Insulin vs. Blood Sugar: Why Fasting Insulin Detects Diabetes Years Earlier
Discover why fasting insulin rises years before blood sugar. Learn how early insulin testing can detect diabetes risk and prevent complications.
DIABETES
Dr. T.S. Didwal, M.D.
12/23/202511 min read
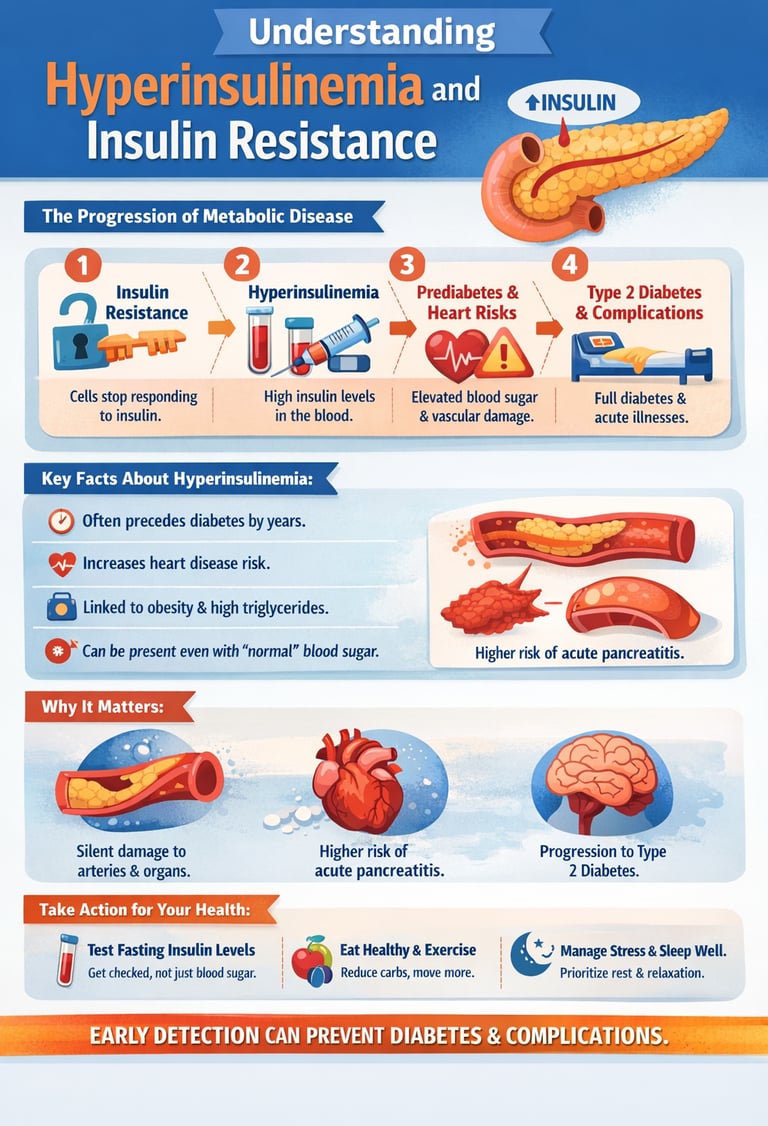
Most people believe diabetes begins the day blood sugar rises. In reality, the disease often starts years earlier, quietly and invisibly, while standard tests still look “normal.” During this hidden phase, the pancreas is not failing—it is working too hard. It floods the bloodstream with insulin in an attempt to keep glucose under control. This state, known as hyperinsulinemia, is the metabolic warning signal we rarely measure, rarely explain, and too often ignore.
For many patients, this silent overload of insulin damages blood vessels, stiffens arteries, alters lipid metabolism, and drives weight gain—all before diabetes is ever diagnosed. You may be told your fasting glucose is normal, your HbA1c reassuring, and yet your cardiovascular risk is already rising. The paradox is striking: insulin, the hormone we prescribe to save lives, can become harmful when chronically elevated.
Understanding hyperinsulinemia changes how we view diabetes, prediabetes, obesity, heart disease, and even acute conditions like pancreatitis. It shifts the focus from chasing blood sugar numbers to understanding why the body is forced to overproduce insulin in the first place. This article explores that hidden biology—clearly, scientifically, and clinically—because recognizing disease early is not alarmist medicine. It is preventive medicine at its most powerful.
Clinical Pearls
1. The "Pancreatic Redline"
Think of your pancreas like a car engine. In the early stages of insulin resistance, your pancreas "redlines"—it revs at maximum RPMs to produce massive amounts of insulin just to keep your blood sugar in the normal range.
Clinical Pearl: A "normal" blood sugar reading can be deceptive. If your insulin is high (Hyperinsulinemia) while your sugar is normal, your engine is redlining. Testing Fasting Insulin along with Glucose is the only way to see how hard your "engine" is actually working.
2. The "Last to Know" Marker (HbA1c)
Many patients rely on HbA1c, which measures your average blood sugar over three months. However, in the 2025 Accoli et al. research, we see that cellular insulin resistance starts a decade before the HbA1c ever moves.
Clinical Pearl: HbA1c is a "lagging indicator"—it tells you about the fire after the house is already smoky. To catch metabolic issues early, monitor your Triglyceride-to-HDL ratio. A high ratio is often the first "smoke" signal that your cells are becoming resistant to insulin.
3. The "Muscle Sponge" Advantage
Your skeletal muscles are your body's largest "sink" for glucose, moving up to 80% of post-meal sugar out of the blood. Insulin resistance happens when these "sponges" get "full" or "crusty."
Clinical Pearl: Resistance training (lifting weights) effectively "wrings out the sponge." By building muscle, you create more storage space for glucose, which naturally lowers the amount of insulin your pancreas needs to produce. This is why muscle is often called "metabolic currency.
4. The Endothelial "Irritant"
We used to think high sugar damaged blood vessels. We now know from the Bkaily et al. (2025) study that high insulin itself is an irritant. Chronic hyperinsulinemia tells the kidneys to hold onto salt and causes the smooth muscles in your arteries to thicken.
Clinical Pearl: If you have high blood pressure that won't budge, the root cause might be your insulin levels, not just your salt intake. Lowering insulin levels can often lead to a spontaneous "whoosh" of water weight and lower blood pressure as the kidneys finally release excess sodium.
5. The "Second Meal Effect"
Metabolic health isn't just about what you eat; it’s about the order in which you eat it.
Clinical Pearl: To protect your pancreas, use the "Fiber-First" rule. Eating fiber (like a salad or beta-glucan-rich oats) before carbohydrates creates a physical gel in the gut. This slows down the "sugar rush," ensuring that your insulin response is a gentle wave rather than a tsumani. This protects your pancreatic "beta cells" from wearing out prematurely.
Hyperinsulinemia and Insulin Resistance: Understanding Diabetes's Silent Partner and Emerging Complications
What Are Hyperinsulinemia and Insulin Resistance?
Hyperinsulinemia refers to elevated fasting insulin levels in the bloodstream, typically indicating that your pancreas is working overtime to manage blood glucose. Meanwhile, insulin resistance means your cells aren't responding properly to insulin signals, forcing your pancreas to produce even more insulin to compensate.
Think of it like a locked door: insulin is the key, but if the lock is broken (insulin resistance), you need to jiggle the key harder and more frequently (hyperinsulinemia). This exhausting process eventually wears down the system, leading to type 2 diabetes and numerous complications.
The Metabolic Connection
The relationship between hyperinsulinemia and insulin resistance is bidirectional. High insulin levels can actually worsen insulin resistance over time, creating a vicious cycle that's difficult to break without intervention. This mechanism is central to understanding why prediabetes so often progresses to full-blown type 2 diabetes if left unaddressed.
Study 1: Diabetes and Its Silent Partner – A Critical Review of Hyperinsulinemia
Rangraze et al. (2025) conducted a comprehensive critical review published in Current Diabetes Reviews examining hyperinsulinemia as a significant complication of diabetes. This research aggregates existing evidence to provide a thorough understanding of how hyperinsulinemia functions as diabetes's shadow companion, often overlooked in clinical practice.
Key Findings and Takeaways
The study highlights that hyperinsulinemia isn't merely a symptom of diabetes—it's an independent risk factor for numerous complications. The research emphasizes:
Hyperinsulinemia precedes the development of type 2 diabetes by years, making it a critical early warning sign
High insulin levels contribute to metabolic syndrome, a cluster of conditions including obesity, hypertension, and dyslipidemia
Hyperinsulinemia independently increases cardiovascular risk, regardless of glucose control
Current clinical practice often fails to measure or monitor fasting insulin levels, missing crucial early intervention opportunities
Clinical Significance
The critical takeaway from Rangraze et al. (2025) is that managing hyperinsulinemia should be as important as managing blood glucose. Many patients with elevated insulin levels appear to have "normal" blood sugar—until they don't. By the time glucose becomes elevated, significant metabolic damage has often already occurred.
Study 2: Hyperinsulinemia and Hypertriglyceridemia-Induced Acute Pancreatitis
Wang et al. (2025) investigated the impact of hyperinsulinemia on short-term prognosis in patients with hypertriglyceridemia-induced acute pancreatitis in Frontiers in Endocrinology. This study bridges the gap between metabolic dysfunction and a serious acute illness, revealing previously underappreciated connections.
Key Findings and Takeaways
Patients with elevated hyperinsulinemia show significantly worse outcomes following acute pancreatitis episodes
Hyperinsulinemia compounds the inflammatory response triggered by hypertriglyceridemia, exacerbating pancreatic damage
Fasting insulin levels can predict prognosis more reliably than traditional markers in acute pancreatitis cases
The presence of hyperinsulinemia may necessitate more aggressive therapeutic interventions
Clinical Implications
This research reveals that hyperinsulinemia isn't just a chronic disease concern—it directly impacts acute medical emergencies. Patients with both metabolic syndrome and high triglycerides face compounded risks, and recognizing hyperinsulinemia as a prognostic factor could improve treatment strategies during critical illness.
Study 3: Insulin Resistance in Type 2 Diabetes Mellitus
Accoli, Deng, and Liu (2025) published a comprehensive article in Nature Reviews Endocrinology examining insulin resistance as the fundamental pathophysiological mechanism underlying type 2 diabetes mellitus. This prestigious review consolidates current understanding of how cellular-level insulin resistance translates into systemic disease.
Key Findings and Takeaways
Insulin resistance begins at the cellular level, primarily in muscle, liver, and adipose tissue
Genetic predisposition interacts with lifestyle factors to determine insulin resistance severity
Insulin resistance triggers inflammatory pathways that further impair metabolic function
The progression from insulin resistance to type 2 diabetes involves both worsening insulin resistance and declining beta-cell function
Emerging therapies targeting insulin resistance mechanisms show promise beyond traditional glucose-lowering drugs
Pathophysiological Significance
Accoli et al. (2025) emphasizes that type 2 diabetes isn't simply a disease of high blood sugar—it's fundamentally a disease of insulin resistance and cellular dysfunction. Understanding these molecular mechanisms opens new therapeutic pathways and explains why treating only blood glucose levels often proves insufficient for preventing complications.
Study 4: Pathophysiology of Prediabetes, Hyperinsulinemia, and Cardiovascular Disease
Bkaily et al. (2025) explored the pathophysiology of prediabetes, hyperinsulinemia, and their effects on the cardiovascular system in Biomedicines. This research specifically connects metabolic dysfunction to heart and blood vessel disease—two of the most serious complications facing millions.
The study reveals multiple cardiovascular mechanisms:
Hyperinsulinemia directly damages endothelial cells (the inner lining of blood vessels), promoting atherosclerosis
Insulin resistance in the cardiovascular system impairs vasodilation, contributing to hypertension
Prediabetes with hyperinsulinemia creates a prothrombotic state, increasing clot formation risk
Metabolic dysfunction in prediabetes accelerates arterial stiffness and cardiac remodeling
Early identification and treatment of hyperinsulinemia in prediabetes could prevent progression to cardiovascular disease
Cardiovascular Prevention Implications
Perhaps most importantly, Bkaily et al. (2025) demonstrates that hyperinsulinemia in prediabetes represents a critical intervention window. Patients with prediabetes and elevated insulin levels face significantly elevated cardiovascular risk—even before developing type 2 diabetes. This shifts the clinical paradigm toward earlier, more aggressive metabolic intervention.
Synthesizing the Research: The Complete Picture of Hyperinsulinemia
The Progression Mode
Stage 1: Insulin Resistance Develops (Accoli et al., 2025) Cellular dysfunction begins, insulin sensitivity declines, pancreatic compensation increases
Stage 2: Hyperinsulinemia Emerges (Rangraze et al., 2025) Elevated fasting insulin becomes measurable, metabolic syndrome components appear, cardiovascular changes begin silently
Stage 3: Prediabetes and Cardiovascular Complications (Bkaily et al., 2025) Blood glucose begins rising, cardiovascular damage accelerates, hypertension and dyslipidemia worsen
Stage 4: Type 2 Diabetes and Acute Complications (Wang et al., 2025) Full diabetes diagnosis, risk for serious acute events like hypertriglyceridemia-induced acute pancreatitis increases dramatically
The Common Thread
All four studies emphasize that hyperinsulinemia and insulin resistance aren't simply late-stage diabetes findings—they're early pathological processes that, once recognized, present crucial treatment opportunities. Yet many patients progress through stages 1-3 without any intervention because these markers aren't routinely monitored.
Why This Matters: Real-World Health Implications
Beyond Blood Sugar Testing
Conventional medical practice primarily focuses on fasting glucose and HbA1c levels to diagnose and monitor type 2 diabetes. But research shows these tests miss the earliest and most preventable stages of metabolic disease. By the time glucose becomes abnormal, years of insulin resistance and hyperinsulinemia have already damaged your cardiovascular system, pancreas, and organs.
The Prevention Paradigm Shift
The cumulative evidence suggests we need to shift toward measuring fasting insulin levels and insulin resistance markers (such as HOMA-IR—Homeostatic Model Assessment for Insulin Resistance) as standard screening tools. This simple change in clinical practice could identify at-risk individuals decades before conventional diagnosis.
Individual Risk Factors
Your risk for hyperinsulinemia and insulin resistance depends on:
Genetics: Family history of type 2 diabetes or cardiovascular disease
Obesity: Excess adipose tissue strongly promotes insulin resistance
Physical inactivity: Sedentary behavior worsens cellular insulin resistance
Dietary patterns: Refined carbohydrates and sugar exacerbate hyperinsulinemia
Chronic stress: Elevated cortisol worsens metabolic dysfunction
Sleep deprivation: Poor sleep quality impairs insulin signaling
Aging: Insulin resistance naturally increases with age
Practical Steps for Prevention and Management
Lifestyle Interventions
Dietary Approaches
Emphasize whole foods, fiber, and complex carbohydrates over refined options
Reduce added sugar and ultra-processed foods
Include protein and healthy fats with each meal to moderate insulin response
Consider intermittent fasting or time-restricted eating under professional guidance
Physical Activity
Engage in resistance training to improve muscle insulin sensitivity
Perform at least 150 minutes of moderate aerobic exercise weekly
Include high-intensity interval training for enhanced metabolic benefits
Move regularly throughout the day, not just during formal exercise
Sleep and Stress Management
Target 7-9 hours of quality sleep nightly
Implement stress-reduction practices like meditation or yoga
Maintain consistent sleep and wake times
Medical Monitoring
Request fasting insulin measurement during routine checkups
Calculate HOMA-IR (Homeostatic Model Assessment for Insulin Resistance) with your healthcare provider
Monitor triglyceride and HDL cholesterol levels as markers of insulin resistance
Track waist circumference and body composition, not just weight
When to Seek Professional Help
Family history of type 2 diabetes or early cardiovascular disease
Prediabetes diagnosis with elevated fasting insulin
Difficulty achieving metabolic goals with lifestyle changes alone
Multiple components of metabolic syndrome
Unusual triglyceride elevation or hypertriglyceridemia
Frequently Asked Questions
Q: Can you have hyperinsulinemia without diabetes?
A: Absolutely. In fact, hyperinsulinemia typically precedes type 2 diabetes by years. You can have elevated fasting insulin with completely normal blood glucose—this is the stage when intervention is most effective.
Q: How is hyperinsulinemia diagnosed?
A: Primarily through fasting insulin measurement (normal is typically below 12 mIU/L, though optimal is under 8) and calculated insulin resistance indices like HOMA-IR. Glucose tolerance tests can also reveal hyperinsulinemia through elevated insulin responses.
Q: Is hyperinsulinemia reversible?
A: Yes, in many cases. Insulin resistance and hyperinsulinemia respond well to lifestyle interventions—weight loss, exercise, and dietary changes can significantly improve insulin sensitivity within weeks to months.
Q: How does hyperinsulinemia cause cardiovascular disease?
A: Hyperinsulinemia damages blood vessel linings, promotes inflammation, increases sodium retention (raising blood pressure), and promotes atherosclerosis. These mechanisms explain why insulin resistance predicts cardiovascular events independent of blood glucose levels.
Q: Can acute pancreatitis be caused by hyperinsulinemia?
A: Not directly, but hyperinsulinemia and insulin resistance often accompany hypertriglyceridemia, which is a major cause of acute pancreatitis. Additionally, hyperinsulinemia worsens outcomes if acute pancreatitis develops.
Q: Should everyone with prediabetes be concerned about hyperinsulinemia?
A: Yes. Prediabetes represents the stage when hyperinsulinemia is typically present and causing silent damage. However, not all prediabetic individuals have elevated insulin—this is why measuring fasting insulin is so important.
Q: What's the difference between treating glucose versus insulin resistance?
A: Glucose-lowering drugs address symptoms (high blood sugar) but don't necessarily address the underlying insulin resistance. Treating insulin resistance directly through lifestyle changes or metabolic drugs addresses the root problem and provides more comprehensive protection against complications.
Key Takeaways
Hyperinsulinemia is a predictable precursor to type 2 diabetes, often appearing years before blood glucose becomes abnormal (Rangraze et al., 2025).
Insulin resistance occurs at the cellular level and involves complex molecular mechanisms affecting muscle, liver, and fat tissue (Accoli et al., 2025).
Hyperinsulinemia significantly worsens outcomes in serious acute illnesses like hypertriglyceridemia-induced acute pancreatitis, demonstrating broad systemic effects (Wang et al., 2025).
Prediabetes with hyperinsulinemia creates substantial cardiovascular risk through multiple mechanisms, even before type 2 diabetes develops (Bkaily et al., 2025).
Fasting insulin measurement should become standard screening, as it identifies disease at the most preventable stage.
Lifestyle interventions targeting insulin resistance are remarkably effective, often producing measurable improvements within weeks to months.
Early intervention in the hyperinsulinemia stage can prevent progression to diabetes and its serious complications.
Call to Action
Don't wait for a diabetes diagnosis to address metabolic dysfunction. The research is clear: hyperinsulinemia and insulin resistance are early, detectable, and highly treatable conditions. If you have any risk factors for metabolic disease—family history, excess weight, sedentary lifestyle, or prediabetes diagnosis—take these three steps today:
Schedule a comprehensive metabolic panel with your healthcare provider, specifically requesting fasting insulin measurement and HOMA-IR calculation.
Implement one dietary change this week: Replace one sugary beverage daily with water, or add one serving of vegetables to dinner. Small, sustainable changes compound into major health improvements.
Increase movement: Add a 15-minute walk to your daily routine. Movement is medicine for insulin resistance, and even modest activity produces measurable benefits.
Conclusion
The paradigm shift in metabolic medicine is clear: we must stop waiting for blood sugar to fail before we intervene. As the 2025 research from Accoli, Bkaily, and others demonstrates, the true "pole position" for preventing chronic disease lies in identifying Hyperinsulinemia—the silent engine strain that precedes a diabetes diagnosis by a decade.
By prioritizing fasting insulin over late-stage markers like HbA1c, we move from a reactive "damage control" model to true preventive medicine. Understanding the HOMA-IR and your own "Pancreatic Redline" empowers you to make targeted lifestyle shifts—such as "Fiber-First" eating and resistance training—when they are most effective. These interventions don't just lower a number on a lab report; they protect the delicate endothelial lining of your arteries and preserve the longevity of your pancreatic beta cells.
The choice is no longer between "normal" and "diabetic." It is about recognizing the spectrum of insulin sensitivity and taking action while your body still has the resilience to heal. Your health is not defined by a single glucose reading, but by the efficiency of the underlying machinery. By monitoring the right parameters today, you are securing a future free from the complications of metabolic failure.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Individual circumstances vary, and treatment decisions should always be made in consultation with qualified healthcare professionals.
Related Articles
Stop the Clock: Proven Ways to Reverse Early Aging if You Have Diabetes | DR T S DIDWAL
Low-Fat vs. Low-Carb: Which Diet is Best for Weight Loss? | DR T S DIDWAL
5 Steps to Reverse Metabolic Syndrome: Diet, Habit, & Lifestyle Plan | DR T S DIDWAL
The Role of Cholesterol in Health and Disease: Beyond the "Bad" Label | DR T S DIDWAL
Lowering Cholesterol with Food: 4 Phases of Dietary Dyslipidemia Treatment | DR T S DIDWAL
High Triglyceride Levels: 5 New Facts to Help You Lower Your Risk | DR T S DIDWAL
The Best Dietary Fat Balance for Insulin Sensitivity, Inflammation, and Longevity | DR T S DIDWAL
Post-Meal Health: The Hidden 2-Hour Window That Predicts Heart Disease and Diabetes | DR T S DIDWAL
Manage Diabetes Naturally: How Beta-Glucans Control Blood Sugar | DR T S DIDWAL
References
Accoli, D., Deng, Z., & Liu, Q. (2025). Insulin resistance in type 2 diabetes mellitus. Nature Reviews Endocrinology, 21, 413–426. https://doi.org/10.1038/s41574-025-01114-y
Bkaily, G., Jazzar, A., Abou-Aichi, A., & Jacques, D. (2025). Pathophysiology of prediabetes hyperinsulinemia and insulin resistance in the cardiovascular system. Biomedicines, 13(8), 1842. https://doi.org/10.3390/biomedicines13081842
Rangraze, I. R., El-Tanani, M., Arman Rabbani, S., Babiker, R., Matalka, I. I., & Rizzo, M. (2025). Diabetes and its silent partner: A critical review of hyperinsulinemia and its complications. Current Diabetes Reviews, 21(9), e15733. https://doi.org/10.2174/0115733998311738240813110032
Wang, M., Zheng, L., Qian, L., & Xu, M. (2025). The impact of hyperinsulinemia on short-term prognosis in patients with hypertriglyceridemia-induced acute pancreatitis. Frontiers in Endocrinology, 16, 1646307. https://doi.org/10.3389/fendo.2025.1646307