIDWAL
Breakthrough Research: Leptin Reduction is Required for Sustained Weight Loss | DR T S DIDWAL
References
Chung, G. E., Yu, S. J., Yoo, J. J., et al. (2025). Metabolic dysfunction-associated steatotic liver disease increases cardiovascular disease risk in young adults. Scientific Reports, 15, 5777. https://doi.org/10.1038/s41598-025-89293-6
Dua, A., Kumari, R., Singh, M., Kumar, R., Pradeep, S., Ojesina, A. I., & Kumar, R. (2025). Metabolic dysfunction-associated steatotic liver disease (MASLD): The interplay of gut microbiome, insulin resistance, and diabetes. Frontiers in Medicine, 12, 1618275. https://doi.org/10.3389/fmed.2025.1618275
Girish, V., & John, S. (2025, August 9). Metabolic dysfunction-associated steatotic liver disease (MASLD). StatPearls - NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK541033/
Huang, D. Q., Wong, V. W. S., Rinella, M. E., et al. (2025). Metabolic dysfunction-associated steatotic liver disease in adults. Nature Reviews Disease Primers, 11, 14. https://doi.org/10.1038/s41572-025-00599-1
Lake-Bakaar, G. (2025). Metabolic dysfunction-associated steatotic liver disease (MASLD): New perspectives on an evolving epidemic. Journal of Clinical Medicine, 14(24), 8872. https://doi.org/10.3390/jcm14248872
Tantu, M. T., Farhana, F. Z., Haque, F., et al. (2025). Pathophysiology, noninvasive diagnostics and emerging personalized treatments for metabolic associated liver diseases. npj Gut Liver, 2, 18. https://doi.org/10.1038/s44355-025-00030-2
Targher, G., Valenti, L., & Byrne, C. D. (2025). Metabolic dysfunction–associated steatotic liver disease. New England Journal of Medicine, 393(7), 683–698. https://doi.org/10.1056/nejmra2412865
Wang, D., Miao, J., Zhang, L., & Zhang, L. (2024). Research advances in the diagnosis and treatment of MASLD/MASH. Annals of Medicine, 57(1), 2445780. https://doi.org/10.1080/07853890.2024.2445780
Zhang, W., Lu, W., Jiao, Y., et al. (2025). Identifying disease progression biomarkers in metabolic associated steatotic liver disease (MASLD) through weighted gene co-expression network analysis and machine learning. Journal of Translational Medicine, 23, 472. https://doi.org/10.1186/s12967-025-06490-7