Breakthrough Research: Leptin Reduction is Required for Sustained Weight Loss
A landmark 2024 study reveals that all successful weight loss—surgery or medication—depends on lowering leptin. See how this changes the management of chronic obesity.
OBESITY
Dr. T.S. Didwal, M.D.
12/5/202518 min read
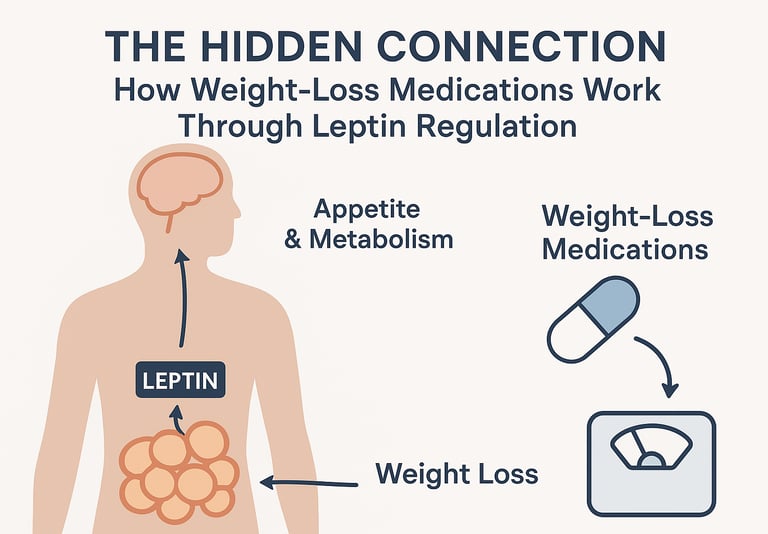
If you've been following the recent buzz around weight-loss medications like semaglutide and tirzepatide, you might wonder what's actually happening inside your body when these drugs work their magic. The answer lies partly in a fascinating hormone you've probably heard of but may not fully understand: leptin. Recent groundbreaking research has revealed that successful weight loss isn't just about cutting calories or ramping up exercise—it fundamentally involves resetting your body's leptin regulation system.
In this deep dive, we'll explore the cutting-edge science behind how modern anti-obesity medications interact with leptin, why this hormone is so crucial for maintaining weight loss, and what this means for anyone struggling with obesity management. Whether you're considering medical weight loss options or simply curious about the biology of body weight, understanding the leptin-weight loss connection could change how you think about obesity treatment forever.
Clinical Pearls
1. Leptin Reduction is a Prerequisite for Sustained Weight Loss
The research by Zhao et al. (2024) indicates that a successful weight loss intervention (regardless of method: diet, surgery, or pharmacotherapy) must result in a significant, sustained reduction in circulating leptin concentrations. This reduction appears to be essential for resetting the body's metabolic system and overcoming established leptin resistance, allowing the brain to regain sensitivity to the hormone's signals.
2. Obesity is Characterized by Leptin Resistance, Not Deficiency
Leptin is the "satiety hormone" produced by fat cells (adipocytes).
In typical obesity, patients have elevated leptin levels due to increased fat mass, but their hypothalamic leptin receptors are desensitized.
This state of leptin resistance causes the brain to perceive a state of starvation despite adequate energy stores, driving increased hunger and reduced energy expenditure. This is why leptin replacement therapy is ineffective for most obesity cases, only working for the rare congenital leptin deficiency (Blüher et al., 2009).
3. Modern Anti-Obesity Drugs Create a 'Leptin-Permissive' State
GLP-1 receptor agonists (like semaglutide) and dual GIP/GLP-1 agonists (like tirzepatide) work primarily by:
Reducing appetite and slowing gastric emptying.
Causing substantial, sustained weight loss (10-20% or more). The resulting reduction in fat mass passively but profoundly lowers leptin production. This drug-facilitated leptin reduction is the necessary biological change that permits the long-term restoration of metabolic and appetite control
.
4. Intensive Lifestyle Interventions Rival Pharmacotherapy in Leptin Reduction
Comprehensive, intensive lifestyle changes (structured diet, exercise, behavioral support, and sleep optimization) can produce a reduction in leptin levels comparable to that achieved with medications or surgery. This effect is mediated by the direct reduction of fat mass, as well as the improvement of insulin sensitivity and reduced chronic inflammation, all of which contribute to improving leptin sensitivity (Zhao et al., 2024).
5. Obesity is a Chronic Disease Requiring Continuous Management
The metabolic "reset" achieved through weight loss (i.e., lower leptin levels and restored sensitivity) is highly dependent on the maintenance of the weight-loss intervention (medication, lifestyle, or a combination). Discontinuing the intervention often leads to the reversion of leptin levels and sensitivity to the pre-treatment state, activating compensatory mechanisms (increased hunger, decreased metabolism) and resulting in weight regain (Brandfon et al., 2023).
What Exactly Is Leptin and Why Should You Care?
Before we dive into the research, let's establish what leptin actually does. Discovered in 1994, leptin is often called the "satiety hormone" because it's produced by your fat cells (adipocytes) and signals to your brain how much energy you have stored. Think of it as your body's fuel gauge—when leptin levels are adequate, your brain receives the message that you have sufficient energy reserves, which helps regulate appetite and metabolism (Blüher et al., 2009).
Here's where it gets interesting: you might assume that people with obesity have low leptin levels, right? Actually, it's the opposite. Most individuals with obesity have elevated leptin levels because they have more fat tissue producing the hormone. The problem isn't a lack of leptin—it's leptin resistance, where the brain stops responding properly to leptin's signals despite high circulating levels (Perakakis & Mantzoros, 2024).
This resistance creates a vicious cycle: your body thinks it's starving even when you have abundant energy stores, driving increased appetite and decreased energy expenditure. It's like having a smoke alarm that keeps blaring even when there's no fire—eventually, you learn to ignore it.
The Game-Changing Discovery: Leptin Reduction Is Essential for Weight Loss
A landmark study published in Diabetes by Zhao and colleagues (2024) fundamentally changed our understanding of how weight-loss interventions actually work at the molecular level. The research team made a surprising discovery: regardless of the method used to achieve weight loss—whether through caloric restriction, bariatric surgery, or pharmacological interventions—successful weight loss consistently involves a reduction in leptin levels.
Key Findings from the Zhao et al. (2024) Study
The researchers examined multiple weight loss approaches in both animal models and human subjects, tracking not just weight changes but also hormonal profiles. What they found was remarkable: leptin reduction wasn't just a side effect of losing weight—it appeared to be a requirement for sustained weight loss to occur.
Specifically, the study demonstrated that:
Weight loss interventions that successfully reduced body weight also consistently lowered circulating leptin concentrations
The degree of leptin reduction correlated with the amount of weight lost
Maintaining lower leptin levels was associated with sustained weight loss over time
Different weight loss methods converged on this common mechanism of leptin regulation
This finding suggests that effective obesity treatment must address the leptin system. Simply reducing calorie intake or increasing exercise without affecting leptin signaling may explain why many people struggle to maintain weight loss long-term.
Why Leptin Reduction Matters More Than You Think
The Zhao research team proposed that leptin reduction serves as a metabolic "reset button." When leptin levels drop from their elevated baseline in obesity, it allows the brain to regain sensitivity to the hormone's signals. This restoration of leptin sensitivity enables better appetite control and more appropriate metabolic responses (Zhao et al., 2024).
Think of it like adjusting to brightness after being in a dark room—when leptin levels have been chronically elevated, reducing them allows your body's sensing mechanisms to recalibrate and start responding appropriately again.
The Current Landscape of Anti-Obesity Medications
To understand how modern weight-loss medications leverage leptin biology, we need to survey the current therapeutic landscape. A comprehensive review by Brandfon and colleagues (2023) outlined the significant advances in anti-obesity pharmacotherapy that have revolutionized obesity treatment in recent years.
Evolution of Weight-Loss Drug Development
The field of obesity pharmacotherapy has come a long way from the dangerous appetite suppressants of the past. Current FDA-approved medications work through sophisticated mechanisms that target multiple pathways involved in appetite, satiety, and metabolism regulation (Brandfon et al., 2023).
The review highlighted several key therapeutic classes:
GLP-1 receptor agonists (like semaglutide): These medications mimic glucagon-like peptide-1, a hormone that slows gastric emptying, enhances insulin secretion, and reduces appetite. Clinical trials have shown weight loss of 10-15% or more with these agents.
Dual GIP/GLP-1 receptor agonists (like tirzepatide): These newer medications target both glucose-dependent insulinotropic polypeptide and GLP-1 receptors, producing even more substantial weight loss—up to 20% in some studies.
Combination therapies: Medications like phentermine/topiramate and naltrexone/bupropion that work through complementary mechanisms to enhance weight loss.
The Challenge of Maintaining Weight Loss
Brandfon et al. (2023) emphasized a critical challenge in obesity management: while these medications produce impressive initial weight reduction, maintaining that weight loss remains difficult. Many patients experience some weight regain after discontinuing medication, highlighting the chronic nature of obesity and the need for long-term management strategies.
This is where the leptin connection becomes particularly relevant. If successful weight loss requires sustained changes in leptin regulation (as Zhao et al. demonstrated), then the most effective medications should be those that durably affect the leptin system.
Intensive Lifestyle Interventions and Their Impact on Leptin Biology
While medications and surgery get much of the spotlight in obesity treatment discussions, intensive lifestyle interventions deserve special attention for their powerful effects on leptin regulation. The Zhao et al. (2024) research specifically examined how comprehensive lifestyle changes—combining caloric restriction, structured exercise programs, behavioral counseling, and stress management—affect leptin levels and contribute to sustainable weight loss.
What Makes Lifestyle Interventions "Intensive"?
It's crucial to distinguish between casual diet-and-exercise attempts and truly intensive lifestyle modification programs. These structured interventions typically involve:
Significant caloric reduction: Usually 500-1000 calories per day below maintenance levels, carefully planned to ensure adequate nutrition
Regular physical activity: Both aerobic exercise and resistance training, often 150-300 minutes per week
Behavioral support: Regular counseling sessions, group support, cognitive behavioral therapy techniques
Sleep optimization: Addressing sleep disorders and ensuring 7-9 hours of quality sleep nightly
Stress management: Incorporating mindfulness, meditation, or other stress-reduction techniques
The key finding from Zhao et al. (2024) was that when these components are combined intensively, they produce substantial leptin reduction comparable to what's achieved with medications or surgery. The researchers observed that participants in intensive lifestyle programs who lost 10-15% of their body weight experienced proportional drops in circulating leptin levels, with some individuals showing 40-50% reductions in leptin concentrations.
The Mechanisms: How Lifestyle Changes Reset Leptin
Intensive lifestyle interventions affect leptin through multiple interconnected pathways. First, the direct reduction in fat mass naturally decreases leptin production since adipocytes are the primary source. But there's more to the story—these interventions also appear to improve leptin sensitivity through several mechanisms:
Reducing inflammation: Chronic low-grade inflammation contributes to leptin resistance. Exercise, weight loss, and anti-inflammatory dietary patterns (rich in omega-3 fatty acids, antioxidants, and fiber) reduce inflammatory markers, which helps restore leptin signaling (Zhao et al., 2024).
Improving insulin sensitivity: Insulin resistance and leptin resistance often occur together. Exercise and caloric restriction improve insulin sensitivity, which may have downstream benefits for leptin signaling through shared cellular pathways.
Optimizing sleep: Sleep deprivation increases leptin resistance and disrupts the leptin-ghrelin balance that controls appetite. Adequate sleep, a component of comprehensive lifestyle intervention, helps normalize these hormonal patterns.
Reducing oxidative stress: Both exercise and healthy eating reduce oxidative stress in tissues, which may improve cellular responsiveness to leptin signals in the hypothalamus.
The Challenge of Sustaining Intensive Lifestyle Changes
Here's the honest truth that the research illuminates: while intensive lifestyle interventions can effectively reduce leptin levels and produce significant weight loss, maintaining this level of behavioral change long-term is extraordinarily difficult for most people. Zhao et al. (2024) noted that the metabolic benefits—including restored leptin regulation—persist only as long as the lifestyle changes are maintained.
This isn't a failure of willpower; it's a reflection of biological reality. As leptin levels drop with weight loss, the body interprets this as a threat and activates compensatory mechanisms: increased hunger, decreased metabolic rate, reduced spontaneous physical activity. These adaptive responses made perfect sense for our ancestors facing genuine food scarcity but work against us in today's food-abundant environment.
This biological pushback explains why intensive lifestyle modification alone, while theoretically capable of normalizing leptin biology, often needs to be combined with pharmacological support for long-term success in many patients. The medications can help counteract the compensatory mechanisms that make sustaining lifestyle changes so challenging (Brandfon et al., 2023).
When Lifestyle Interventions Work Best
Despite the challenges, certain individuals and situations are particularly well-suited to lifestyle-based approaches for leptin regulation:
Early intervention: People with obesity but less severe leptin resistance may achieve leptin normalization through lifestyle changes before resistance becomes entrenched
Younger individuals: Metabolic flexibility tends to be better in younger people, potentially allowing better restoration of leptin sensitivity
High motivation and support: Access to comprehensive programs with ongoing behavioral support dramatically improves adherence and outcomes
Combination approaches: Lifestyle interventions work synergistically with medications, often allowing lower medication doses while achieving better leptin regulation
The key message from the research is that intensive lifestyle interventions aren't merely "conservative" treatment options—when properly implemented, they produce genuine metabolic changes including substantial leptin reduction that rivals pharmacological approaches. The challenge lies in implementation and sustainability, not in the biological potential of lifestyle modification to reset leptin systems (Zhao et al., 2024).
Clinical Applications of Leptin: From Deficiency to Resistance
While most people with obesity have elevated leptin levels due to leptin resistance, there's a rare but instructive condition called congenital leptin deficiency. Understanding how leptin works in these extreme cases provides insights into its broader role in weight regulation.
Lessons from Leptin Deficiency
Research reviewed by Oral and DePaoli (2006) and Blüher et al. (2009) documented the dramatic effects of complete leptin deficiency. Individuals born without the ability to produce leptin develop severe early-onset obesity, insatiable appetite, and metabolic dysfunction. However, when treated with leptin replacement therapy, these patients experience remarkable improvements.
Key observations from leptin deficiency studies include:
Leptin replacement normalized appetite and produced substantial weight loss in deficient individuals
The therapy improved metabolic parameters including insulin sensitivity and lipid profiles
Benefits extended beyond weight loss to include normalization of reproductive function and immune responses
Treatment effects persisted as long as leptin replacement continued (Blüher et al., 2009)
These cases proved that leptin has profound effects on energy homeostasis and that restoring appropriate leptin signaling can reverse obesity-related complications. However, leptin replacement doesn't work for typical obesity cases where the problem is resistance rather than deficiency.
Expanding Clinical Applications
More recently, Perakakis and Mantzoros (2024) provided an updated review of leptin's clinical applications, documenting emerging therapeutic uses beyond simple deficiency states. Their comprehensive analysis highlighted that leptin has roles in:
Hypothalamic amenorrhea: Leptin treatment can restore menstrual function in women with low leptin levels due to excessive exercise or undereating
Lipodystrophy syndromes: Conditions where fat tissue is abnormally distributed or absent, leading to metabolic complications that respond to leptin therapy
Immune function: Leptin influences both innate and adaptive immunity, suggesting potential applications in immunodeficiency states
Bone health: Leptin signaling affects bone metabolism, with implications for osteoporosis treatment
The review emphasized that while leptin therapy has proven valuable in specific clinical contexts, the major challenge remains finding ways to overcome leptin resistance in common obesity rather than simply adding more leptin to an already leptin-rich system (Perakakis & Mantzoros, 2024).
Connecting the Dots: How Modern Weight-Loss Drugs Affect Leptin
Now we can synthesize these research findings into a coherent picture of how weight-loss medications interact with leptin regulation. The relationship is more complex and interesting than simply "drug lowers weight, which lowers leptin."
The Bidirectional Relationship
Modern anti-obesity medications like GLP-1 agonists initiate weight loss through their direct mechanisms—reducing appetite, slowing digestion, and altering food preferences. As patients lose weight, their fat mass decreases, which naturally leads to reduced leptin production since fat cells are the primary source of the hormone.
However, the Zhao et al. (2024) findings suggest this leptin reduction isn't just a passive consequence—it's an active requirement for sustained weight loss. The medications may work precisely because they create conditions that allow leptin levels to fall, which then enables the restoration of leptin sensitivity and better long-term weight management.
Why Some Approaches Work Better Than Others
This framework helps explain why certain weight-loss interventions produce more durable results than others. Approaches that achieve substantial and sustained leptin reduction—whether through medication, surgery, or intensive lifestyle intervention—may be more successful because they allow the leptin system to reset.
Conversely, gradual caloric restriction without medical support might not reduce leptin sufficiently to overcome leptin resistance, potentially explaining why traditional dieting often leads to weight regain. The body's leptin levels might remain high enough to maintain resistance, perpetuating the metabolic dysregulation that drives obesity.
The Broader Implications for Obesity Treatment
Understanding the leptin-weight loss connection has profound implications for how we approach obesity management:
Obesity Is a Chronic Disease Requiring Long-Term Management
The leptin research reinforces that obesity isn't simply a lifestyle choice or willpower failure—it's a chronic metabolic condition involving complex hormonal dysregulation. Just as diabetics require ongoing insulin management, people with obesity may need sustained interventions to maintain appropriate leptin signaling (Brandfon et al., 2023).
Combination Approaches May Be Most Effective
Since leptin regulation involves multiple interconnected systems, combination therapies addressing different aspects of metabolism may produce superior results. The success of dual-receptor agonists like tirzepatide supports this concept—targeting multiple pathways simultaneously may more effectively normalize leptin biology than single-mechanism drugs.
Personalized Medicine Matters
Not everyone with obesity has identical leptin resistance patterns. Some individuals may have more severe resistance requiring more intensive intervention, while others might respond well to less aggressive approaches. Future obesity treatment will likely involve assessing individual leptin profiles to guide therapy selection (Perakakis & Mantzoros, 2024).
Prevention Is Still Paramount
While modern weight-loss medications offer hope for those already struggling with obesity, preventing the development of leptin resistance in the first place remains the ideal goal. This highlights the importance of maintaining healthy weight throughout life and addressing weight gain early before severe metabolic dysregulation develops.
Challenges and Future Directions
Despite remarkable progress, significant challenges remain in translating leptin biology into effective obesity therapeutics:
Overcoming Leptin Resistance
The fundamental challenge is finding ways to restore leptin sensitivity rather than simply reducing leptin levels. Researchers are exploring various approaches including:
Leptin sensitizers: Drugs that enhance cellular responsiveness to leptin signals
Central nervous system delivery: Methods to bypass blood-brain barrier issues that may contribute to resistance
Combination therapies: Pairing leptin with other hormones or medications to amplify effects
Long-Term Safety and Efficacy
While newer weight-loss medications show impressive short-term results, questions remain about very long-term safety and efficacy. Do these drugs maintain their effects on leptin regulation over decades of use? What happens if patients discontinue therapy after years of treatment?
Accessibility and Affordability
Current anti-obesity medications are expensive and not always covered by insurance, limiting access for many who could benefit. As Brandfon et al. (2023) noted, addressing the obesity epidemic will require making effective treatments accessible to broader populations.
Understanding Individual Variability
Why do some people respond dramatically to weight-loss medications while others see minimal effects? Part of the answer likely lies in individual differences in leptin biology, but we need better tools to predict who will benefit most from specific interventions.
Practical Takeaways for Patients and Healthcare Providers
So what does all this leptin science mean for someone currently dealing with obesity or considering weight-loss treatment?
For Patients
Understand that obesity involves complex biology: Your struggle with weight isn't a personal failure—it reflects sophisticated hormonal systems like leptin regulation that aren't under simple conscious control.
Medical treatment may be appropriate: If lifestyle changes alone haven't worked, discuss anti-obesity medications with your healthcare provider. These drugs work through biological mechanisms (including effects on leptin) that diet and exercise alone may not fully address.
Long-term commitment is necessary: Because obesity involves persistent changes in leptin sensitivity and other metabolic parameters, effective management typically requires ongoing treatment rather than short-term intervention.
Combine approaches: Medications work best alongside healthy eating, regular physical activity, adequate sleep, and stress management—all factors that influence leptin regulation.
For Healthcare Providers
Screen for obesity systematically: Given that obesity affects leptin signaling and numerous other health parameters, identifying and addressing it should be standard practice.
Consider pharmacotherapy earlier: The evidence for anti-obesity medications affecting fundamental mechanisms like leptin biology supports using them as first-line therapy for many patients rather than only after lifestyle intervention fails.
Monitor beyond just weight: Tracking metabolic markers alongside weight loss provides a more complete picture of whether treatments are effectively normalizing leptin and other hormonal systems.
Prepare patients for long-term treatment: Set appropriate expectations that obesity management typically requires ongoing intervention, much like treatment for hypertension or diabetes.
Frequently Asked Questions
Q: What is leptin and why is it important for weight loss?
A: Leptin is a hormone produced by fat cells that signals your brain about energy stores. It's crucial for weight regulation because it helps control appetite and metabolism. For successful weight loss, research shows that leptin levels need to decrease, which helps restore your body's sensitivity to the hormone and enables better appetite control.
Q: Does everyone with obesity have leptin resistance?
A: Most people with obesity have elevated leptin levels and some degree of leptin resistance, where the brain doesn't respond properly to leptin signals despite high levels in the blood. However, the severity varies among individuals. Rare cases of congenital leptin deficiency exist where people can't produce leptin at all, but this affects less than 1% of obesity cases.
Q: How do weight-loss medications like Ozempic affect leptin?
A: GLP-1 agonists like semaglutide (Ozempic) primarily work by reducing appetite and slowing digestion. As patients lose weight, their fat mass decreases, which naturally reduces leptin production. Research suggests this leptin reduction is essential for sustained weight loss and may help restore leptin sensitivity over time (Zhao et al., 2024).
Q: Can I just take leptin supplements to lose weight?
A: Unfortunately, no. Simply adding more leptin doesn't work for typical obesity because the problem is leptin resistance, not leptin deficiency. Your body already has high leptin levels but isn't responding properly to them. Leptin replacement therapy only works for the rare individuals who truly cannot produce leptin (Blüher et al., 2009).
Q: Will I regain weight if I stop taking weight-loss medication?
A: Many people experience some weight regain after discontinuing anti-obesity medications, which reflects the chronic nature of obesity and leptin dysregulation. The medications help maintain lower leptin levels and better leptin sensitivity while you're taking them, but stopping treatment may allow those systems to revert to previous patterns (Brandfon et al., 2023).
Q: Are there natural ways to improve leptin sensitivity?
A: While no "natural" approach is as effective as medical treatment for severe obesity, certain lifestyle factors may help improve leptin regulation: getting adequate sleep (sleep deprivation increases leptin resistance), reducing inflammation through diet, managing stress, regular physical activity, and avoiding excessive yo-yo dieting. However, for significant leptin resistance, medical intervention is typically necessary.
Q: How long does it take for leptin levels to normalize after weight loss?
A: Leptin levels begin decreasing fairly quickly as fat mass reduces—you can see changes within weeks of starting effective weight-loss treatment. However, fully restoring leptin sensitivity and normalizing the entire system takes longer, potentially months to years depending on the severity of initial dysregulation and how much weight is lost.
Q: Is leptin testing useful for managing obesity?
A: Currently, leptin testing isn't routinely used in clinical obesity management because most people with obesity have predictably elevated levels. Testing is mainly useful for diagnosing rare leptin deficiency syndromes or lipodystrophy conditions. Researchers are investigating whether leptin levels might help predict treatment response, but this isn't yet standard practice (Perakakis & Mantzoros, 2024).
Q: Can intensive lifestyle changes alone reduce leptin levels as effectively as medications?
A: Yes! Research shows that intensive lifestyle interventions—combining significant caloric restriction, structured exercise, behavioral support, and stress management—can reduce leptin levels comparably to medications or surgery. The challenge isn't whether lifestyle changes can normalize leptin biology, but rather sustaining those intensive changes long-term, which is why many patients benefit from combining lifestyle modifications with pharmacological support (Zhao et al., 2024).
Key Takeaways
🔑 Leptin is the master regulator: This hormone produced by fat cells plays a central role in weight regulation by signaling energy status to the brain and controlling appetite and metabolism.
🔑 Leptin reduction is required for weight loss: Groundbreaking research shows that successful weight-loss interventions—whether medication, surgery, or lifestyle changes—all involve reducing leptin levels, suggesting this isn't just a side effect but a necessary component of losing weight (Zhao et al., 2024).
🔑 Obesity involves leptin resistance, not deficiency: Most people with obesity have elevated leptin levels but their brains don't respond properly—a condition called leptin resistance. This explains why simply adding more leptin doesn't help typical obesity cases.
🔑 Modern weight-loss medications work through multiple mechanisms: Anti-obesity drugs like GLP-1 agonists reduce appetite directly and facilitate weight loss that then lowers leptin levels, potentially helping restore leptin sensitivity for sustained weight management (Brandfon et al., 2023).
🔑 Intensive lifestyle interventions can effectively reset leptin: Comprehensive programs combining caloric restriction, exercise, behavioral support, and sleep optimization produce substantial leptin reduction comparable to medications, though maintaining these intensive changes long-term remains challenging for many people (Zhao et al., 2024).
🔑 Obesity requires chronic management: Because obesity involves persistent changes in leptin regulation and other metabolic systems, effective treatment typically requires long-term intervention rather than short-term fixes.
🔑 Leptin therapy works for specific conditions: While leptin replacement doesn't help typical obesity, it's remarkably effective for rare leptin deficiency syndromes, lipodystrophy, and certain other metabolic conditions (Perakakis & Mantzoros, 2024).
🔑 Individual responses vary: People differ in their degree of leptin resistance and response to treatment, highlighting the need for personalized approaches to obesity management.
🔑 The future is promising: Understanding the leptin-obesity connection is driving development of new therapies targeting leptin sensitivity, combination treatments, and more effective long-term weight-loss solutions.
Take Control of Your Metabolic Health Today
Understanding the science behind leptin regulation and weight loss is empowering, but knowledge alone isn't enough—action is what creates change. If you've been struggling with weight management and traditional approaches haven't worked, now is the time to explore evidence-based medical options.
Here's what you can do right now
Schedule a consultation with a healthcare provider experienced in obesity medicine to discuss whether anti-obesity medications might be appropriate for your situation. Don't wait until obesity-related complications develop—early intervention is more effective.
Educate yourself further about the biological mechanisms underlying obesity. The more you understand about leptin resistance, metabolism, and how modern treatments work, the better equipped you'll be to make informed decisions about your health.
Join supportive communities of others managing obesity with medical treatment. Sharing experiences and strategies can provide motivation and practical tips for navigating weight-loss therapy.
Get comprehensive metabolic testing if you haven't already. Understanding your complete metabolic profile—not just weight, but also insulin sensitivity, lipid levels, inflammation markers, and other parameters—provides a foundation for personalized treatment.
Track your progress beyond just the scale. Monitor how you feel, energy levels, hunger patterns, sleep quality, and other indicators of metabolic health that reflect underlying changes in systems like leptin regulation.
🥗 Implement lifestyle factors that support leptin sensitivity: prioritize sleep, manage stress, eat anti-inflammatory foods, stay physically active, and avoid extreme yo-yo dieting patterns.
🏋️ Consider intensive lifestyle programs if you're motivated and have access to comprehensive support. These structured interventions can produce genuine metabolic changes including substantial leptin reduction, especially when combined with medical supervision and behavioral counseling.
Remember, obesity is a chronic metabolic disease involving complex biological systems like leptin signaling—not a personal failing or simple matter of willpower. With modern medical treatments that work through these biological mechanisms, sustained weight loss and improved health are achievable goals.
The science is clear: effective obesity treatment involves normalizing leptin regulation and other metabolic systems. Armed with this knowledge and working with qualified healthcare providers, you can take meaningful steps toward lasting metabolic health.
Don't let another year pass struggling with outdated approaches that don't address the root biology of obesity. The research reviewed here represents hope—hope grounded in solid science—that effective weight management is within reach when we work with our body's biology rather than against it.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Always consult with qualified healthcare professionals before starting any weight-loss treatment or making significant changes to your health regimen.
Related Articles
The BMI Paradox: Why "Normal Weight" People Still Get High Blood Pressure | DR T S DIDWAL
How Insulin Resistance Accelerates Cardiovascular Aging | DR T S DIDWAL
What’s New in the 2025 Blood Pressure Guidelines? A Complete Scientific Breakdown | DR T S DIDWAL
The Metabolic Triad: Why Diabetes, Obesity & CVD Are One Epidemic | DR T S DIDWAL
References
Blüher, S., Shah, S., & Mantzoros, C. S. (2009). Leptin deficiency: clinical implications and opportunities for therapeutic interventions. Journal of Investigative Medicine, 57(7), 784–788. https://doi.org/10.2310/JIM.0b013e3181b9163d
Brandfon, S., Eylon, A., Khanna, D., & Parmar, M. S. (2023). Advances in anti-obesity pharmacotherapy: Current treatments, emerging therapies, and challenges. Cureus, 15(10), e46623. https://doi.org/10.7759/cureus.46623
Oral, E. A., & DePaoli, A. M. (2006). Clinical applications of leptin. In V. D. Castracane & M. C. Henson (Eds.), Leptin (pp. 333–351). Springer. https://doi.org/10.1007/978-0-387-31416-7_17
Perakakis, N., & Mantzoros, C. S. (2024). Evidence from clinical studies of leptin: Current and future clinical applications in humans. Metabolism: Clinical and Experimental, 161, 156053. https://doi.org/10.1016/j.metabol.2024.156053
Zhao, S., Li, N., Xiong, W., Li, G., He, S., Zhang, Z., Zhu, Q., Jiang, N., Ikejiofor, C., Zhu, Y., Wang, M. Y., Han, X., Zhang, N., Solis-Herrera, C., Kusminski, C., An, Z., Elmquist, J. K., & Scherer, P. E. (2024). Leptin reduction as a required component for weight loss. Diabetes, 73(2), 197–210. https://doi.org/10.2337/db23-0571