Tired of Daily Insulin Injections? What Once-Weekly Insulin Means for Type 2 Diabetes Care
Managing type 2 diabetes may soon mean just one injection a week. Discover how once-weekly insulin compares with daily shots and how it can improve adherence and quality of life.
DIABETES
Dr. T.S. Didwal, M.D.(Internal Medicine)
1/25/202610 min read
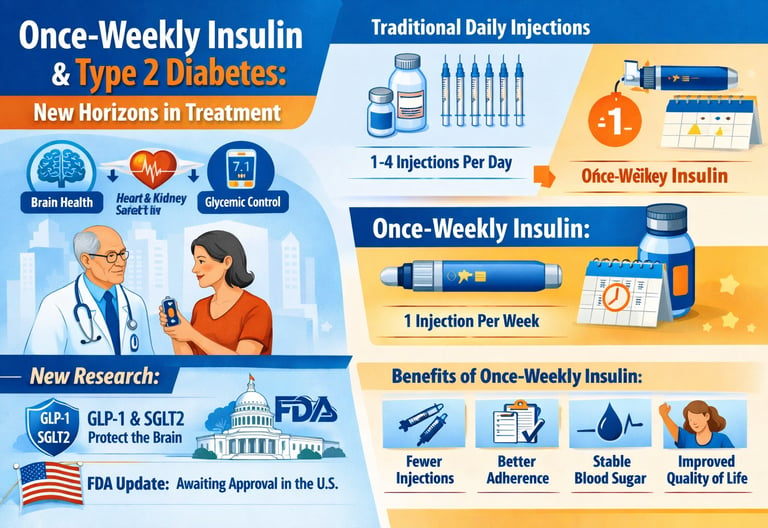
For decades, the story of type 2 diabetes management has been defined by complexity—multiple daily injections, rigid medication schedules, and the constant mental burden of monitoring blood glucose levels. For many patients, especially those requiring basal insulin, effective glycemic control often came at the cost of convenience, adherence, and quality of life. But that narrative is beginning to change.
Recent advances in anti-diabetic agents and insulin therapy are reshaping how clinicians and patients approach type 2 diabetes mellitus. Beyond simply lowering HbA1c, modern treatments now target broader goals—improving medication adherence, minimizing hypoglycemia risk, protecting cardiovascular and renal health, and even addressing concerns about cognitive decline.
Perhaps the most disruptive innovation, however, is the emergence of once-weekly insulin—a paradigm shift in basal insulin therapy. Supported by robust randomized controlled trials and systematic reviews, these ultra–long-acting formulations have demonstrated non-inferior glycemic control compared with daily insulin, while dramatically reducing injection frequency and improving treatment persistence (Soetedjo et al., 2024; Bourron & Denimal, 2026).
As diabetes care moves toward personalized medicine, the question is no longer whether patients can control their blood sugar—but how sustainably, safely, and simply they can do so. Understanding where once-weekly insulin and contemporary diabetes medications fit into this evolving landscape is now essential for informed decision-making in modern diabetes care.
Clinical pearls
1. The "Adherence Advantage" of Weekly Dosing
In clinical terms, once-weekly insulin addresses the treatment burden that often leads to "psychological insulin resistance." The research suggests that by reducing injections from 365 to 52 per year, patients are significantly more likely to stay on track. This isn't just about convenience; it’s about pharmacokinetic stability. A once-weekly dose provides a very steady "basal" or background level of insulin, which can lead to more predictable morning blood sugar readings compared to daily shots that may peak and trough more sharply.
2. The "Legacy Effect" of HbA1c Control
The RCT evidence emphasizes that achieving your HbA1c targets early—even with novel weekly treatments—creates a "metabolic memory." When you use highly adherent treatments (like once-weekly insulin) to keep your average blood sugar stable now, you are effectively "locking in" protection for your small blood vessels (microvasculature) in the eyes, kidneys, and nerves for years to come.
3. Kidney-Neutral and Heart-Friendly Profiles
Patients often worry that adding "stronger" medications like insulin might strain their organs. However, the most recent meta-analyses confirm that once-weekly insulins and SGLT2 inhibitors are renoprotective (kidney-protective). Rather than stressing the kidneys, these medications help manage the pressure within the kidney's filtering units (glomeruli), which is vital for preventing long-term diabetic kidney disease.
4. Managing the "Hypoglycemic Floor"
While once-weekly insulin is a powerful tool, it’s important to understand its long half-life. Because the medication stays in your system for a full week, the "safety profile" is built on a slow, steady release. This means you don't get the sudden, sharp drops in blood sugar often associated with older, fast-acting insulins. Clinical data show that the risk of severe hypoglycemia (dangerously low blood sugar) is no higher than with daily injections, providing a "safety floor" for patients worried about "going low" overnight.
Once-Weekly Insulin : What Type 2 Diabetes Patients Need to Know
This comprehensive guide explores the latest research on diabetes management, including groundbreaking studies on once-weekly insulin and its effect on both blood sugar control and overall health. We'll break down what the science says in patient-friendly language, so you can make informed decisions about your diabetes care.
What Is Type 2 Diabetes? A Quick Overview
Type 2 diabetes is a chronic condition characterised by insulin resistance and elevated blood glucose levels. Unlike type 1 diabetes, your pancreas still produces insulin, but your body can't use it effectively. This leads to the need for diabetes medications and lifestyle modifications to maintain glycemic control and prevent serious complications.
The good news? Modern diabetes treatment options are more effective and convenient than ever before, allowing you to achieve better blood sugar management while fitting treatment into your busy life.
Study 1: Once-Weekly Insulins—A Game Changer for Type 2 Diabetes Management
Understanding Once-Weekly Insulin Therapy
Imagine treating your type 2 diabetes with just one injection per week instead of daily shots. That's the promise of once-weekly insulins—a revolutionary novel treatment that's transforming how patients approach insulin therapy.
A systematic review and meta-analysis by Bourron & Denimal (2026) examined the efficacy and safety of once-weekly insulin formulations in type 2 diabetes mellitus management. This study analyzed data from multiple clinical trials to determine whether these long-acting insulins could deliver comparable results to traditional daily insulin injections while dramatically improving medication adherence.
Key Findings and Safety Profile
Glycemic control achieved with once-weekly insulins was comparable to daily insulin regimens, making them an effective diabetes treatment option
Injection frequency reduction from daily to weekly significantly improved patient compliance and quality of life
Hypoglycemia rates were generally similar between once-weekly and daily insulin groups, indicating comparable safety profiles
Weight gain, a common concern with insulin therapy, was not significantly different between treatment groups
Patient satisfaction dramatically improved due to the convenience factor of weekly insulin injections
For patients struggling with diabetes medication adherence due to the burden of daily injections, once-weekly insulin represents a significant advancement in diabetes care. By reducing the frequency of insulin administration, these formulations help address one of the biggest barriers to effective glucose management—remembering to take your medication.
Study 2: Once-Weekly Insulin as Novel Treatment—RCT Evidence
Randomized controlled trials (RCTs) are considered the gold standard in medical research because they directly compare treatment groups under controlled conditions, providing the strongest evidence for treatment efficacy.
Soetedjo et al. (2024) conducted a systematic review and meta-analysis of RCTs specifically examining once-weekly insulin as a novel treatment for type 2 diabetes mellitus. This research compiled evidence from multiple clinical trials to create a comprehensive picture of how weekly insulin therapy performs in real-world diabetes management.
Research Highlights and Practical Implications
Once-weekly insulin formulations effectively reduced HbA1c levels (a three-month average of blood sugar), demonstrating solid glucose control
Treatment persistence improved significantly, as patients were more likely to continue weekly insulin therapy compared to daily insulin regimens
Cardiovascular outcomes showed no adverse effects, addressing safety concerns about insulin-based diabetes treatment
Renal function remained stable in patients receiving once-weekly insulins, indicating good kidney safety
The time to achieve glycemic targets was comparable to daily insulin, but with superior long-term adherence
Unlike observational studies, which simply observe what happens in real life, RCTs randomly assign patients to different treatments, eliminating bias. This gold-standard evidence confirms that once-weekly insulin isn't just convenient—it's clinically effective for diabetes control.
Comparing Treatment Options: Practical Insights
To make this comparison more digestible, here is the breakdown of Once-Weekly vs. Daily Insulin categorized by the practical factors that matter most to your daily routine:
Dosing Frequency:
Once-Weekly: Requires only one injection per week (52 per year).
Daily: Requires 1 to 4+ injections every day (365–1,460+ per year).
Blood Sugar (Glycemic) Control:
Once-Weekly: Clinical trials show it is comparable to daily regimens in lowering HbA1c.
Daily: Provides comparable control, but relies heavily on the patient never missing a dose.
Medication Adherence:
Once-Weekly: Rated as superior because it is significantly easier for patients to remember and maintain the schedule.
Daily: Often lower due to "treatment fatigue" or the complexity of multiple daily shots.
Safety & Hypoglycemia Risk:
Once-Weekly: Research indicates the risk of "going low" (hypoglycemia) is similar to daily options.
Daily: Similar risk profile, though it may fluctuate more depending on timing and meal consistency.
Lifestyle & Convenience:
Once-Weekly: Considered excellent; it offers more freedom for travel and a less intrusive daily schedule.
Daily: Can be challenging, as it requires constant planning around meals and daily activities.
Financial Investment:
Once-Weekly: May be higher upfront due to the newer technology, though it may reduce long-term costs by preventing complications.
Daily: Variable cost depending on the specific brand and type of insulin used.
Regulatory Status and Regional Availability of Once-Weekly Insulin
Once-weekly insulin formulations—especially insulin icodec—represent a major innovation in basal insulin therapy, but their availability and approval status differ significantly across regions.
✔ Approved / Authorized Regions
In the European Union and multiple countries (including Australia, Canada, Japan, China, and Switzerland), insulin icodec (branded as Awiqli®) has received regulatory approval for adults with type 2 diabetes, offering a once-weekly basal insulin option that reduces injection burden and supports stable glucose control.
This approval reflects global recognition of robust clinical trial evidence showing comparable glycemic control to daily basal insulin with similar safety profiles.
⚠ Pending / Evolving Approvals
In the United States, the status is evolving: insulin icodec is currently investigational following a resubmission of its Biologics License Application (BLA) to the U.S. Food and Drug Administration (FDA) in 2025. If approved, it would become the first once-weekly basal insulin available in the U.S., potentially transforming adherence and treatment convenience for adults with type 2 diabetes.
Earlier, an FDA advisory panel had identified specific issues in review—particularly around manufacturing and indications—highlighting ongoing regulatory refinement before final approval.
While once-weekly insulin represents a significant advance in diabetes care with the potential to improve medication adherence and quality of life, clinicians should be aware of regional regulatory status, prescribing guidelines, and access limitations when considering it. In regions where it is not yet approved, daily basal insulin and contemporary anti-diabetic agents remain the standard of care.
Anti-Diabetic Agents: Choosing What's Right
Different diabetes medications work through different mechanisms:
Metformin reduces glucose production and improves insulin sensitivity
GLP-1 receptor agonists stimulate insulin release and promote weight loss
SGLT2 inhibitors help kidneys remove excess glucose through urine
DPP-4 inhibitors preserve incretin hormones that regulate blood sugar
Once-weekly insulins provide steady basal insulin coverage throughout the week
Your doctor will recommend the best diabetes treatment based on your glucose control, kidney function, weight, and other health conditions.
Key Takeaways: What the Research Tells Us
Once-weekly insulin is game-changing: Both systematic reviews demonstrate that once-weekly insulin therapy delivers comparable glycemic control to daily insulin while dramatically improving medication adherence.
Adherence drives outcomes: The convenience of weekly insulin injections translates to better long-term treatment persistence, which is crucial for preventing diabetes complications.
RCT evidence supports efficacy: Randomized controlled trials confirm that once-weekly insulins are not just convenient—they're clinically equivalent to daily insulin regimens.
Personalization is key: The best diabetes treatment depends on individual factors including glucose targets, lifestyle, kidney function, and concerns about hypoglycemia or weight gain.
FAQs:
Q1: Is once-weekly insulin safe for long-term use?
A: Yes. The research by Bourron & Denimal and Soetedjo et al. found that once-weekly insulin has a comparable safety profile to daily insulin, with similar hypoglycemia rates and no additional concerns about cardiovascular or renal complications.
Q2: Can once-weekly insulin help me lose weight?
A: Weight changes with once-weekly insulin are similar to daily insulin. However, combining insulin therapy with GLP-1 receptor agonists (which promote weight loss) is increasingly common in type 2 diabetes management.
Q3: How often do I need to check my blood sugar on once-weekly insulin?
A: Your doctor will determine a blood glucose monitoring schedule based on your treatment regimen. Some patients check fasting glucose daily, while others use continuous glucose monitors.
Q4: Is once-weekly insulin more expensive than daily insulin?
A: Once-weekly insulin may have higher upfront costs, but improved medication adherence often leads to better glycemic control, potentially reducing long-term complications and overall healthcare costs.
Q5: Can I switch from daily insulin to once-weekly insulin?
A: Many patients can successfully transition to once-weekly insulin therapy under medical supervision. Your endocrinologist or diabetes educator will help with the insulin conversion process.
Q6: What's the difference between systemic review and randomized controlled trials?
A: Systematic reviews analyze all available research on a topic, while RCTs are individual studies where patients are randomly assigned to treatments. RCTs provide the strongest individual evidence, and systematic reviews synthesize multiple RCTs for comprehensive conclusions.
Semantic Keywords: Understanding the Diabetes Treatment Landscape
As you navigate your type 2 diabetes care, you'll encounter terms like:
Insulin resistance: Your body's reduced ability to respond to insulin
HbA1c: A three-month average of blood glucose levels
Basal insulin: Long-acting insulin that provides background coverage
Bolus insulin: Fast-acting insulin taken with meals
Medication adherence: Consistently taking medications as prescribed
Glycemic targets: Your personalized blood sugar goals
Endocrinologist: A doctor specializing in diabetes and hormonal disorders
Continuous glucose monitoring (CGM): A device tracking real-time glucose levels
Clinical Implications and Future Directions
The convergence of evidence from these studies points toward an exciting future in type 2 diabetes management:
Personalized Medicine Approach
Rather than a "one-size-fits-all" approach, modern diabetes care increasingly tailors treatment regimens to individual patient needs. Someone struggling with medication adherence might benefit most from once-weekly insulin, while another patient with weight concerns might prefer GLP-1 receptor agonists.
Combination Therapy
The safety data on anti-diabetic agents encourages combination approaches. For example, pairing once-weekly insulin with GLP-1 agonists addresses both glycemic control and weight management while maintaining safety.
Making Your Decision: Questions to Ask Your Doctor
Before choosing a diabetes treatment regimen, discuss these points with your healthcare provider:
What glycemic targets should I aim for?
Is once-weekly insulin appropriate for my diabetes severity and lifestyle?
How will we monitor my blood glucose—daily testing or continuous monitoring?
What anti-diabetic agents align with my other health conditions?
How often will we reassess my treatment plan?
What support is available for medication adherence?
Are there concerns about hypoglycemia or weight gain?
How do I report side effects or challenges with my diabetes medications?
Author’s Note
This article was written to bridge the gap between rapidly evolving diabetes research and real-world clinical decision-making. Advances such as once-weekly basal insulin and newer anti-diabetic agents represent more than technological innovation—they reflect a shift toward treatment strategies that prioritize long-term adherence, patient convenience, and holistic health outcomes, alongside glycemic control.
The evidence summarized here is drawn from peer-reviewed systematic reviews, randomized controlled trials, and regulatory updates, with careful attention to distinguishing established clinical practice from emerging or region-specific approvals. Where therapies remain investigational or newly approved, this has been clearly stated to support responsible, guideline-aligned care.
Importantly, this article is intended for educational purposes only. Diabetes management must always be individualized, taking into account clinical profile, comorbidities, access, and patient preferences. Readers are encouraged to discuss any potential treatment changes—including once-weekly insulin—with their treating physician or endocrinologist.
As diabetes care continues to evolve toward personalized and patient-centered medicine, informed dialogue between clinicians and patients remains the most powerful therapeutic tool.
About This Information
This article synthesizes evidence from three peer-reviewed studies published in 2024-2026. While based on rigorous scientific research, this content is educational and not a substitute for medical advice. Always consult your healthcare provider before making changes to your diabetes treatment plan.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Individual circumstances vary, and treatment decisions should always be made in consultation with qualified healthcare professionals.
Related Articles
Stop the Clock: Proven Ways to Reverse Early Aging if You Have Diabetes | DR T S DIDWAL
Low-Fat vs. Low-Carb: Which Diet is Best for Weight Loss? | DR T S DIDWAL
5 Steps to Reverse Metabolic Syndrome: Diet, Habit, & Lifestyle Plan | DR T S DIDWAL
The Role of Cholesterol in Health and Disease: Beyond the "Bad" Label | DR T S DIDWAL
Lowering Cholesterol with Food: 4 Phases of Dietary Dyslipidemia Treatment | DR T S DIDWAL
High Triglyceride Levels: 5 New Facts to Help You Lower Your Risk | DR T S DIDWAL
The Best Dietary Fat Balance for Insulin Sensitivity, Inflammation, and Longevity | DR T S DIDWAL
Post-Meal Health: The Hidden 2-Hour Window That Predicts Heart Disease and Diabetes | DR T S DIDWAL
Manage Diabetes Naturally: How Beta-Glucans Control Blood Sugar | DR T S DIDWAL
Insulin vs. Blood Sugar: Why Fasting Insulin Detects Diabetes Years Earlier | DR T S DIDWAL
References
Bourron, O., & Denimal, D. (2026). Efficacy and safety of once-weekly insulins in type 2 diabetes: A systematic review and meta-analysis. Diabetes, Obesity & Metabolism. Advance online publication. https://doi.org/10.1111/dom.70497
Li, Z., Lin, C., Cai, X., Hu, S., Gao, L., & Ji, L. (2024). Anti-diabetic agents and the risks of dementia in patients with type 2 diabetes: A systematic review and network meta-analysis of observational studies and randomized controlled trials. Diabetes Research and Clinical Practice, 210, 111627. https://doi.org/10.1016/j.diabres.2024.111627
Soetedjo, N. N. M., Permana, H., Hariyanto, T. I., Marcella, E., Susanto, H., Sugiarto, S., & Soeroto, A. Y. (2024). Once-weekly insulin as novel treatment for type 2 diabetes mellitus: A systematic review and meta-analysis of randomized clinical trials. Diabetes Research and Clinical Practice, 211, 111630. https://doi.org/10.1016/j.diabres.2023.110984