How Insulin Resistance Accelerates Cardiovascular Aging
Insulin resistance is a silent saboteur. Read the latest research on vascular stiffening, endothelial damage, and metabolic interventions to reverse heart aging.
DIABETES
Dr. T.S. Didwal, M.D.
11/27/202514 min read
Imagine your body's cells silently rejecting messages from your pancreas, like a phone that keeps dropping calls. This is insulin resistance—a condition that's become increasingly common, yet remains dangerously underrecognized as a driver of cardiovascular disease and premature aging. The connection between insulin resistance and heart health isn't just a minor health concern; it's a critical relationship that affects millions of people worldwide, often without their knowledge.
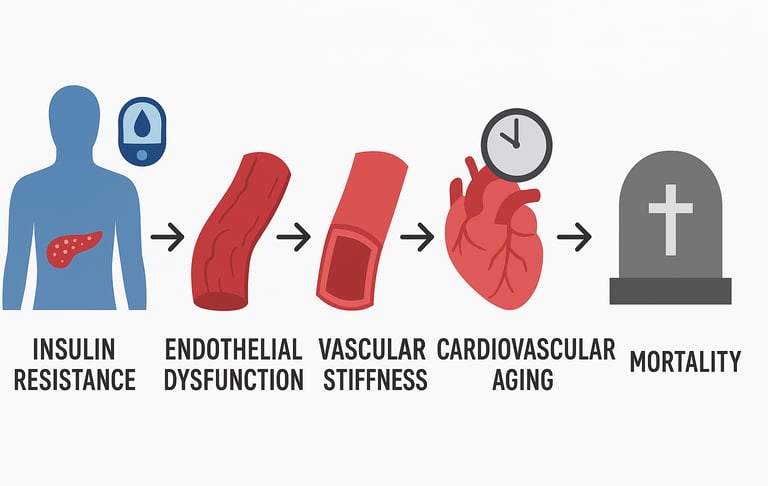
The relationship between metabolic dysfunction and cardiovascular aging has become a focal point of modern medical research. Recent studies reveal that insulin resistance doesn't simply increase your risk of diabetes—it fundamentally alters how your heart and blood vessels age, stiffens them prematurely, and sets the stage for life-threatening conditions (Hill et al., 2021). Understanding this connection could be the difference between a vibrant, healthy life and one shadowed by preventable cardiovascular disease.
In this comprehensive guide, we'll explore the cutting-edge science behind insulin resistance and cardiovascular aging, examine the latest research findings, and equip you with actionable insights to protect your heart health.
Clinical Pearls on Insulin Resistance & Cardiovascular Aging
1. Screen Beyond Glucose: Fasting Insulin and HOMA-IR
The Pearl: Do not rely solely on normal Fasting Plasma Glucose (FPG) or HbA1c to rule out significant cardiovascular risk. Insulin resistance (IR) often precedes Type 2 Diabetes by years, and patients are at high cardiovascular risk during this hyperinsulinemic, normoglycemic phase (Fazio et al., 2024).
Actionable Insight: Routinely request Fasting Insulin (FI) and calculate the HOMA-IR (Homeostasis Model Assessment-Insulin Resistance) index. A HOMA-IR > 2.0 or FI > 12 mIU/mL is a strong signal for aggressive lifestyle intervention, even if HbA1c is normal.
2. IR Drives Arterial Stiffening (Vascular Aging)
The Pearl: View insulin resistance not just as a metabolic problem, but as a primary driver of accelerated vascular aging (Hill et al., 2021). IR promotes collagen deposition and reduces NO (nitric oxide) availability, causing arterial stiffening.
Actionable Insight: Increased Arterial Stiffness (e.g., measured via Pulse Wave Velocity) in a non-diabetic patient should immediately trigger a deep investigation for underlying insulin resistance, as this stiffening is an early and often irreversible consequence.
3. The Bidirectional Risk: Age Multiplies IR's Impact
The Pearl: The relationship between aging and IR is synergistic (Hao et al., 2025). Advanced age not only makes the body more insulin-resistant but also dramatically amplifies the atherosclerotic consequences of existing IR
Actionable Insight: Early, aggressive intervention (especially lifestyle) in younger and middle-aged patients with IR is critical. Preventing metabolic dysfunction from becoming entrenched saves more years of cardiovascular health than intervening late.
4. Biological Aging is the Mediator (The Core Mechanism)
The Pearl: Insulin resistance doesn't just raise risk—it directly accelerates biological aging (Li et al., 2024), which is what ultimately drives CVD mortality. The mechanism involves mitochondrial dysfunction, cellular senescence, and impaired autophagy.
Actionable Insight: Interventions like Metformin and GLP-1 agonists are effective because they don't just lower glucose; they improve mitochondrial function and reduce cellular stress, effectively acting as "anti-aging" interventions that lower CVD risk.
5. Exercise is the Most Potent Insulin Sensitizer
The Pearl: Of all non-pharmacological interventions, physical activity is arguably the fastest and most powerful tool to reverse insulin resistance. It enhances glucose uptake in muscles independently of insulin, improving peripheral sensitivity immediately.
Actionable Insight: Prescribe a specific exercise regimen—not just general advice. Recommend a combination of 150 minutes/week of moderate-intensity aerobic exercise plus 2 sessions/week of resistance training. Resistance training is essential as it builds muscle mass, the primary site of glucose disposal.
Understanding Insulin Resistance: The Metabolic Foundation
Insulin resistance occurs when your cells don't respond effectively to insulin, the hormone responsible for regulating blood sugar levels. Rather than allowing glucose to enter cells for energy, your pancreas must produce increasingly higher amounts of insulin to achieve the same effect. This state of chronic hyperinsulinemia (elevated insulin levels) triggers a cascade of metabolic changes that extend far beyond blood sugar regulation.
The condition develops gradually, often without noticeable symptoms, making it what many researchers call a "silent metabolic saboteur." What makes insulin resistance particularly concerning is that it frequently coexists with other cardiovascular risk factors, including hypertension, dyslipidemia, and obesity—a dangerous cluster known as metabolic syndrome.
Recent research emphasizes that insulin resistance/hyperinsulinemia represents an important cardiovascular risk factor that has long been underestimated by both healthcare providers and the public (Fazio et al., 2024). This underestimation has led to delayed interventions and preventable cardiovascular complications in millions of patients worldwide.
The Mechanism: How Insulin Resistance Ages Your Cardiovascular System
The pathway from insulin resistance to cardiovascular aging is multifaceted and involves several interconnected mechanisms. When cells become resistant to insulin, a series of molecular events unfolds that directly impacts vascular health.
Vascular Stiffening and Structural Changes
One of the most significant consequences of insulin resistance is cardiovascular stiffening. Insulin-resistant states promote alterations in arterial wall composition, including increased collagen deposition and reduced elastin content. This leads to arterial stiffness, which impairs the natural elasticity of blood vessels and compromises their ability to respond to hemodynamic changes (Hill et al., 2021).
Cardiovascular stiffening represents a hallmark of cardiovascular aging, accelerating the aging process by years or even decades. The large arteries, particularly the aorta, become less compliant, forcing the heart to work harder to pump blood effectively. This increased workload contributes to left ventricular hypertrophy and eventually heart failure—a tragic but preventable outcome of chronic insulin resistance.
Endothelial Dysfunction and Inflammation
The endothelium—the delicate inner lining of blood vessels—is exquisitely sensitive to metabolic dysfunction. Insulin resistance impairs endothelial function by reducing nitric oxide availability, a critical signaling molecule that promotes vasodilation and prevents platelet aggregation. When nitric oxide levels drop, blood vessels become prone to vasoconstriction, thrombosis, and acceleration of atherosclerosis.
Simultaneously, insulin resistance activates systemic inflammatory pathways, increasing circulating levels of pro-inflammatory cytokines and adhesion molecules. This chronic inflammatory state accelerates plaque formation in arteries and promotes the development of unstable lesions vulnerable to rupture. The molecular landscape underlying these changes reveals complex interactions between insulin signaling dysfunction, mitochondrial disturbances, and inflammatory cascades that characterize aging-related cardiovascular disease .
Oxidative Stress and Mitochondrial Dysfunction
Insulin-resistant states generate excessive reactive oxygen species (ROS), leading to oxidative stress throughout the cardiovascular system. This oxidative burden damages mitochondrial function in endothelial cells and cardiomyocytes, impairing energy production and accelerating cellular senescence. The result is premature cardiovascular aging at the cellular and tissue levels.
Recent Research: Unveiling New Insights into Insulin Resistance and Heart Health
Study 1: Cardiovascular Stiffening and Disease Mechanisms
Research examining insulin resistance, cardiovascular stiffening and cardiovascular disease provides crucial mechanistic insights into how metabolic dysfunction translates to structural heart damage (Hill et al., 2021). This foundational work demonstrates that the hyperinsulinemic state triggers specific signaling cascades that promote vascular smooth muscle cell proliferation and increase extracellular matrix deposition. The study highlights that addressing insulin resistance early may prevent the irreversible cardiovascular stiffening that characterizes advanced cardiovascular disease.
By elucidating the molecular pathways connecting insulin resistance to arterial wall remodeling, this research establishes the biological plausibility for cardiovascular interventions targeting metabolic dysfunction at the earliest stages.
Key Takeaway: Early intervention targeting insulin resistance could prevent the vascular remodeling that leads to cardiovascular stiffening and premature cardiovascular disease.
Study 2: The Molecular and Metabolic Landscape
Contemporary research exploring the molecular and metabolic landscape of insulin resistance in aging-related cardiovascular diseases reveals the complexity of how metabolic dysfunction contributes to cardiovascular aging (2025). This investigation demonstrates that multiple molecular pathways—including those involving oxidative stress, mitochondrial dysfunction, and altered lipid metabolism—converge to accelerate cardiovascular aging in insulin-resistant individuals.
The research emphasizes that aging itself amplifies insulin resistance, creating a bidirectional relationship where advanced age promotes metabolic dysfunction, which in turn accelerates cardiovascular aging. This vicious cycle underscores why older adults with insulin resistance face exponentially higher cardiovascular risks. The aging process exacerbates insulin signaling defects at multiple levels, from impaired glucose transporter translocation to reduced mitochondrial oxidative capacity.
Key Takeaway: The relationship between aging and insulin resistance is bidirectional, with each condition amplifying the other's cardiovascular impact.
Study 3: Genome-Wide Discoveries and Therapeutic Targets
Multivariate genome-wide analyses of insulin resistance have unveiled novel genetic loci and therapeutic targets for cardiometabolic health (Ye et al., 2025). These discoveries identify specific molecular nodes that, when therapeutically targeted, could interrupt the pathways linking insulin resistance to cardiovascular disease. The research suggests that precision medicine approaches—tailored to individual genetic profiles—may offer superior outcomes compared to one-size-fits-all interventions.
Of particular significance, these studies identify metabolic signaling pathways and circulating biomarkers that predict which insulin-resistant individuals are at highest risk for developing severe cardiovascular complications. This knowledge enables risk stratification and personalized prevention strategies. The identification of novel therapeutic targets opens possibilities for developing pharmacological interventions that address the fundamental molecular underpinnings of insulin resistance.
Key Takeaway: Genetic research is identifying novel therapeutic targets that could more effectively interrupt the pathway from insulin resistance to cardiovascular disease.
Study 4: The Underestimated Cardiovascular Risk Factor
Recent literature emphasizes that insulin resistance/hyperinsulinemia: an important cardiovascular risk factor has been substantially underestimated in clinical practice (Fazio et al., 2024). Many patients with insulin resistance are never diagnosed because screening relies on glucose and hemoglobin A1c measurements that appear deceptively normal despite significantly elevated insulin levels.
This diagnostic gap has profound implications: patients receive no targeted interventions for the root metabolic problem, allowing insulin resistance to silently damage their cardiovascular system. By the time cardiovascular symptoms emerge, substantial vascular damage has already occurred. The recognition of insulin resistance as a primary cardiovascular risk factor necessitates a paradigm shift in clinical screening practices and diagnostic strategies.
Key Takeaway: Insulin resistance often goes undiagnosed because standard glucose-based screening misses the underlying metabolic dysfunction occurring at the insulin signaling level.
Study 5: Aging, Insulin Resistance, and Atherosclerosis
The relationship of ageing to insulin resistance and atherosclerosis has been systematically examined in recent research, revealing that advanced age significantly amplifies the atherosclerotic consequences of insulin resistance (Hao et al., 2025). Older adults with insulin resistance show accelerated plaque accumulation, increased plaque vulnerability, and higher rates of acute atherosclerotic events.
This research demonstrates that chronological age acts as a multiplicative risk factor for insulin-resistant individuals, not simply an additive one. The cardiovascular consequences compound dramatically in older adults, making early intervention in younger, insulin-resistant patients particularly critical for long-term cardiovascular health. The synergistic interaction between aging and insulin resistance in promoting atherosclerotic disease suggests that prevention strategies should focus on younger populations before metabolic dysfunction becomes entrenched.
Key Takeaway: Age amplifies the atherosclerotic consequences of insulin resistance, making early detection and intervention crucial in younger populations.
Study 6: Biological Aging as a Mediator
Groundbreaking research demonstrates that biological aging mediates the associations of metabolic score for insulin resistance with cardiovascular disease mortality (Li et al., 2024). This finding reveals that insulin resistance doesn't simply increase cardiovascular risk—it accelerates the biological aging process itself, which then drives cardiovascular disease development.
Using the metabolic score for insulin resistance (METS-IR) as a composite marker, this national cohort study found that individuals with elevated insulin resistance showed accelerated biological aging, manifested through multiple biomarkers of cellular senescence, mitochondrial dysfunction, and telomere shortening. This accelerated biological aging explained a substantial portion of the excess cardiovascular mortality observed in insulin-resistant populations. The mechanisms linking insulin resistance to accelerated aging include impaired autophagy, accumulation of senescent cells, and mitochondrial dysfunction—processes that cascade to promote cardiovascular disease development.
Key Takeaway: Insulin resistance accelerates biological aging, which directly translates to increased cardiovascular disease mortality and suggests that anti-aging interventions may also reduce cardiovascular disease risk.
The Cardiovascular Consequences: What Happens When Insulin Resistance Goes Untreated
Atherosclerosis and Plaque Formation
Insulin resistance creates a pro-atherosclerotic environment through multiple mechanisms. Elevated insulin levels directly stimulate vascular smooth muscle cell proliferation, promoting atherosclerotic plaque development (Hill et al., 2021). Additionally, insulin resistance impairs the clearance of atherogenic lipoproteins, allowing them to accumulate in arterial walls where they undergo oxidation and inflammatory processing.
The atherosclerotic plaques that develop in insulin-resistant individuals tend to be more lipid-rich, more inflammatory, and more unstable—characteristics associated with increased risk of acute plaque rupture and myocardial infarction. The interaction between insulin resistance and atherogenesis appears to be particularly problematic in aging populations, where multiple additional risk factors often coexist (Hao et al., 2025).
Hypertension and Left Ventricular Changes
Insulin resistance is intimately linked with hypertension development. Hyperinsulinemia increases sympathetic nervous system activation, promotes sodium retention by the kidneys, and induces endothelial dysfunction—all of which elevate blood pressure. The resulting hypertension, combined with cardiovascular stiffening from insulin resistance, promotes left ventricular hypertrophy and diastolic dysfunction.
Over time, these changes can progress to heart failure with preserved ejection fraction (HFpEF), a condition increasingly common in insulin-resistant populations and notoriously difficult to treat. The contribution of insulin resistance to heart failure development has become increasingly appreciated in recent years, with recognition that metabolic dysfunction represents a primary driver of HFpEF pathophysiology.
Thrombotic Complications
Insulin-resistant states promote a prothrombotic environment by increasing platelet reactivity, elevating procoagulant factors, and reducing anticoagulant mechanisms. This increased thrombotic tendency, combined with the plaque instability promoted by insulin resistance, substantially increases the risk of acute thrombotic events, including stroke and myocardial infarction.
Prevention and Management: Taking Control of Insulin Resistance
Dietary Approaches
Dietary modification represents the foundational intervention for insulin resistance. A Mediterranean-style diet rich in whole grains, legumes, fruits, vegetables, and healthy fats has demonstrated robust evidence for improving insulin sensitivity. The key is minimizing refined carbohydrates and added sugars while emphasizing whole, minimally processed foods.
Low-glycemic-index foods, high in fiber, help stabilize blood glucose levels and reduce the compensatory hyperinsulinemia that perpetuates insulin resistance. Research demonstrates that dietary changes can produce measurable improvements in metabolic dysfunction within weeks, with sustained improvements in cardiovascular outcomes following continued adherence (Fazio et al., 2024).
Physical Activity and Exercise
Regular physical activity represents one of the most powerful interventions for improving insulin sensitivity and reversing insulin resistance. Both aerobic exercise and resistance training enhance glucose uptake by muscles, reduce visceral adiposity, and improve endothelial function.
The evidence suggests that approximately 150 minutes of moderate-intensity aerobic activity weekly, combined with twice-weekly resistance training, produces substantial improvements in insulin resistance and cardiovascular risk markers. Exercise-induced improvements in insulin sensitivity occur through multiple mechanisms, including enhanced mitochondrial function and reduced inflammatory signaling.
Weight Management
For overweight and obese individuals, weight loss of 5-10% of body weight can significantly improve insulin sensitivity and reverse insulin resistance (Li et al., 2024). The benefit extends beyond simple caloric reduction—adipose tissue itself produces inflammatory cytokines and metabolic dysregulation, so reducing visceral adiposity directly addresses the root pathophysiology.
Studies demonstrate that relatively modest weight reductions can substantially attenuate the biological aging processes accelerated by insulin resistance, potentially translating to meaningful improvements in cardiovascular disease mortality (Li et al., 2024).
Medical Interventions
For individuals with established insulin resistance who haven't responded adequately to lifestyle modifications, pharmacological options exist. Metformin remains the first-line agent, improving insulin sensitivity through multiple mechanisms including AMPK activation and mitochondrial optimization.
Thiazolidinediones represent another option, though they carry metabolic side effects. GLP-1 receptor agonists, increasingly recognized for their pleiotropic cardiovascular benefits, improve insulin sensitivity while reducing body weight and providing direct cardioprotective effects. Recent evidence suggests that addressing insulin resistance pharmacologically can slow the acceleration of biological aging and reduce excess cardiovascular mortality in high-risk populations (Li et al., 2024).
Stress Management and Sleep
Chronic stress and sleep deprivation both impair insulin sensitivity and accelerate cardiovascular aging. Cortisol elevation from stress directly antagonizes insulin signaling, while poor sleep disrupts metabolic hormones and promotes inflammation.
Prioritizing 7-9 hours of quality sleep nightly and implementing stress-reduction techniques—such as meditation, yoga, or regular nature exposure—should be considered essential components of insulin resistance management. The relationship between sleep quality and metabolic dysfunction represents an underappreciated but critical dimension of cardiometabolic health.
Key Takeaways: What You Must Know
Insulin resistance is a silent metabolic saboteur (Fazio et al., 2024) that damages your cardiovascular system long before symptoms develop, making early detection and intervention critical.
Cardiovascular stiffening represents a hallmark consequence of insulin resistance (Hill et al., 2021), accelerating the aging of your heart and blood vessels by years or decades.
Insulin resistance has been substantially underestimated as a cardiovascular risk factor (Fazio et al., 2024), with many individuals never formally diagnosed despite harboring significant metabolic dysfunction.
The relationship between aging and insulin resistance is bidirectional and synergistic—advanced age amplifies the cardiovascular consequences of insulin resistance (Hao et al., 2025), while insulin resistance accelerates biological aging.
Biological aging appears to mediate much of the excess cardiovascular mortality associated with insulin resistance (Li et al., 2024), suggesting that interventions targeting aging mechanisms may reduce cardiovascular disease risk.
Novel genetic discoveries have identified specific therapeutic targets for interrupting the pathway from insulin resistance to cardiovascular disease (Ye et al., 2025), enabling precision medicine approaches.
Early intervention through lifestyle modification—particularly diet, exercise, and weight management—can reverse insulin resistance and prevent the vascular damage that leads to catastrophic cardiovascular events.
Frequently Asked Questions
Q: How do I know if I have insulin resistance?
A: Standard blood glucose and hemoglobin A1c tests often appear normal despite significant insulin resistance (Fazio et al., 2024). Ask your healthcare provider to measure fasting insulin levels (above 12 mIU/mL is concerning) or calculate the HOMA-IR index. Symptoms include unexplained fatigue, difficulty losing weight despite dieting, sugar cravings, and skin discoloration (acanthosis nigricans) around the neck and armpits.
Q: Can insulin resistance be reversed?
A: Yes. Lifestyle interventions—particularly caloric restriction combined with regular exercise—can substantially reverse insulin resistance, even in advanced cases. Studies show that 5-10% weight loss and regular physical activity can restore insulin sensitivity within weeks to months, with corresponding improvements in cardiovascular stiffening and arterial function.
Q: How long does it take for insulin resistance to damage my heart?
A: The timeline varies, but vascular damage begins within months to years of sustained insulin resistance. That's why early detection and intervention are so critical—reversing insulin resistance early can prevent years of cumulative cardiovascular damage. Research indicates that the relationship between insulin resistance and biological aging suggests that even relatively short durations of untreated metabolic dysfunction can initiate cellular aging cascades (Li et al., 2024).
Q: Is insulin resistance the same as type 2 diabetes?
A: No. Insulin resistance is the metabolic precursor to type 2 diabetes. You can have significant insulin resistance for years with normal glucose levels before progressing to diabetic glucose ranges. Identifying and treating insulin resistance early may prevent diabetes development entirely.
Q: What's the best diet for improving insulin sensitivity?
A: Mediterranean-style diets consistently show superior outcomes for improving insulin sensitivity (Fazio et al., 2024). Focus on whole grains, legumes, vegetables, fruits, healthy fats, and fish. Minimize refined carbohydrates, added sugars, and processed foods. Dietary interventions can produce measurable improvements in both insulin sensitivity and cardiovascular function markers.
Q: Can medications help with insulin resistance?
A: Yes. Metformin is the first-line agent, improving insulin sensitivity through multiple mechanisms. GLP-1 receptor agonists provide additional cardiovascular benefits beyond improving insulin sensitivity. Recent evidence demonstrates that pharmacological approaches to addressing insulin resistance can attenuate biological aging and reduce excess cardiovascular mortality (Li et al., 2024). Your healthcare provider can determine if medications are appropriate for your situation.
Call to Action: Protect Your Cardiovascular Future
The evidence is clear and compelling: insulin resistance represents a critical, often underrecognized threat to cardiovascular health and longevity. Research demonstrates that insulin resistance accelerates cardiovascular aging through multiple interconnected pathways, from cardiovascular stiffening (Hill et al., 2021) to accelerated biological aging (Li et al., 2024), ultimately driving excess cardiovascular mortality. But here's the encouraging news—this threat is largely preventable and reversible through early detection and intervention.
Don't wait for a heart attack or stroke to motivate change. Take these steps today:
Schedule a comprehensive metabolic assessment with your healthcare provider, specifically requesting fasting insulin measurement or HOMA-IR calculation—not just standard glucose testing. Early identification of insulin resistance is the critical first step toward prevention.
Evaluate your lifestyle honestly. Are you getting 150 minutes of weekly exercise? Are your meals primarily whole foods? Are you maintaining a healthy body weight? Identify specific areas for improvement. Research shows that relatively modest lifestyle interventions can produce dramatic improvements in insulin sensitivity and reverse insulin resistance.
Implement dietary changes immediately. Start incorporating more whole grains, legumes, vegetables, and healthy fats into your diet while minimizing refined carbohydrates and processed foods. Mediterranean-style dietary patterns show particular promise (Fazio et al., 2024).
Commit to regular physical activity. Whether you prefer walking, swimming, cycling, or resistance training, find activities you enjoy and commit to them consistently. Exercise represents one of the most effective interventions for reversing insulin resistance and preventing cardiovascular aging.
Share this knowledge with family members and friends who may be at risk for insulin resistance. Early detection can be lifesaving, particularly given the bidirectional relationship between aging and metabolic dysfunction (Hao et al., 2025).
Your cardiovascular system has a remarkable capacity to heal and regenerate when given the right conditions. By addressing insulin resistance now, you're investing in years of vibrant, healthy life ahead. The scientific evidence is unequivocal: intervening early to reverse insulin resistance can prevent cardiovascular stiffening, attenuate biological aging, and dramatically reduce your risk of premature cardiovascular disease. The choice, and the power to change, is entirely in your hands.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Individual circumstances vary, and treatment decisions should always be made in consultation with qualified healthcare professionals.
Related Articles
What’s New in the 2025 Blood Pressure Guidelines? A Complete Scientific Breakdown | DR T S DIDWAL
References
Fazio, S., Mercurio, V., Tibullo, L., Fazio, V., & Affuso, F. (2024). Insulin resistance/hyperinsulinemia: An important cardiovascular risk factor that has long been underestimated. Frontiers in Cardiovascular Medicine, 11, 1380506. https://doi.org/10.3389/fcvm.2024.1380506
Hao, X., Tu, S., Pan, D., Liao, W., Yang, L., Wang, S., & Sun, G. (2025). Relationship of ageing to insulin resistance and atherosclerosis. Metabolites, 15(9), 613. https://doi.org/10.3390/metabo15090613
Hill, M. A., Yang, Y., Zhang, L., Sun, Z., Jia, G., Parrish, A. R., & Sowers, J. R. (2021). Insulin resistance, cardiovascular stiffening and cardiovascular disease. Metabolism: Clinical and Experimental, 119, 154766. https://doi.org/10.1016/j.metabol.2021.154766
Li, X., Wang, J., Zhang, M., Li, X., Fan, Y., Zhou, X., Sun, Y., & Qiu, Z. (2024). Biological aging mediates the associations of metabolic score for insulin resistance with all-cause and cardiovascular disease mortality among US adults: A nationwide cohort study. Diabetes, Obesity & Metabolism, 26(9), 3552–3564. https://doi.org/10.1111/dom.15694
The Molecular and Metabolic landscape of Insulin Resistance in Aging-Related Cardiovascular Diseases. (2025). Aging and Disease. https://doi.org/10.14336/ad.2025.1108
Ye, C., Dou, C., Liu, D., et al. (2025). Multivariate genome-wide analyses of insulin resistance unravel novel loci and therapeutic targets for cardiometabolic health. Nature Communications, 16, 10057. https://doi.org/10.1038/s41467-025-64985-9