Metabolic Flexibility: Train Your Body to Switch Between Fat and Sugar for Better Diabetes Control
Discover how metabolic flexibility is redefining Type 2 Diabetes treatment. Explore 2025 research on personalized lifestyle interventions and precision medicine.
DIABETES
Dr. T.S. Didwal, M.D.
12/22/202510 min read
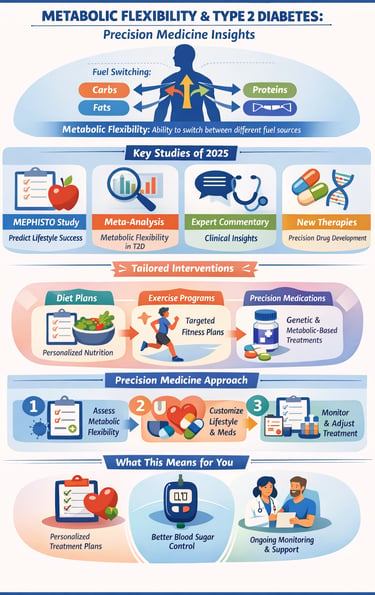
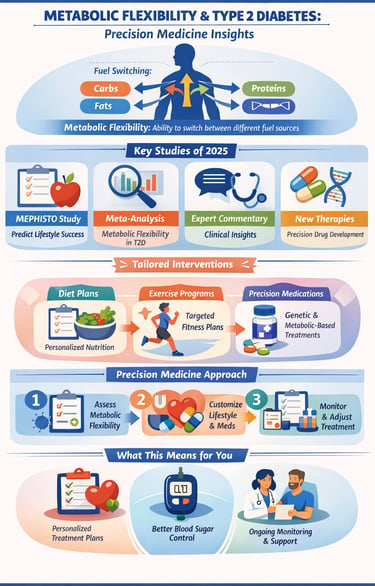
If you've been following diabetes research lately, you've probably heard the term metabolic flexibility popping up everywhere. But what exactly is it, and why should you care? Metabolic flexibility refers to your body's ability to switch between using different fuel sources—carbohydrates, fats, and proteins—depending on availability and energy demands. Think of it like having a versatile engine that can run on multiple fuel types seamlessly.
Recent groundbreaking research is reshaping how we understand and treat type 2 diabetes, suggesting that metabolic flexibility might be the key to predicting which patients will benefit most from lifestyle interventions. This discovery has profound implications for precision medicine and personalized diabetes management.
In this comprehensive guide, we'll explore four pivotal 2025 studies that illuminate the relationship between metabolic flexibility and type 2 diabetes, and how these findings could revolutionize your treatment options.
Clinical pearls
1. The "Hybrid Engine" Efficiency
Think of your body like a hybrid car. A healthy metabolism should switch seamlessly between burning "electricity" (stored fat) and "gasoline" (glucose from food). In type 2 diabetes, the "switch" often gets stuck.
Clinical Pearl: Being metabolically flexible means your body doesn't panic when you skip a meal. If you can go 4–5 hours without a snack and still feel focused, your "hybrid engine" is likely switching over to fat-burning mode efficiently.
2. Muscle as the "Flexibility Factory"
The 2025 MEPHISTO study highlights that your muscles are where the most fuel-switching happens. Inside your muscle cells, tiny power plants called mitochondria decide what to burn.
Clinical Pearl: "Zone 2" exercise—activity where you can still hold a conversation but are breathing heavily—is the gold standard for fixing a "rusty" switch. It forces your muscle mitochondria to become fat-burning specialists, improving your overall flexibility.
3. The "Mitochondrial Traffic Jam"
Metabolic inflexibility is often just a "traffic jam" at the cellular level. When we eat too frequently, the mitochondria get overwhelmed with too many fuel signals at once, leading to cellular "indecision" and insulin resistance.
Clinical Pearl: Giving your body a "rest period" from digestion (like 12–14 hours of overnight fasting) acts like a traffic controller. It clears the backlog of fuel and allows your cells to recalibrate their ability to burn fat.
4. Precision Over Procrastination
The research by Hansen et al. (2025) shows that not every person with diabetes is "inflexible." This is why a one-size-fits-all diet often fails.
Clinical Pearl: If a low-carb diet makes you feel energized, you likely have some fat-burning flexibility. If it makes you feel weak and "foggy" for weeks, your cellular machinery may need a more gradual approach, like "Carb Cycling," to retrain the switch slowly.
5. The "Fuel Priority" Rule
Your body has a strict hierarchy for burning fuel. It will always try to burn alcohol first, then sugar, then fat. If there is always sugar in the system, the "fat-burning" door stays locked.
Clinical Pearl: To improve flexibility, try the "Fiber, Protein, Fat, then Carb" eating order. By slowing down the sugar entry, you prevent the massive insulin spike that "locks" your fat stores, allowing your body to keep its fuel-switching options open throughout the day.
Metabolic Flexibility and Type 2 Diabetes
Study 1: MEPHISTO Protocol—Predicting Lifestyle Intervention Success
The MEPHISTO (Metabolic Flexibility to Predict Lifestyle Interventions Outcomes) study represents an ambitious attempt to answer a critical clinical question: Can we predict which patients will respond best to lifestyle interventions before they even start?
According to Ludlova et al (2025), the MEPHISTO protocol is designed as a predictive validation study and randomized controlled trial aimed at determining whether baseline metabolic flexibility can forecast lifestyle intervention outcomes in individuals with metabolic disorders.
Key Study Features
This protocol-based research establishes a rigorous framework for:
Baseline metabolic assessment: Measuring participants' initial metabolic flexibility using standardized protocols
Intervention tracking: Following participants through structured lifestyle interventions
Outcome prediction: Correlating baseline flexibility metrics with actual intervention success rates
Precision matching: Identifying which patients should prioritize dietary changes versus exercise versus combined approaches
Key Takeaways
The researchers emphasize that understanding metabolic flexibility at the outset could transform how clinicians design personalized intervention strategies. Rather than applying a one-size-fits-all approach, healthcare providers could use metabolic flexibility assessments to tailor interventions to individual physiological capabilities. This shift toward precision medicine in diabetes management means patients might finally receive recommendations based on their unique metabolic profiles rather than generic guidelines.
Study 2: The Metabolic Inflexibility Question in Type 2 Diabetes
Exploring the Evidence: Are People With Type 2 Diabetes Actually Metabolically Inflexible?
While the concept of metabolic inflexibility in type 2 diabetes seems intuitive, Hansen et al. (2025) decided to put it to the test through a comprehensive systematic review and meta-analysis. Their question was deceptively simple yet scientifically crucial: Do individuals with type 2 diabetes truly exhibit metabolic inflexibility?
The meta-analysis synthesized data from multiple studies examining:
Metabolic substrate utilization in diabetic versus non-diabetic populations
Insulin resistance and its relationship to fuel substrate switching
Mitochondrial function and energy substrate preference
Carbohydrate and fat oxidation capacity under varying conditions
Hansen and colleagues' findings reveal a nuanced picture. Rather than a clear-cut conclusion that type 2 diabetes inherently causes metabolic inflexibility, the research suggests the relationship is more complex. Some individuals with type 2 diabetes demonstrate impaired metabolic flexibility, while others maintain relatively preserved switching capacity despite elevated blood glucose. This heterogeneity is critical because it validates the precision medicine approach championed by other researchers in this field.
Key Takeaways
Metabolic inflexibility is not universal in type 2 diabetes populations
Individual variation is substantial and clinically meaningful
Assessment of metabolic flexibility could identify subgroups most likely to benefit from metabolic rehabilitation
Understanding this heterogeneity is essential for designing effective personalized treatment plans
Study 3: The Expert Perspective—Moving Research to the Real World
When a massive analysis like the Hansen study (Study 2) is released, the scientific community weighs in to figure out how it changes actual patient care. Koudelkova et al (2025) provided a "bridge" between the laboratory findings and the doctor’s office.
:The experts point out that "metabolic flexibility" isn't just a yes/no label. Because the studies use different ways to measure it, some results can seem confusing. However, the core takeaway is clear: treatment must be stratified. In medical terms, stratification means grouping patients by how their bodies actually function, rather than just their diagnosis.
The "Flexible" Group: These patients might thrive on a standard diet and exercise plan.
The "Inflexible" Group: These patients may have a "stiff" metabolic switch and need specific help—like medical fasting or targeted medications—to help their cells start burning fat again.
The Patient Takeaway: If you’ve ever felt like a "failed patient" because a popular diet didn't work for you, this commentary is your vindication. It suggests that your specific "metabolic profile" should dictate your treatment, not a generic pamphlet.
Study 4 The Future of Diabetes Medicines Precision over "Trial and Error"
Historically, diabetes drugs were designed to work for "the average person." But as Tian et al. (2025) explain, precision medicine is changing the blueprint for new medications. Instead of just lowering blood sugar, new drugs are being designed to fix the root causes of metabolic "stiffness."
Key Scientific Targets :
Mitochondrial Repair: Instead of just adding more insulin, researchers are looking at drugs that "repair" the power plants in your cells so they can switch fuels naturally.
Genetic Biomarkers: Scientists are identifying specific "tags" in your DNA that can tell a doctor, "This person will respond perfectly to Medication A, but will have side effects with Medication B."
The GLP-1 and SGLT2 Evolution: You may know these as popular weight-loss or heart-health diabetes meds. New research is looking at how to use these drugs specifically to "unlock" fat-burning doors in patients who are currently metabolically stuck.
The Patient Takeaway: We are moving away from "trial and error" medicine. The next generation of diabetes care isn't just about "controlling" your sugar; it's about using your unique genetic and metabolic markers to pick the exact tool that restores your body's natural "hybrid engine."
Connecting the Research: The Integrated Picture
While each study approaches type 2 diabetes from a different angle, together they paint a compelling picture of where diabetes care is heading:
MEPHISTO provides the clinical framework for using metabolic flexibility assessments to predict intervention outcomes. Hansen's meta-analysis clarifies that metabolic inflexibility isn't universal in type 2 diabetes, validating MEPHISTO's precision approach. Koudelkova's commentary bridges laboratory findings with clinical application. Finally, Tian's research shows how precision medicine extends beyond behavior change into pharmaceutical development. The unifying theme: One-size-fits-all diabetes treatment is obsolete. The future belongs to personalized, metabolically informed precision medicine.
Zone 2 Exercise: The "Mitochondrial Tune-Up"
The article calls muscle the "Flexibility Factory." Zone 2 exercise is the specific intensity that forces your mitochondria to stop relying on easy-access sugar and start burning fat efficiently.
The Intensity: You should be moving at a pace where you can still hold a conversation, but you are breathing heavily enough that you'd rather not. If you can sing, you’re going too slow; if you’re gasping for air, you’re going too fast.
The Goal: 60% - 70% of your maximum heart rate.
The Routine: Aim for 30–45 minutes, 3-4 times a week.
Why it works: High-intensity "sprints" burn sugar (anaerobic). Stable, moderate Zone 2 activity "cleans the rust" off the fat-burning machinery in your muscle cells.
Carb Cycling: The "Slow Retrain"
If you have been type 2 diabetic for a long time, the article suggests your "switch" might be stuck. Jumping straight into a strict low-carb diet can lead to "brain fog" because your body has forgotten how to access fat stores.
The "Step-Down" Approach:
Training Days: On days you do your Zone 2 exercise, include healthy complex carbohydrates (sweet potatoes, berries, oats) to fuel the movement.
Rest Days: On days you are sedentary, focus strictly on high protein, healthy fats, and fiber-rich vegetables.
The "Eating Order": Regardless of the day, always eat in this order:
Fiber (Salad/Greens)
Protein/Fat (Meat/Eggs/Nuts)
Carbs (Starches/Fruits)
Why this works: Eating fiber and protein first creates a "mesh" in your gut that slows down the absorption of sugar, preventing the insulin spike that locks the "fat-burning door."
Practical Implications: What This Means for Patients and Clinicians
For Patients with Type 2 Diabetes
Metabolic assessment could soon become standard before starting lifestyle interventions
Your intervention plan should be tailored to your individual metabolic flexibility status
Combining lifestyle changes with precision pharmacotherapy offers better outcomes than either alone
Monitoring metabolic flexibility over time helps track real physiological improvements, not just blood glucose levels
For Healthcare Providers
Incorporating metabolic flexibility assessment into routine type 2 diabetes evaluation
Moving beyond standardized intervention protocols toward personalized treatment pathways
Staying informed about emerging precision medicine approaches in drug selection
Recognizing that patients respond differently to identical interventions based on metabolic phenotype
The "Metabolic Switch" Progress Tracker
As your "hybrid engine" becomes more efficient, you should notice these changes in your daily life:
1. The "Hunger" Test
The Inflexible State: You get "hangry" (irritable/shaky) if you miss a meal by 30 minutes. You feel like you must snack between lunch and dinner.
The Flexible State: You can comfortably go 4–6 hours between meals without a drop in mood or focus. This is a sign your body has successfully "switched" to burning fat stores to keep your brain fueled.
2. Morning Energy Levels
The Inflexible State: You wake up feeling "foggy" and feel you need coffee or a sugary breakfast just to start your brain.
The Flexible State: You wake up with clear-headed energy before you even eat. This indicates your body maintained steady fuel levels overnight via fat oxidation.
3. Post-Meal Focus
The Inflexible State: You experience a "food coma" or extreme sleepiness 30–60 minutes after a meal (especially a high-carb one).
The Flexible State: You feel satisfied but energized after eating. Your body is handling the glucose entry without a massive insulin spike that "shuts down" the system.
FAQs: Answering Your Burning Questions
What exactly is metabolic flexibility, and why does it matter?
Metabolic flexibility is your body's ability to switch between different fuel sources—carbs, fats, and proteins. It matters because individuals with good metabolic flexibility can adapt to dietary changes and exercise more effectively, making them better candidates for lifestyle-based interventions.
Does everyone with type 2 diabetes have metabolic inflexibility?
No. Hansen's meta-analysis shows that while some people with type 2 diabetes have impaired metabolic flexibility, others maintain relatively normal switching capacity. This variation is why precision assessment is so valuable.
How soon will the MEPHISTO protocol be available clinically?
As a validation study, MEPHISTO is ongoing. Results will likely inform clinical guidelines within the next few years, but widespread adoption will depend on regulatory approval and healthcare system integration.
Can lifestyle interventions alone fix metabolic inflexibility?
For many patients, yes—but not all. That's why the research emphasizes precision medicine approaches that combine metabolic assessment, tailored lifestyle interventions, and when necessary, targeted medications.
What's the difference between traditional and precision medicine approaches to type 2 diabetes?
Traditional approaches use the same treatment recommendations for everyone. Precision medicine assesses individual metabolic markers, genetic factors, and lifestyle capacity to create customized treatment plans that work with your unique biology rather than against it.
How are new drugs being developed differently under precision medicine?
Instead of creating drugs that work for most people, researchers now identify specific therapeutic targets that address the root causes of disease in particular patient subgroups. This results in more effective treatments with fewer side effects for individuals who match the metabolic profile the drug was designed for.
Should I ask my doctor for metabolic flexibility testing?
While still not routine, it's worth discussing. As this research becomes more mainstream, metabolic flexibility assessment may become standard. Your doctor can help determine if testing is appropriate for your situation.
Conclusion
Metabolic flexibility—the body’s ability to switch between fuel sources like carbohydrates, fats, and proteins—is emerging as a key factor in type 2 diabetes management. Recent research shows that not all patients with type 2 diabetes exhibit metabolic inflexibility, highlighting the importance of individualized assessment. The MEPHISTO study demonstrates that measuring baseline metabolic flexibility can predict which patients will respond best to lifestyle interventions, such as diet and exercise. Complementing this, systematic reviews indicate significant variability in metabolic flexibility among diabetic populations, reinforcing the need for personalized approaches. Expert commentaries emphasize standardized assessment methods and bridging research with clinical practice.
In parallel, precision medicine is reshaping drug development, identifying genetic, metabolic, and molecular targets to optimize therapy. Combining lifestyle interventions with targeted medications tailored to a patient’s metabolic profile offers superior outcomes compared with conventional, one-size-fits-all approaches. For patients, this means personalized treatment plans, better blood glucose control, and ongoing monitoring. For clinicians, integrating metabolic flexibility assessment into routine care can guide intervention choices and improve long-term outcomes.
In essence, understanding and optimizing metabolic flexibility represents a transformative step toward precision, evidence-based diabetes care, enabling interventions that align with each patient’s unique physiology.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Individual circumstances vary, and treatment decisions should always be made in consultation with qualified healthcare professionals.
Related Articles
The Metabolic Triad: Why Diabetes, Obesity & CVD Are One Epidemic | DR T S DIDWAL
What’s New in the 2025 Blood Pressure Guidelines? A Complete Scientific Breakdown | DR T S DIDWAL
Manage Diabetes Naturally: How Beta-Glucans Control Blood Sugar | DR T S DIDWAL
Exercise as Metabolic Medicine: Latest Research on Glucose and Heart Health| DR T S DIDWAL
References
Hansen, M., Lange, K. K., Stausholm, M. B., & Dela, F. (2025). Are individuals with type 2 diabetes metabolically inflexible? A systematic review and meta-analysis. Endocrinology, Diabetes & Metabolism, 8(3), e70044. https://doi.org/10.1002/edm2.70044
Koudelkova, K., Moro, C., & Gojda, J. (2025). Commentary on "Are individuals with Type 2 Diabetes metabolically inflexible? A systematic review and meta‐analysis." Endocrinology, Diabetes & Metabolism, 8(4), e70068. https://doi.org/10.1002/edm2.70068
Ludlova, M., Koudelková, K., Pallova, J., Koudelkova, B., Siklova, M., Cahova, M., Vetrovsky, T., Steffl, M., & Gojda, J. (2025). Metabolic flexibility to predict lifestyle interventions outcomes (MEPHISTO): Protocol for predictive validation study and randomized controlled trial. JMIR Research Protocols, 14, e67570. https://doi.org/10.2196/67570
Tian, X., Wang, L., Zhang, L., et al. (2025). New discoveries in therapeutic targets and drug development pathways for type 2 diabetes mellitus under the guidance of precision medicine. European Journal of Medical Research, 30, 450. https://doi.org/10.1186/s40001-025-02682-5