The Best Dietary Fat Balance for Insulin Sensitivity, Inflammation, and Longevity
Discover why fat quality, not calorie count, drives insulin resistance and aging. Learn the optimal SFA, MUFA, and PUFA ratios for metabolic health based on 2025 evidence
NUTRITION
Dr. T.S. Didwal, M.D.(Internal Medicine)
12/20/202513 min read
When was the last time you looked past the "total fat" line on a nutrition label? Most of us were raised to focus on quantity, but cutting-edge research reveals that the type of fat you consume is far more critical than the amount. We are officially moving beyond the era of "low-fat" dogma into a more nuanced reality: your metabolic health depends less on subtraction and more on a precise molecular balance.
For decades, the standard prescription for a healthy heart was simple: eat less fat. However, emerging 2025 evidence suggests that obsessing over "low-fat" targets might actually be sabotaging your longevity. The real secret to metabolic resilience isn't found in a calorie counter, but in a mathematical ratio of fatty acids that can either quiet systemic inflammation or set it ablaze.
Recent scientific breakthroughs demonstrate that saturated (SFAs), monounsaturated (MUFAs), and polyunsaturated fatty acids (PUFAs) act as biological signals, each triggering a distinct physiological response. By mastering these differences, you can transform your nutrition from a guessing game into a targeted strategy for disease prevention and long-term wellness.
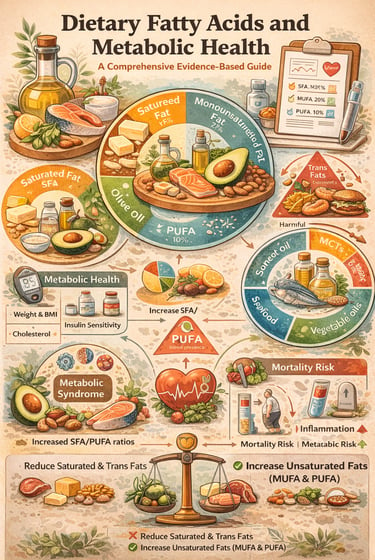
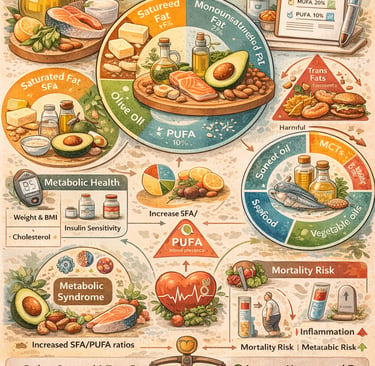
Clinical Pearls: The New Rules of Fat
1. The "Seesaw" Principle
Stop counting grams; start measuring ratios.
The balance between Saturated (SFA) and Polyunsaturated (PUFA) fats is a better predictor of death than total fat intake.
The Goal: Keep the "Unsaturated" side of the seesaw heavier.
The Ratio: Aim for a 1:1 or 1:2 ratio (SFA to PUFA). Most Western diets are currently 2.5:1, which creates a metabolic "tipping point" toward disease.
2. The "Immune Thermostat"
Fat is a signal, not just fuel.
Your fat choices act as a remote control for your immune system.
Saturated Fats: Can act like a "false alarm," triggering Toll-like receptors and putting your body in a pro-inflammatory state.
Polyunsaturated Fats: Send a "resolve" signal, telling your immune system to switch from "attack mode" to "repair mode."
The Marker: Track your Neutrophil-to-Albumin ratio—it’s the biological window into how your diet is affecting your internal inflammation.
3. The Metabolic Workhorse (MUFAs)
Replace, don't just subtract.
Monounsaturated fats (found in Extra Virgin Olive Oil and Avocados) are the "Goldilocks" of fuel.
They are uniquely effective at fixing glucolipid dysfunction (where high blood sugar meets bad cholesterol).
Pro-Tip: Replacing just a small portion of daily butter or lard with olive oil sharpens insulin sensitivity and powers up your mitochondria.
4. Your "Fat Fingerprint"
One size fits none.
Everyone has a unique plasma metabolite signature.
If you aren't seeing results on a "standard" healthy diet, your specific biology may require a different fatty acid ratio.
The Future: Use biomarkers to tailor your fat intake to your specific genetic and microbial makeup.
5.The Food Matrix
Source is as vital as chemistry.
A fat's "neighborhood" matters.
Whole Foods: Saturated fats bundled with fiber and minerals (like fermented dairy or coconuts) behave differently than "isolated" fats in processed meats.
Rule of Thumb: Prioritize fats in their whole-food form to get the co-nutrients needed for healthy metabolism.
What the Latest Research Says About Fatty Acid Types
New 2025 research reveals that the proportion of saturated to polyunsaturated fats—not total quantity—is the secret to quieting systemic inflammation.
Study 1: The Foundation—Dietary Fatty Acids and Metabolic Health Overview
Szabó’s 2025 comprehensive review in Nutrients provides the conceptual backbone for modern dietary fat science, reframing fats not as passive energy sources but as active regulators of metabolic physiology. Drawing on a broad synthesis of human, mechanistic, and translational research, this review clarifies how fatty acid quality fundamentally determines metabolic health outcomes.
Beyond Calories: Fat as a Biological Signal
A central conclusion of the review is that dietary fats function as molecular signals that influence cellular behavior across multiple organ systems. Saturated, monounsaturated, and polyunsaturated fatty acids each exert distinct effects on:
Glucose and lipid homeostasis
Inflammatory signaling and immune regulation
Mitochondrial function and energy efficiency
Endothelial health and vascular integrity
Hormonal signaling and gene expression
This signaling perspective explains why equal-calorie diets with different fatty acid compositions produce markedly different metabolic outcomes.
Metabolic Health as a Systems Property
Szabó emphasizes that metabolic health cannot be reduced to single biomarkers such as LDL cholesterol or triglycerides. Instead, it reflects the coordinated performance of interconnected biological systems, including mitochondrial energy production, immune balance, and vascular function. Fatty acid composition influences these systems simultaneously, either reinforcing metabolic resilience or accelerating dysfunction.
Why Low-Fat Paradigms Failed
The review critically examines decades of low-fat dietary recommendations, concluding that they overlooked the qualitative differences between fat types. Simply reducing total fat intake often displaced beneficial unsaturated fats while increasing refined carbohydrates, inadvertently worsening insulin resistance, inflammation, and lipid profiles.
The Role of Fatty Acid–Derived Metabolites
A major contribution of this review is its focus on fatty acid–derived metabolites—bioactive molecules generated during fat metabolism that act as signaling intermediates. These metabolites modulate immune cell behavior, endothelial tone, mitochondrial activity, and even cognitive function, providing a mechanistic explanation for fat-type–specific health effects.
Individual Variability and Personalized Nutrition
Szabó highlights substantial interindividual variability in metabolic responses to dietary fats, driven by genetics, gut microbiome composition, baseline metabolic health, physical activity, and age. This heterogeneity undermines universal fat prescriptions and supports a shift toward personalized, biomarker-guided dietary strategies.
Key Takeaway
Dietary fat quality—not quantity—forms the foundation of metabolic health. Different fatty acids deliver distinct biological instructions that shape inflammation, energy metabolism, vascular function, and aging trajectories. Effective nutrition guidance must therefore move beyond low-fat dogma toward fat-type–specific and individualized approaches grounded in modern metabolic science.
Study 2: Fatty Acid Ratios and Mortality Risk—The Critical Connection
Liu er al. 2025 study in Lipids in Health and Disease delivers one of the clearest demonstrations to date that fat quality—not fat quantity—directly influences lifespan. Rather than relying on broad dietary categories, the investigators identified a precise and measurable dietary signal: the ratio of saturated fatty acids (SFAs) to polyunsaturated fatty acids (PUFAs).
The Core Finding
The study shows that a higher SFA:PUFA ratio is strongly associated with increased all-cause mortality, independent of total fat intake. Importantly, this relationship is not merely associative—it is biologically mediated through systemic inflammation.
The Key Biomarker: Neutrophil Percentage-to-Albumin Ratio
Liu et al. identified the neutrophil percentage-to-albumin ratio as a sensitive biological marker linking dietary fat composition to long-term survival:
Neutrophils reflect immune activation and inflammatory burden
Albumin reflects nutritional status and anti-inflammatory capacity
A diet high in saturated fats relative to polyunsaturated fats increases neutrophil activation while lowering albumin levels—shifting the body toward a chronic pro-inflammatory state. Diets richer in polyunsaturated fats demonstrate the opposite pattern, signaling immune resolution and metabolic stability.
Mechanistic Insight: How Fat Ratios Reprogram Physiology
Unfavorable SFA:PUFA ratios were shown to drive mortality risk through several converging mechanisms:
Inflammatory signaling: Saturated fats activate Toll-like receptor pathways, while PUFAs—especially omega-3s—suppress inflammatory cascades and promote resolution
Mitochondrial efficiency: High SFA dominance impairs mitochondrial membranes and energy production, increasing cellular stress
Lipid mediator balance: PUFA-rich diets enable production of specialized pro-resolving mediators that actively terminate inflammation
Gut–immune interaction: Excess saturated fat promotes intestinal permeability and endotoxemia, amplifying systemic inflammation
Quantifying Risk: The Threshold That Matters
Mortality risk rose sharply when SFA intake exceeded PUFA intake by roughly 2:1 or more. In contrast, individuals maintaining ratios closer to 1:1 or 1:2 (SFA:PUFA) showed significantly lower mortality rates. This provides a practical, targetable dietary metric, rather than abstract nutritional advice.
Clinical Translation
The findings suggest that transitioning from a typical Western fat pattern (approximately 2.5:1 SFA: PUFA) to a Mediterranean-style pattern—by replacing butter and processed meats with olive oil, nuts, seeds, and fatty fish—could meaningfully reduce inflammation and mortality risk without requiring drastic caloric restriction.
Key Takeaway
Your lifespan is influenced not by how much fat you eat, but by which fats dominate your plate. The SFA:PUFA ratio directly shapes systemic inflammation through measurable immune markers, offering clinicians and individuals a powerful, evidence-based lever to improve long-term metabolic and cardiovascular outcomes.
Study 3: Metabolic Syndrome and Dietary Fat—A Systematic Review
This study shifts the focus from "fat as a fuel" to "fat as a metabolic regulator." By analyzing data across various populations, Julibert et al.(2019) identified that metabolic syndrome—a cluster of conditions including high blood pressure, high blood sugar, and excess body fat—is driven more by the quality of fat intake than the total percentage of fat in the diet.
Key Clinical Insights:
The SFA Threshold: High consumption of saturated fatty acids (SFAs) was consistently linked to increased waist circumference and elevated triglycerides, two hallmarks of metabolic syndrome.
The "Protective" Effect: Conversely, diets rich in unsaturated fats (MUFAs and PUFAs) acted as metabolic buffers, showing a strong inverse relationship with disease prevalence.
Quality over Calories: The researchers concluded that dietary interventions for metabolic health should prioritize fat composition rather than simple caloric restriction or low-fat mandates.
Study 4: The Mortality Risk Meta-Analysis—Big Picture Evidence
Mazidi and the International Lipid Expert Panel conducted an extensive meta-analysis involving over 1.16 million participants examining how different dietary fat types relate to all-cause mortality. This large-scale investigation provides robust evidence for fat type recommendations (Mazidi et al., 2020).
Key Takeaways:
Polyunsaturated fatty acid consumption shows consistent mortality benefits
Saturated fat excessive intake associates with increased mortality risk
Trans fats demonstrate the most harmful effects on longevity
Plant-based unsaturated fats provide greater protection than animal sources
The optimal dietary fat ratio remains a key target for disease prevention
Study 5: Diet-Induced Obesity and Glucolipid Dysfunction—Metabolic Complexity
Dutta and colleagues' 2025 paper in Diabetology & Metabolic Syndrome explores how dietary composition, particularly fat intake patterns, contributes to obesity development and glucose-lipid dysfunction in metabolic syndrome. Their work emphasizes the intricate connections between dietary fats and multiple metabolic pathways (Dutta et al., 2025).
Key Takeaways:
Diet-induced obesity involves complex interactions between fat types and metabolic regulation
Glucolipid metabolism dysfunction directly connects to inappropriate fatty acid ratios
Metabolic syndrome components respond differently to various dietary fat interventions
Understanding individual metabolic responses to fats is essential for personalized nutrition
Study 6: The Optimal Fat Balance—Practical Evidence from Animal Models
The research by Zhou et al.(2024) tested whether a specific balance of Saturated Fatty Acids (SFA), Monounsaturated Fatty Acids (MUFA), and Polyunsaturated Fatty Acids (PUFA) could outperform traditional dietary models in managing weight, lipids, and liver health.
Key Findings
MUFAs as the "Hero" Fat: The group consuming a diet high in monounsaturated fats (like those found in olive oil) showed the most significant improvements in metabolic markers.
Optimized Ratios: The study identified that a specific ratio—roughly 1:1.5:1 (SFA : MUFA: PUFA)—led to the best health outcomes in the subjects.
Metabolic Benefits: Rats on the optimized "Normal Fat" diet showed:
Lower systemic inflammation.
Improved lipid profiles (cholesterol and triglycerides).
Reduced fat accumulation in the liver (hepatic steatosis).
Better glucose regulation compared to both high-fat and poorly balanced normal-fat groups.
Why It Matters
The study provides mechanistic evidence that fat quality and balance are more important for preventing metabolic syndrome than simply cutting out fat. It reinforces the idea that monounsaturated fats serve as a "metabolic stabilizer" when consumed in the right proportion to other fats.
The "Takeaway" Ratio
While conducted on rats, the research aligns with the 2025 human data you mentioned earlier: don't fear fat; balance it. Specifically, increasing the proportion of MUFAs while keeping SFAs and PUFAs in a supporting role appears to be the "sweet spot" for metabolic longevity.
The Oxidation Warning: Why Heat Matters
Choosing the right fat is only half the battle; how you heat it determines whether it remains a "signal for health" or becomes a "signal for inflammation."
The PUFA Paradox: While polyunsaturated fats (PUFAs) like those in walnuts, seeds, and certain vegetable oils are highly beneficial for your heart and immune system, they are chemically fragile. Their multiple double bonds make them prone to oxidation when exposed to high heat.
The Danger of Smoke Points: When an oil is heated past its "smoke point," it undergoes a molecular breakdown, creating polar compounds and lipid peroxides. Consuming oxidised fats can counteract the very anti-inflammatory benefits you are trying to achieve.
The Clinical Kitchen Strategy:
High Heat (Searing/Roasting): Use oils with high Monounsaturated (MUFA) content and natural antioxidants, like Extra Virgin Olive Oil or Avocado Oil. Their single-bond structure is more resilient to heat.
Low to Medium Heat: Grass-fed butter or coconut oil (SFAs) are stable but should be used sparingly according to your target ratios.
No Heat (Dressing/Finishing): Reserve your high-PUFA oils (Flaxseed, Walnut, Hemp) strictly for cold use. Drizzle them over meals after cooking to preserve their delicate molecular structure and medicinal properties.
The Bottom Line: What Optimal Fat Intake Actually Looks Like
Based on comprehensive analysis of these seven rigorous studies, the evidence converges on several key principles for dietary fat and health:
Prioritize Fatty Acid Balance Over Total Fat Reduction
Rather than obsessing over total fat calories, focus on achieving appropriate SFA/MUFA/PUFA ratios. Research suggests roughly:
Saturated fats: 7-10% of total calories
Monounsaturated fats: 10-15% of total calories
Polyunsaturated fats: 5-10% of total calories (with emphasis on omega-3 sources)
Emphasize Plant-Based Unsaturated Fats
The evidence overwhelmingly supports dietary patterns emphasizing monounsaturated and polyunsaturated fatty acids from plant sources (nuts, seeds, olive oil, avocados) and fatty fish rich in omega-3 fatty acids.
Balance Your Omega-3 to Omega-6 Intake (N3:N6 Ratio)
An often overlooked aspect of dietary fat quality is the balance between omega-3 and omega-6 polyunsaturated fatty acids. Both are essential, yet modern Western diets typically provide a disproportionately high omega-6 intake, resulting in N6:N3 ratios commonly ranging from 15:1 to 20:1, compared with ranges of approximately 4:1 to 10:1 that are frequently associated with better metabolic and inflammatory profiles.
Why the N3:N6 Balance Matters
Omega-3 and omega-6 fatty acids share enzymatic pathways; imbalance can shift downstream signaling.
Adequate omega-3 intake (EPA and DHA from fish; ALA from plant sources) supports the production of anti-inflammatory and pro-resolving lipid mediators.
Several studies link higher omega-3 intake and lower relative omega-6 dominance with improved lipid profiles, insulin sensitivity, and inflammatory markers, including the neutrophil-to-albumin ratio.
Importantly, current evidence does not support eliminating omega-6 fats, which are essential and can be metabolically neutral or cardioprotective when consumed from whole-food sources.
Practical, Balanced Strategies
Prioritise omega-3 intake by consuming fatty fish (such as salmon, sardines, and mackerel), flaxseeds, chia seeds, and walnuts.
Avoid excess refined omega-6 sources: limit heavy reliance on industrial seed oils rich in linoleic acid (e.g., soybean, corn, sunflower oils).
Favour food quality over elimination: omega-6 fats from nuts, seeds, and minimally processed foods appear less problematic than those from refined oils.
Use olive oil as a primary culinary fat, emphasising monounsaturated fats rather than replacing all omega-6 sources.
Aim for regular fish intake (2–3 servings weekly) rather than aggressive omega-6 restriction.
Overall, optimizing the omega-3 to omega-6 balance should focus on increasing omega-3 intake and improving fat quality, rather than broadly reducing omega-6 fats. This nuanced approach aligns with current evidence and supports metabolic health without oversimplifying a complex and evolving area of lipid science.
Consider Biomarker Assessment
Emerging research suggests plasma metabolite testing and inflammatory markers (like the neutrophil-to-albumin ratio) may help determine whether your current fat intake pattern supports your metabolic health goals.
Frequently Asked Questions About Dietary Fats and Metabolic Health
Q: Should I completely eliminate saturated fats?
A: No. The research suggests moderate saturated fat intake (7-10% of calories) is acceptable when balanced with adequate unsaturated fats. The key is the overall ratio and total pattern, not complete elimination.
Q: Are all unsaturated fats equally beneficial?
A: Research indicates monounsaturated fatty acids and omega-3 polyunsaturated fats show the strongest health benefits, while some omega-6 polyunsaturated fats require careful balance. The N3:N6 ratio (omega-3 to omega-6 ratio) is particularly important—most people consume excessive omega-6 relative to omega-3, which promotes inflammation and metabolic dysfunction. Aiming for a 4:1 to 10:1 N6:N3 ratio rather than the typical 15:1 to 20:1 can significantly improve metabolic health outcomes.
Q: Can I get metabolic syndrome from eating too much healthy fat?
A: While unsaturated fats are healthier than saturated fats, excessive total caloric intake—including from healthy fats—can contribute to obesity and metabolic dysfunction. Portion control remains important.
Q: How quickly will changing my fat intake improve my metabolic health?
A: Research suggests meaningful changes in metabolic markers typically appear within 4-12 weeks of consistent dietary fat pattern modifications, though individual responses vary significantly.
Q: Should I avoid saturated fats from all sources equally?
A: Emerging evidence suggests the source matters. Saturated fats from whole food sources (like coconuts or grass-fed dairy) may have different effects than saturated fats from processed foods, though unsaturated fat sources remain preferable.
Q: What if I can't get accurate metabolic syndrome testing?
A: Start with basic dietary fat pattern optimization: reduce processed foods, increase plant-based unsaturated fats, and limit saturated fat sources. These foundational changes benefit most people regardless of specific testing.
Q: How do polyunsaturated fats prevent mortality risk increases?
A: Research suggests PUFAs reduce systemic inflammation (reflected in markers like the neutrophil percentage-to-albumin ratio), support healthy lipid profiles, and improve glucose metabolism—all protective against metabolic disease and premature mortality.
Ready to Optimize Your Metabolic Health Through Better Fat Choices?
The evolving science of dietary fats makes one message unmistakably clear: metabolic health is determined far more by fat quality and balance than by total fat reduction. Decades of low-fat dogma overlooked the reality that saturated, monounsaturated, and polyunsaturated fatty acids function as powerful biological signals, shaping inflammation, mitochondrial efficiency, immune regulation, and long-term disease risk. Contemporary evidence consistently demonstrates that unfavorable fatty acid ratios—particularly excess saturated fat relative to polyunsaturated fats—promote chronic inflammation and increase mortality risk, while diets rich in unsaturated fats support metabolic resilience and healthy aging.
Rather than eliminating fat, optimal nutrition focuses on achieving appropriate SFA/MUFA/PUFA and omega-3 to omega-6 balances. Monounsaturated fats emerge as metabolic stabilizers, polyunsaturated fats—especially omega-3s—act as inflammation-resolving agents, and moderate saturated fat intake appears acceptable when consumed within a balanced, whole-food matrix. Importantly, individual responses to dietary fats vary substantially, reinforcing the need to move beyond one-size-fits-all recommendations toward personalized, biomarker-guided strategies.
In practical terms, shifting from processed, saturated-fat-heavy foods toward olive oil, nuts, seeds, and fatty fish can meaningfully improve metabolic markers within weeks. The evidence no longer supports simplistic calorie or fat avoidance; instead, it calls for intentional selection of fats that align with human physiology. Ultimately, optimizing dietary fat composition represents one of the most powerful, achievable tools for reducing chronic disease risk and supporting long-term metabolic health.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Individual circumstances vary, and treatment decisions should always be made in consultation with qualified healthcare professionals.
Related Articles
What’s New in the 2025 Blood Pressure Guidelines? A Complete Scientific Breakdown | DR T S DIDWAL
Low-Fat vs. Low-Carb: Which Diet is Best for Weight Loss? | DR T S DIDWAL
Does Saturated Fat Cause Heart Disease? What the Latest Science Really Says | DR T S DIDWAL
5 Steps to Reverse Metabolic Syndrome: Diet, Habit, & Lifestyle Plan | DR T S DIDWAL
The Role of Cholesterol in Health and Disease: Beyond the "Bad" Label | DR T S DIDWAL
Lowering Cholesterol with Food: 4 Phases of Dietary Dyslipidemia Treatment | DR T S DIDWAL
High Triglyceride Levels: 5 New Facts to Help You Lower Your Risk | DR T S DIDWAL
References
Dutta, B., Tripathy, A., Archana, P. R., et al. (2025). Unraveling the complexities of diet induced obesity and glucolipid dysfunction in metabolic syndrome. Diabetology & Metabolic Syndrome, 17, 292. https://doi.org/10.1186/s13098-025-01837-y
Julibert, A., Bibiloni, M. M., & Tur, J. A. (2019). Dietary fat intake and metabolic syndrome risk: A systematic review. Nutrition, Metabolism and Cardiovascular Diseases, 29(9), 887–905. https://doi.org/10.1016/j.numecd.2019.05.004
Liu, J., Ren, J., Zhang, Y., Wang, X., Li, C., Wang, Z., & Zhao, L. (2024). Plasma signature metabolites of dietary fat intake and their associations with metabolic syndrome prevalence. Food & Function Today. https://doi.org/10.1002/fft2.505
Liu, Y., Wang, J., Chang, X., Ren, X., Wang, G., & Liu, J. (2025). Association between saturated and polyunsaturated fatty acid proportions in total fat intake and mortality risk: Mediation by the neutrophil percentage-to-albumin ratio. Lipids in Health and Disease, 24(1), 175. https://doi.org/10.1186/s12944-025-02592-9
Mazidi, M., Mikhailidis, D. P., Sattar, N., Toth, P. P., Judd, S., Blaha, M. J., Hernandez, A. V., Penson, P. E., Banach, M., & International Lipid Expert Panel (ILEP) & Lipid and Blood Pressure Meta-analysis Collaboration (LBPMC) Group. (2020). Association of types of dietary fats and all-cause and cause-specific mortality: A prospective cohort study and meta-analysis of prospective studies with 1,164,029 participants. Clinical Nutrition, 39(12), 3677–3686. https://doi.org/10.1016/j.clnu.2020.03.028
Szabó, É. (2025). Dietary fatty acids and metabolic health. Nutrients, 17(15), 2512. https://doi.org/10.3390/nu17152512
Zhou, Y., Yang, L., Chu, C., Chen, S., Yue, D., Hao, Y. J., Sun, G., & Xia, H. (2024). Normal fat intake with high monounsaturated fatty acid (MUFA) content and an appropriate SFA/MUFA/PUFA ratio improved the health of rats. European Journal of Lipid Science and Technology, 126(6), 2300214. https://doi.org/10.1002/ejlt.202300214