When Your Nervous System Meets Your Waistline: The Science of Resensitizing Your Fat Burners
Your weight loss signals might be blocked! We explain how exercise and stress management restore the sensitivity of beta-adrenergic receptors, turning your fat cells into energy burners.
OBESITY
Dr. T.S. Didwal, M.D.
11/30/202515 min read
How Your Adrenergic System Controls Fat Storage and Obesity
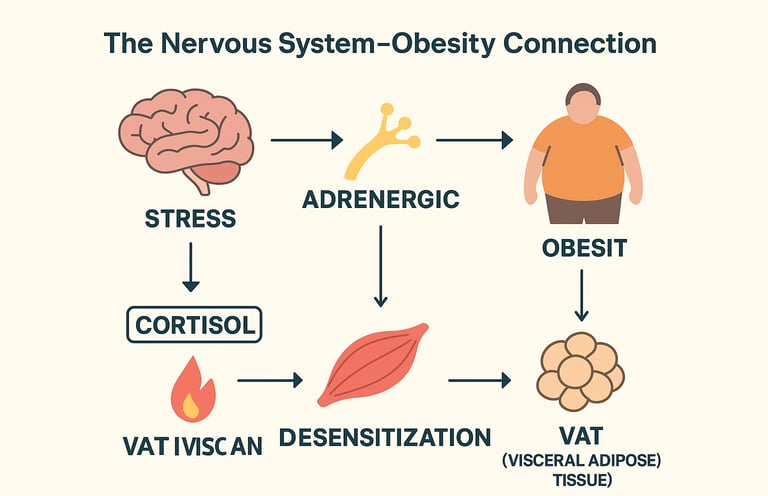
Have you ever noticed how stress seems to pack pounds around your midsection, or how some people seem naturally energized to burn calories while others struggle? The answer might lie in a sophisticated biological communication system that most of us have never heard of: the adrenergic system. This intricate network of nerves and hormones plays a far more significant role in body weight regulation than traditional diet-focused approaches might suggest.
The adrenergic system and obesity connection represents one of the most compelling frontiers in metabolic science. Unlike the simplistic "calories in, calories out" model, this relationship reveals how your nervous system, hormones, and fat tissue engage in constant dialogue to determine whether your body stores or burns energy. Understanding this interplay isn't just academically interesting—it could fundamentally change how you approach weight management and metabolic health.
This comprehensive guide explores the cutting-edge research connecting the sympathetic nervous system, beta-adrenergic receptor activation, and obesity mechanisms. We'll translate complex neurobiology into actionable insights you can apply to your life, while examining the latest scientific evidence that challenges conventional wisdom about weight loss
Clinical Pearls
1. Stress Doesn't Just Affect Willpower—It Rewires Fat Storage
The Science: Chronic psychological stress and the resulting elevation of the hormone cortisol (via the HPA axis) fundamentally alters your body's metabolic environment. Cortisol paradoxically promotes the accumulation of visceral fat (belly fat), even when your "fight or flight" system is active (Lengton et al., 2024).
The Pearl: Weight gain around your midsection isn't just about diet; it's a stress response. Focusing on stress management and HPA axis recovery (not just calorie restriction) is a non-negotiable step for reducing metabolically harmful belly fat.
2. Your Fat Cells Need a Strong Nerve Signal
The Science: Your fat tissue is not passive; it is directly connected to and regulated by your nervous system (adipose tissue innervation). When you have chronic obesity or inflammation, your fat tissue can lose this crucial nerve connection (denervation), leading to dysfunction and a reduced ability to burn energy (Shi et al., 2025).
The Pearl: To make your fat cells responsive to signals to burn energy, you need to restore nerve function. Consistent aerobic exercise directly stimulates the sympathetic nervous system, helping to reconnect and repair this vital metabolic machinery.
3. Yoga Is an Evidence-Based Metabolic Intervention
The Science: Structured yoga-based interventions are effective because they simultaneously target multiple dysfunctions. They reduce inflammation (metaflammation), lower cortisol, and restore the autonomic nervous system balance (parasympathetic tone), leading to favorable shifts in metabolic hormones like adiponectin (Chobe et al., 2023; Sarvottam & Yadav, 2014).
The Pearl: Yoga is more than relaxation; it's medicine for your metabolism. It systematically addresses the stress-inflammation-dysfunction cycle at the root of weight gain, making it an essential, evidence-based part of a weight management plan.
4. Your Body Needs to Respond to the "Burn" Signal
The Science: The beta-adrenergic receptors on your fat cells are the "locks" that open to hormonal signals (catecholamines) that trigger fat burning (lipolysis). In chronic stress or obesity, these locks become desensitized, meaning your body stops responding effectively to the signals to expend energy (Araújo et al., 2025).
The Pearl: It's not just about producing fat-burning signals; it's about your body hearing them. Regular exercise is crucial for resensitizing these receptors, ensuring that when your body signals the need to burn fat, your cells listen.
5. Sustainable Weight Loss Requires System Integration
The Science: Effective obesity management must address the interconnectedness of four systems: the Adrenergic System, the HPA Axis (Stress), Adipose Tissue Innervation, and Inflammation (Araújo et al., 2025). Single-pathway interventions (like diet alone) often fail because they don't fix the underlying nervous and hormonal dysregulation.
The Pearl: Think of your metabolism as a complex ecosystem. You need an integrated approach that combines exercise (to fix adrenergic function), stress management (to fix the HPA axis), and anti-inflammatory nutrition (to fix metaflammation).
What Is the Adrenergic System, and Why Should You Care?
Before diving into the obesity connection, let's establish what the adrenergic system actually is. Your body contains two complementary nervous system divisions: the sympathetic (your "fight or flight" system) and the parasympathetic (your "rest and digest" system). The adrenergic system operates through the sympathetic nervous system, using chemical messengers called catecholamines—primarily norepinephrine and epinephrine (adrenaline).
These powerful molecules don't just prepare you for danger. They're constantly regulating fundamental metabolic processes like thermogenesis (heat production), lipolysis (fat breakdown), and glucose metabolism. When your adrenergic system functions optimally, it promotes fat oxidation and energy expenditure. When it becomes dysregulated—a condition increasingly common in modern life—it can contribute to metabolic dysfunction and weight gain.
The key players in this system are specialized proteins called adrenergic receptors, found on virtually every cell type. Among these, β-adrenergic receptors (beta-adrenergic receptors) deserve special attention because of their profound influence on obesity pathophysiology. When these receptors receive signals from catecholamines, they trigger the cascade of events that leads to efficient energy expenditure and brown adipose tissue activation.
The Adrenergic System as a Master Regulator of Metabolism
How Beta-Adrenergic Receptors Control Fat Metabolism
The relationship between β-adrenergic receptor signaling and obesity begins at the cellular level (Araújo et al., 2025). These receptors function like locks that open when catecholamines arrive as keys. Once activated, β-adrenergic receptors trigger an intracellular cascade that increases cellular energy expenditure and promotes lipolysis—the breakdown of stored fat into usable fuel.
What makes this particularly fascinating is the specificity of different receptor subtypes (Ranganathan & Robinson, 2023). β3-adrenergic receptors, predominantly found in brown adipose tissue and classical white fat, are especially important for thermogenesis and metabolic rate elevation. When properly stimulated, these receptors can essentially reprogram fat cells from storage depots into metabolic furnaces.
The implications for obesity treatment are substantial. Individuals who maintain robust adrenergic signaling tend to have higher basal metabolic rates and greater capacity for weight regulation. Conversely, the sympathetic nervous system dysfunction observed in many obese individuals represents a fundamental impairment in this crucial metabolic control system (Araújo et al., 2025).
Stress, the HPA Axis, and Metabolic Complications
Your body doesn't experience stress in isolation. The hypothalamic-pituitary-adrenal (HPA) axis, working in concert with the adrenergic system, orchestrates your entire stress response. During acute stress, this creates a coordinated response: norepinephrine and epinephrine surge to mobilize energy, while cortisol (a glucocorticoid hormone) rises to maintain blood glucose availability.
Here's where the problem emerges for many people: chronic stress dysregulates this finely tuned system (Lengton et al., 2024). The research reveals that persistent activation of the stress-obesity connection creates a vicious cycle. Elevated cortisol levels from chronic psychological stress paradoxically promote central adiposity (belly fat) despite overall sympathetic nervous system activation. This occurs through multiple mechanisms, including increased cortisol-mediated visceral fat deposition and impaired glucose metabolism regulation .
The interaction between glucocorticoids and the adrenergic system explains why some stressed individuals develop severe metabolic dysfunction despite increased circulating catecholamines. The simultaneous elevation of stress hormones can overwhelm the system's compensatory mechanisms, leading to a state of adrenergic receptor desensitization where cells stop responding effectively to catecholamine signals .
Adipose Tissue Innervation: The Nervous System's Direct Pipeline to Fat Storage
One of the most exciting recent developments in obesity research concerns the adipose tissue innervation—the direct nerve connections between the sympathetic nervous system and fat cells (Shi et al., 2025). Your fat tissue isn't passive; it's actively innervated by sympathetic nerve fibers that regulate its metabolic activity.
The Neural Architecture of Fat
Within visceral and subcutaneous adipose tissue, sympathetic nerve terminals form intimate connections with adipocytes (fat cells) (Shi et al., 2025). These nerves release norepinephrine, which binds to adrenergic receptors on fat cell surfaces, triggering lipolysis and promoting thermogenesis in specialized fat depots. The density and functionality of this innervation varies significantly between individuals and can be influenced by factors including obesity history, physical activity, and metabolic health status.
Recent evidence demonstrates that the innervation pattern of adipose tissue profoundly influences metabolic fate (Shi et al., 2025). Well-innervated brown adipose tissue generates tremendous heat through a process called non-shivering thermogenesis, while under-innervated or dysfunctional tissue fails to respond appropriately to sympathetic signals, leading to energy accumulation rather than expenditure.
Metaflammation and Innervation Dysfunction
An exciting avenue of research reveals the cross-regulation between adipose tissue innervation and metaflammation (chronic, low-grade inflammation associated with obesity) (Shi et al., 2025). When adipose tissue becomes dysfunctional and inflamed, it simultaneously loses proper sympathetic innervation. This creates a self-perpetuating problem: without adequate nerve signaling, fat tissue becomes more susceptible to inflammatory activation, which further impairs innervation.
The inflammation-innervation link represents a crucial therapeutic target (Shi et al., 2025). As research progresses, interventions designed to restore proper adipose tissue innervation and simultaneously reduce obesity-related inflammation may prove more effective than single-pathway approaches.
Current Research: What the Latest Studies Reveal
A Comprehensive Systematic Review of the Adrenergic-Obesity Connection
Recent systematic analysis has consolidated our understanding of how the adrenergic system and obesity interconnect across multiple biological pathways (Araújo et al., 2025). A 2025 systematic review synthesizing current evidence demonstrates that adrenergic dysfunction contributes to obesity development through at least three major mechanisms: impaired thermogenic capacity, dysregulated glucose homeostasis, and altered adipokine secretion patterns .
The research emphasizes that effective obesity management must address not just dietary intake but also the restoration of proper sympathetic nervous system function . Individuals demonstrating robust β-adrenergic receptor signaling and appropriate sympathetic activation consistently show better long-term weight management outcomes compared to those with blunted adrenergic responsiveness.
Key Takeaway The systematic review synthesizes evidence showing that adrenergic system dysfunction operates through multiple distinct pathways, all contributing to obesity development. This multi-mechanism understanding suggests that single-intervention approaches may have limited effectiveness, supporting the case for integrated, systems-based obesity treatment strategies targeting sympathetic nervous system restoration, thermogenic capacity enhancement, and metabolic hormone optimization.
The Stress-Obesity Nexus: HPA Axis Regulation and Metabolic Consequences
Understanding the glucocorticoid-adrenergic interaction proves essential for comprehending the stress-obesity connection (Lengton et al., 2024). Comprehensive analysis of the biological, physiological, and behavioral dimensions of this relationship reveals that chronic psychological stress and resulting HPA axis dysregulation create a metabolic environment favoring fat accumulation, particularly in visceral depots . The mechanism involves multiple pathways: direct glucocorticoid-mediated changes in fat cell gene expression, altered appetite regulation through hypothalamic signaling, and impaired sympathetic responsiveness to metabolic challenges .
The research indicates that interventions addressing stress management and HPA axis recovery should form integral components of comprehensive obesity treatment protocols . Individuals with optimal stress resilience and healthy cortisol rhythm patterns demonstrate superior metabolic flexibility and more favorable weight regulation outcomes.
Key Takeaway : This comprehensive overview reveals that the stress-obesity connection functions through coordinated dysregulation of both the HPA axis and adrenergic system. Chronic stress doesn't merely increase appetite or reduce willpower—it fundamentally alters how fat cells respond to hormonal signals and accumulate energy. The research underscores that stress management interventions represent not optional wellness activities but essential components of evidence-based obesity treatment, equal in importance to dietary and exercise modifications.
Adipose Tissue Innervation as a Therapeutic Frontier
Recent investigation into the cross-regulation between adipose tissue innervation and metaflammation highlights innervation restoration as a potential therapeutic target (Shi et al., 2025). The research identifies that sympathetic denervation of adipose tissue creates conditions favoring local inflammation and metabolic dysfunction. Conversely, improved adrenergic signaling and maintained tissue innervation support anti-inflammatory responses and sustained thermogenic capacity.
This understanding suggests that interventions promoting sympathetic nervous system activation and maintaining adipose tissue innervation—whether through targeted pharmaceutical approaches, behavioral modifications, or lifestyle interventions—represent promising directions for obesity prevention and management
Key Takeaway : The discovery of cross-regulation between adipose tissue innervation and metaflammation opens new therapeutic possibilities. Rather than viewing obesity-related inflammation and sympathetic nervous system dysfunction as separate problems, this research reveals they're interconnected aspects of a single pathological process. Therapeutic strategies that simultaneously address both components—restoring nerve function while reducing inflammation—may prove more effective than interventions targeting only one pathway.
Beta-Adrenergic Receptors: Recent Mechanistic Insights
Current research continues to elucidate how β-adrenergic receptor activation generates heat and energy expenditure even in the face of obesity's many complications (Ranganathan & Robinson, 2023). The evidence indicates that maintaining functional β3-adrenergic signaling in brown adipose tissue remains central to effective metabolic rate elevation and sustainable weight management Additionally, novel insights into receptor heterogeneity reveal that β1-adrenergic and β2-adrenergic receptors may play underappreciated roles in maintaining overall metabolic health through cardiac and pulmonary effects that indirectly support systemic energy expenditure .
Key Takeaway : The emerging mechanistic understanding of β-adrenergic receptor function challenges oversimplified models of thermogenesis. Different receptor subtypes operate in distinct tissues and generate their thermogenic effects through multiple pathways. This complexity has important implications for pharmaceutical obesity treatment development, suggesting that effective drugs will need to target specific receptor subtypes in specific tissues rather than producing uniform adrenergic system activation.
Lifestyle Interventions: Restoring Adrenergic Function Through Behavioral Change
Physical Activity and Sympathetic Nervous System Restoration
Among all behavioral interventions, aerobic exercise stands out for its profound capacity to restore adrenergic function. Regular cardiovascular activity directly stimulates sympathetic nervous system tone, promotes adrenergic receptor sensitivity, and increases the volume and functionality of brown adipose tissue. These adaptations translate directly into improved baseline metabolic rate and enhanced fat oxidation capacity during and after exercise.
Research demonstrates that individuals maintaining regular exercise programs show markedly improved sympathetic responsiveness compared to sedentary populations. This isn't merely about calorie burning; exercise literally restores the biological machinery underlying effective weight regulation.
Stress Management and HPA Axis Recovery
Given the profound impact of chronic stress on metabolic dysfunction, intentional stress management becomes a critical component of any obesity intervention strategy (Lengton et al., 2024). Techniques that reliably reduce psychological stress while simultaneously promoting parasympathetic activation—creating better balance in the autonomic nervous system—deserve special attention.
Yoga-Based Interventions: Integrating Mind and Metabolism
An intriguing body of evidence supports yoga-based lifestyle interventions for obesity management. Research indicates that structured yoga programs produce multifaceted effects on the systems governing weight regulation (Sarvottam & Yadav, 2014). Beyond the obvious caloric expenditure from physical movement, yoga appears to work through several interconnected pathways.
First, regular yoga practice reduces obesity-related inflammation by lowering circulating levels of pro-inflammatory cytokines (Sarvottam & Yadav, 2014). Simultaneously, yoga reduces cortisol levels and improves HPA axis function, directly addressing the stress-obesity connection. The parasympathetic activation induced by yoga—particularly through practices emphasizing controlled breathing—helps restore autonomic nervous system balance.
Evidence examining adipokine levels among overweight and obese individuals demonstrates that structured yoga interventions produce favorable shifts in hormone profiles associated with metabolic health (Chobe et al., 2023). Individuals participating in regular yoga programs show improvements in adiponectin levels (a protective adipokine) and reductions in inflammatory markers, suggesting that this practice addresses multiple aspects of obesity pathophysiology simultaneously.
Key Takeaway: This research demonstrates that yoga-based lifestyle interventions produce significant reductions in obesity-related inflammation and cardiovascular disease risk. The mechanism extends beyond simple physical activity to encompass direct effects on the hypothalamic-pituitary axis, inflammatory pathways, and autonomic nervous system balance. These findings legitimize yoga as an evidence-based component of comprehensive obesity management rather than merely a relaxation technique.
Key Takeaway: The systematic review of yoga's effects on adipokine levels reveals that structured yoga interventions produce measurable improvements in endocrine function related to metabolic regulation. Particularly significant is the elevation of adiponectin, a hormone with well-documented protective effects against metabolic syndrome and cardiovascular disease. The consistency of these findings across multiple studies suggests yoga addresses fundamental aspects of obesity pathophysiology through hormone regulation.
The mechanism likely involves yoga's effects on both the nervous system (through vagal tone enhancement and stress hormone reduction) and direct effects on adipose tissue metabolism. This makes yoga-based interventions particularly attractive for individuals seeking holistic obesity management approaches that address biological, physiological, and psychological dimensions simultaneously.
Integration of Mechanisms: How Everything Works Together
The research reveals a sophisticated interconnected system where adrenergic function, HPA axis regulation, adipose tissue innervation, and inflammatory processes don't operate in isolation (Araújo et al., 2025). Rather, dysfunction in one component perpetuates problems in others, while improvements in any single pathway create cascading benefits across the entire system.
Consider a typical scenario: chronic psychological stress dysregulates the HPA axis, elevating cortisol. This elevated cortisol impairs sympathetic responsiveness and promotes visceral fat deposition. The dysfunctional visceral fat develops impaired innervation and becomes chronically inflamed. This inflammation further reduces adrenergic signaling effectiveness, creating a self-perpetuating cycle of metabolic dysfunction (Lengton et al., 2024; Shi et al., 2025).
Conversely, interventions addressing this system recognize these interconnections. Exercise simultaneously restores sympathetic nervous system function, improves HPA axis regulation, and reduces inflammatory markers. Yoga-based practices address stress-driven HPA axis dysregulation while promoting parasympathetic balance and reducing circulating inflammatory cytokines (Sarvottam & Yadav, 2014; Chobe et al., 2023). The cumulative effect of multiple interventions targeting different aspects of this system produces outcomes superior to single-intervention approaches.
Key Takeaways: What You Need to Know
The Adrenergic System Controls Metabolism (Araújo et al., 2025): Your sympathetic nervous system and β-adrenergic receptors represent a master control system for energy expenditure, fat breakdown, and thermogenesis. Maintaining optimal adrenergic function is fundamental to effective weight regulation.
Stress Dysregulates the System (Lengton et al., 2024): Chronic psychological stress creates paradoxical effects through the HPA axis, promoting fat storage despite elevated catecholamines. This stress-obesity connection represents a crucial but often overlooked factor in metabolic health.
Your Fat Tissue Is Innervated (Shi et al., 2025): Direct nerve connections from your sympathetic nervous system to your adipose tissue regulate fat cell metabolism. Loss of proper innervation contributes to metabolic dysfunction and correlates with obesity-related inflammation.
Inflammation and Innervation Interact (Shi et al., 2025): The cross-regulation between adipose tissue innervation and metaflammation creates a self-perpetuating cycle that contributes to obesity progression. Addressing both aspects simultaneously proves more effective than single-pathway interventions.
Lifestyle Interventions Restore Function (Sarvottam & Yadav, 2014; Chobe et al., 2023): Regular physical activity, stress management, and particularly yoga-based interventions directly restore adrenergic function and improve HPA axis regulation, creating sustained improvements in metabolic health and weight management.
Multiple Pathways Require Integration (Araújo et al., 2025): Effective obesity treatment addresses sympathetic nervous system function, HPA axis balance, adipose tissue innervation, and inflammation reduction simultaneously through integrated lifestyle medicine approaches.
Frequently Asked Questions
Q: Can I improve my adrenergic system function through lifestyle changes alone?
A: Yes, absolutely. Regular physical activity, adequate sleep, stress management, and structured practices like yoga all directly enhance sympathetic nervous system function and β-adrenergic receptor sensitivity. While some individuals may benefit from pharmacological support, lifestyle modifications represent the first-line intervention for restoring adrenergic function (Araújo et al., 2025).
Q: How does yoga specifically help with obesity beyond just burning calories?
A: Yoga interventions work through multiple interconnected pathways: reducing stress hormones and HPA axis dysregulation, decreasing obesity-related inflammation, improving adipokine profiles, and restoring autonomic nervous system balance (Sarvottam & Yadav, 2014; Chobe et al., 2023). Research shows improvements in metabolic markers that extend far beyond simple caloric expenditure.
Q: Is visceral fat more responsive to adrenergic stimulation than subcutaneous fat?
A: Research indicates that visceral adipose tissue generally shows differential innervation patterns and metabolic responsiveness compared to subcutaneous fat (Shi et al., 2025). The stress-obesity connection particularly affects visceral fat deposition, making this depot especially problematic. However, both depots respond positively to improved adrenergic function through exercise and stress management.
Q: Can I have a "broken" adrenergic system?
A: Adrenergic dysfunction occurs along a spectrum rather than as an all-or-nothing condition (Araújo et al., 2025). Chronic obesity, sustained psychological stress, and prolonged sedentary behavior can all contribute to receptor desensitization and reduced sympathetic responsiveness. The encouraging news is that this remains largely reversible through lifestyle intervention.
Q: How long does it take to restore adrenergic function?
A: Some improvements occur within weeks of consistent exercise and stress management. More substantial restoration of β-adrenergic receptor sensitivity and sympathetic nervous system function typically requires 8-12 weeks of sustained behavior change. The process continues improving over months and years with ongoing healthy practices.
Q: What's the connection between cortisol and belly fat?
A: Cortisol, while necessary for survival, promotes visceral fat deposition through multiple mechanisms including altered glucose metabolism, increased insulin sensitivity in fat cells, and impaired sympathetic responsiveness in this depot (Lengton et al., 2024). Chronic stress and resulting HPA axis dysregulation create conditions favoring abdominal weight gain despite overall sympathetic activation.
The Path Forward: Integrating Systems Biology Into Practice
Understanding the adrenergic system and obesity connection transforms how we approach weight management. Rather than viewing obesity as a simple matter of willpower or caloric arithmetic, we recognize it as a complex systems problem involving nervous system function, hormonal regulation, tissue-level innervation, and inflammatory processes (Araújo et al., 2025).
This systems perspective suggests that the most effective obesity interventions will address multiple pathways simultaneously (Araújo et al., 2025). A truly comprehensive approach combines regular physical activity (which directly stimulates sympathetic nervous system function and β-adrenergic signaling), evidence-based stress management (particularly yoga-based interventions that restore HPA axis balance) (Sarvottam & Yadav, 2014), sleep optimization (essential for autonomic recovery), and anti-inflammatory dietary patterns.
The science reveals what many have intuitively understood: lasting weight management requires addressing not just what you eat, but how your nervous system functions, how you handle stress, and whether your body's metabolic machinery remains responsive to the signals designed to burn energy rather than store it.
Ready to Restore Your Metabolic Health?
The evidence is clear: your adrenergic system holds tremendous untapped potential for weight management and metabolic optimization. Rather than pursuing another restrictive diet or expensive supplement, consider whether your sympathetic nervous system might benefit from restoration through evidence-based lifestyle interventions.
Start small: Commit to three sessions of moderate aerobic activity weekly. Explore yoga practices specifically designed to enhance stress resilience and metabolic health. Prioritize sleep and stress management. Monitor how your body responds as your adrenergic system gradually recovers its natural capacity for energy expenditure and metabolic regulation.
The biology of your body—honed through millions of years of evolution to efficiently manage energy—remains on your side. All that's required is understanding how to work with these ancient systems rather than against them.
Your journey toward sustainable metabolic health starts with recognizing that your nervous system, not just your willpower, holds the key to lasting weight management.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Individual circumstances vary, and treatment decisions should always be made in consultation with qualified healthcare professionals.
Related Articles
The BMI Paradox: Why "Normal Weight" People Still Get High Blood Pressure | DR T S DIDWAL
How Insulin Resistance Accelerates Cardiovascular Aging | DR T S DIDWAL
References
Araújo, B., Leite, F., & Ribeiro, L. (2025). The interplay between the adrenergic system and obesity: a systematic review. International Journal of Obesity, 49(12), 2426–2445. https://doi.org/10.1038/s41366-025-01924-0
Chobe, M. P., Nanjundaiah, R. M., Chobe, S., & Raghuram, N. (2023). Effect of yoga on adipokine levels among overweight and obese people: A systematic review. Journal of Ayurveda and Integrative Medicine, 14(6), 100813. https://doi.org/10.1016/j.jaim.2023.100813
Lengton, R., Schoenmakers, M., Penninx, B. W. J. H., Boon, M. R., & Van Rossum, E. F. C. (2024). Glucocorticoids and HPA axis regulation in the stress–obesity connection: A comprehensive overview of biological, physiological and behavioural dimensions. Clinical Obesity, 15(2), e12725. https://doi.org/10.1111/cob.12725
Ranganathan, S., & Robinson, E. L. (2023). β-adrenergic receptors feel the heat against obesity. Nature Reviews Endocrinology, 19, 621. https://doi.org/10.1038/s41574-023-00889-2
Sarvottam, K., & Yadav, R. K. (2014). Obesity-related inflammation & cardiovascular disease: efficacy of a yoga-based lifestyle intervention. The Indian journal of medical research, 139(6), 822–834.
Shi, W., Tan, H., Liao, C., & An, Z. (2025). Cross-regulation between adipose tissue innervation and metaflammation: a potential therapeutic target for obesity. American Journal of Translational Research, 17(6), 4087–4100. https://doi.org/10.62347/AIWS5429