Why We Age: The Hidden Role of Chronic Inflammation in Accelerating Aging
Discover how chronic inflammation accelerates aging. Learn the science of inflammaging, why it’s not inevitable, and evidence-backed strategies to slow biological aging.
AGING
Dr. T.S. Didwal, M.D
1/21/202612 min read
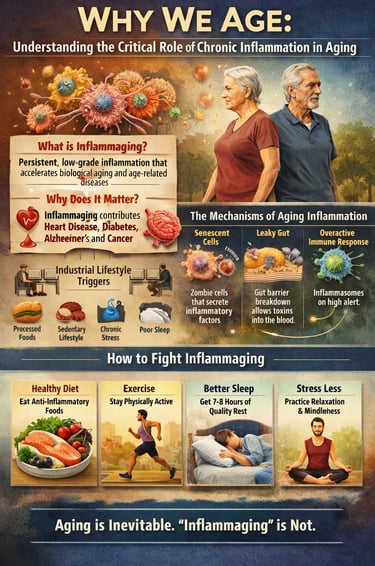

Why do we age—and why do some people age dramatically faster than others? Emerging research reveals that the true driver of biological aging isn’t simply the passage of time, but chronic inflammation, a persistent, low-grade immune activation that silently damages tissues for decades. This phenomenon, known as inflammaging, is now recognized as one of the leading inflammaging causes of cardiovascular disease, type 2 diabetes, neurodegeneration, frailty, and accelerated biological aging (Huang et al, 2025).
Unlike acute inflammation, which protects us after injury, chronic inflammation slowly chips away at cellular resilience, disrupts metabolism, impairs immunity, and accelerates DNA damage. Scientists now know that senescence and aging are deeply connected: as senescent cells accumulate, they release inflammatory molecules called SASP, creating a toxic internal environment that speeds up tissue aging (Falzone et al., 2023).
The encouraging news? Chronic inflammation is not destiny—it is highly responsive to intervention. Modern geroscience demonstrates that a targeted anti-inflammatory lifestyle can dramatically slow biological aging. Simple, evidence-based habits such as improving gut health, optimizing sleep, increasing physical activity, and reducing processed foods can meaningfully lower inflammatory markers. In fact, many leading researchers now consider lifestyle modification the most effective form of chronic inflammation treatment (Naddaf, 2025).
This also means you can reduce inflammation naturally without relying solely on medication. Diets rich in polyphenols and omega-3s, regular resistance training, stress management, and circadian-aligned sleep can all lower CRP, IL-6, and TNF-α—restoring metabolic balance and slowing the aging process (Bender et al., 2025).
Aging, therefore, is not merely a biological clock ticking away—it is a modifiable process shaped by daily choices.
Clinical Pearls
1. Think of Inflammation as a "False Alarm," Not an Enemy
In a young body, inflammation is like a fire department—it arrives, puts out the fire (infection or injury), and leaves. In aging, the "alarm" gets stuck in the ON position. This persistent, low-grade humming of the immune system wears down your healthy tissues over time.
The Message: You don’t want to "kill" inflammation; you want to help your immune system recognize when the fire is out.
2. Your Gut is the "Front Gate" of Aging
Much of the chronic inflammation we see in aging starts in the digestive tract. As we age, the lining of the gut can become slightly more permeable (often called "leaky gut"). This allows tiny bacterial fragments to slip into your bloodstream, causing your immune system to stay on high alert.
The Message: Strengthening your gut barrier with fiber and fermented foods is one of the most direct ways to "quiet" systemic inflammation.
3. Exercise is a "Molecular Cleanup Crew"
We often think of exercise for heart health or weight, but scientifically, it acts as a senolytic—a process that helps clear out "zombie cells" (senescent cells). These cells no longer divide but sit in your body secreting inflammatory chemicals. Movement helps your body identify and recycle these cellular "trash" items.
The Message: Every time you exercise, you are essentially "cleaning" your internal environment at a cellular level.
4. Stress and Sleep are Biological "Dimmer Switches"
Chronic stress and poor sleep aren't just feelings; they are biological triggers. They keep your cortisol levels high, which acts like a "dimmer switch" that turns up the volume on inflammatory genes. High-quality sleep, specifically, is when your brain’s waste-clearance system (the glymphatic system) flushes out inflammatory proteins.
The Message: Sleep is your body’s primary anti-inflammatory treatment. It is the time when your biological "software" updates and repairs itself.
5. Your "Biological Age" is Negotiable
Research in industrialized vs. traditional societies shows that while chronological age (the number of birthdays) is fixed, biological age (the state of your inflammation) is highly flexible. High inflammation markers (like CRP) are often a reflection of modern lifestyle factors—diet, inactivity, and environment—not a "side effect" of being 70 or 80.
The Message: Aging is mandatory, but "inflammaging" is largely modifiable. You have a seat at the steering wheel of your own biological clock.
Why We Age: Understanding the Critical Role of Chronic Inflammation in Aging
What Is Chronic Inflammation and Why Should You Care?
Before diving into the aging connection, let's establish what chronic inflammation actually is. Unlike acute inflammation—the redness and swelling you see after cutting your finger—chronic inflammation operates silently in the background. Your immune system remains partially activated, continuously releasing inflammatory molecules called cytokines into your bloodstream.
For decades, medical science focused on inflammation as a protective mechanism. When pathogens invade or tissue is damaged, inflammation mobilizes immune cells to the rescue. This is healthy and necessary. However, persistent low-grade inflammation creates a fundamentally different situation. Your body essentially stays in a state of alarm, even when there's no immediate threat.
Why does this matter for aging? Because this constant inflammatory state accelerates almost every age-related disease you can name: heart disease, Alzheimer's, type 2 diabetes, osteoporosis, and cancer. Understanding inflammation's role in aging is therefore crucial for anyone interested in living not just longer, but healthier
The Science of Inflammaging: Understanding Age-Associated Inflammation
What Happens in Our Bodies as We Age?
Recent research has revealed that age-associated inflammation follows surprisingly predictable patterns. As we accumulate more years, our immune cells become increasingly prone to activation. Senescent cells—cells that have stopped dividing but remain metabolically active—accumulate in tissues and continuously pump out inflammatory cytokines. Additionally, the microbiome changes, the integrity of our intestinal barrier weakens, and various tissue damage accumulates.
The convergence of these factors creates what scientists call inflammaging—a chronic, systemic state of low-grade inflammation. This isn't a disease in the traditional sense; it's a fundamental aging process that underlies many diseases.
Key Breakthrough: A Fascinating Geographic Distinction
One of the most surprising recent discoveries challenges our assumptions about whether aging and inflammation necessarily go hand-in-hand. Research has revealed something remarkable: Ageing is linked to inflammation—but primarily in industrialized nations. This geographical distinction opens entirely new perspectives on whether chronic inflammation in aging is truly unavoidable.(Naddaf, 2025)
What explains this difference? Scientists point to lifestyle factors distinctive to industrialized societies: highly processed diets, sedentary behavior, chronic stress, sleep disruption, and environmental pollutants. In contrast, populations in non-industrialized regions often maintain traditional diets rich in anti-inflammatory compounds, engage in more physical activity, and experience different stress patterns. These environmental and behavioral factors significantly influence whether aging is accompanied by the chronic inflammatory state so common in developed countries.
This discovery is profoundly important because it suggests that age-related inflammation isn't written into our genetic destiny. The high prevalence of inflammaging in industrialized nations may reflect modifiable lifestyle factors rather than inevitable aging biology.
Research Spotlight: Current Evidence on Inflammation and Aging
Study 1: Insights and Interventions in Age-Associated Inflammation
Chronic Inflammation as the Root Cause of Accelerated Aging
Huang et al .2025. synthesises current understanding of age-associated inflammation and explores emerging intervention strategies. This research provides crucial insights into how biological aging processes intersect with inflammatory pathways.
Key findings include: The study emphasizes that chronic inflammation doesn't develop randomly but follows specific molecular pathways. Senescent cells emerge as major contributors to inflammaging, releasing a cocktail of inflammatory factors that damage surrounding tissues. The research highlights that understanding these specific pathways opens doors to targeted therapeutic interventions rather than crude, broad-based approaches.
The broader significance: By mapping the mechanisms of age-related inflammation, this research establishes a scientific foundation for developing interventions that could genuinely slow aging. Rather than treating individual age-related diseases separately, targeting the underlying chronic inflammation could simultaneously address multiple conditions.
Study 2: The Geographic Reality of Inflammaging
Naddaf (2025 ), examining how aging is linked to inflammation primarily in industrialized contexts, provide a crucial reality check on aging narratives. This research demolishes the assumption that high levels of age-associated inflammation are universally inevitable.
What this means: When 80-year-olds in non-industrialized populations show dramatically lower markers of chronic inflammation compared to their counterparts in wealthy nations, it proves something fundamental: the Western pattern of inflammaging reflects lifestyle choices, not just chronological age. The inflammatory burden we accumulate is significantly influenced by diet, movement, sleep, stress management, and environmental exposures.
Practical implications: This research directly contradicts the fatalistic narrative that aging inevitably brings escalating inflammation. It demonstrates that inflammation and aging connect through modifiable pathways, making prevention and intervention strategies genuinely feasible.
Study 3: Therapeutic Strategies for Inflammation and Aging
Falzone et al. (2023) surveyed the landscape of therapeutic approaches to managing inflammation in chronic and degenerative diseases associated with aging. This work synthesizes thinking on how medical science might intervene in the inflammation-ageing axis.
Current therapeutic strategies discussed: The research examines both pharmaceutical and lifestyle-based approaches to reducing age-related inflammation. Emerging therapies targeting senescent cells, modulating immune responses, and addressing metabolic dysfunction show promise. Simultaneously, the research affirms that chronic inflammation remains highly responsive to traditional interventions: diet modification, regular physical activity, stress management, and sleep optimization.
The integration of old and new: What makes this research particularly valuable is its recognition that cutting-edge pharmaceutical interventions will ultimately complement, rather than replace, the lifestyle foundations of healthy aging. Understanding inflammaging means appreciating both emerging science and timeless health principles.
How Chronic Inflammation Accelerates Aging: The Mechanisms
Cellular Senescence and Inflammaging
Understanding why chronic inflammation accelerates aging requires examining cellular senescence. As cells age, they eventually stop dividing—a process called senescence that's actually a tumour-prevention mechanism. However, senescent cells don't simply disappear. Instead, they accumulate in tissues and secrete inflammatory cytokines, growth factors, and proteases. This secretory profile is literally called SASP—the Senescence-Associated Secretory Phenotype.
Imagine having trillions of tiny cellular factories throughout your body continuously pumping out inflammatory chemicals. This is essentially what happens in aging. The accumulation of senescent cells represents a major contributor to age-associated inflammation.
The Inflammasome and Innate Immunity
Deeper still, scientists have identified specific molecular machines called inflammasomes that become hyperactive with age. These protein complexes detect damage signals and trigger the release of inflammatory cytokines like IL-1β and IL-18. In young, healthy individuals, inflammasome activation represents an appropriate response to genuine threats. In aging, these systems become hair-trigger sensitive, firing in response to normal metabolic byproducts and minor cellular damage.
This hyperactivity of age-related inflammatory signaling cascades means that by the time we reach older age, our bodies are essentially maintaining a state of alert even during peaceful times.
Microbiome Dysbiosis and Intestinal Barrier Dysfunction
The trillions of bacteria in our gut evolve dramatically across the lifespan. In aging, we typically see reduced bacterial diversity and alterations in bacterial composition—a condition called dysbiosis. Simultaneously, the intestinal barrier becomes more permeable, allowing bacterial lipopolysaccharides (LPS) to enter circulation. These molecules are recognized as danger signals by immune cells, triggering additional chronic inflammation. This phenomenon is so characteristic that researchers coined the term "leaky gut" to describe it.
The gut-inflammation-aging connection reveals why dietary choices profoundly influence age-associated inflammation. What you eat directly shapes your microbiome, which in turn influences your inflammatory burden.
Why Industrialized Lifestyles Amplify Age-Related Inflammation
The research showing that aging is linked to inflammation specifically in industrialized nations points to several culprits:
Processed Food and Nutrient Depletion: Ultra-processed diets lack the polyphenols, fiber, and micronutrients that support immune regulation and gut health. They're simultaneously high in omega-6 polyunsaturated fatty acids and low in omega-3s, skewing the inflammatory balance toward pro-inflammatory states
.
Sedentary Behavior: Physical inactivity removes one of the most powerful anti-inflammatory stimuli available. Exercise suppresses multiple inflammatory pathways simultaneously and promotes the expansion of anti-inflammatory immune cell populations.
Chronic Psychological Stress: Modern life delivers unprecedented psychological stressors. Stress hormones chronically activate immune cells, directly contributing to low-grade inflammation that persists regardless of whether any real threat exists.
Sleep Disruption: Industrial society's schedules and artificial lighting profoundly disrupt circadian rhythms. Poor sleep independently amplifies inflammatory signaling and impairs immune regulation.
Environmental Exposures: Air pollution, endocrine-disrupting chemicals, and other modern environmental stressors trigger immune activation. Many of these exposures are unique to industrialized settings.
When you combine all these factors, it becomes clear why populations in industrialized nations show elevated age-associated inflammation even at younger ages. It's not aging causing inflammation—it's lifestyle creating the inflammatory state that accelerates aging.
The Disease Consequences: How Inflammaging Drives Age-Related Pathology
Chronic inflammation serves as a common pathway connecting diverse age-related diseases. Understanding this connection explains why addressing age-related inflammation could simultaneously combat multiple conditions.
Cardiovascular Disease: Inflammation damages endothelial cells, promotes atherosclerotic plaque formation, and makes plaques more likely to rupture. Elevated inflammatory markers predict cardiovascular events independently of cholesterol levels.
Neurodegenerative Disease: In the brain, chronic microglial activation—a neuroinflammatory state—contributes to amyloid accumulation and tau pathology. The inflammatory environment accelerates cognitive decline.
Metabolic Dysfunction: Chronic inflammation interferes with insulin signaling and promotes weight gain while reducing metabolic flexibility. This creates a vicious cycle where metabolic dysfunction amplifies inflammation.
Bone Loss: Inflammatory cytokines stimulate osteoclasts while inhibiting osteoblasts, resulting in net bone loss. Osteoporosis reflects decades of accumulated age-related inflammatory damage.
Cancer: Chronic inflammation promotes tumor initiation, progression, and metastasis through multiple mechanisms. The inflammatory microenvironment both promotes cancer development and suppresses anti-tumor immunity.
This interconnected web demonstrates why inflammation and aging have become central to modern gerontology.
Proven Interventions: Reducing Age-Related Inflammation
The encouraging news from recent research is that chronic inflammation responds dramatically to intervention. You don't need to accept inflammaging as inevitable.
Dietary Approaches
Mediterranean and plant-rich diets consistently demonstrate anti-inflammatory effects. These diets are rich in polyphenols, fiber, and omega-3 fatty acids while low in refined carbohydrates and processed foods. They modify the microbiome in anti-inflammatory directions and reduce circulating inflammatory markers.
Intermittent fasting and time-restricted eating appear to reduce age-associated inflammation through multiple mechanisms, including enhanced autophagy and microbiome modifications.
Elimination of specific inflammatory triggers like refined seed oils and processed sugar can meaningfully reduce inflammatory burden.
Physical Activity
Regular exercise represents perhaps the most potent anti-inflammatory intervention available. Aerobic exercise, resistance training, and even low-intensity movement all suppress low-grade inflammation. The mechanisms involve both reduced inflammatory signaling and enhanced anti-inflammatory immune cell populations.
Sleep Optimization
Prioritizing 7-9 hours of consistent, high-quality sleep directly reduces inflammatory markers. Sleep deprivation amplifies inflammasome activation and impairs immune regulation.
Stress Management
Chronic stress management through meditation, breathwork, nature exposure, and social connection meaningfully reduces chronic inflammation. These aren't merely "feel-good" measures—they're biological interventions with measurable effects on inflammatory markers.
Targeted Supplementation
While no supplement replaces lifestyle fundamentals, certain compounds show evidence for reducing age-related inflammation: omega-3 fatty acids, curcumin, quercetin, and resveratrol all demonstrate anti-inflammatory properties in research settings.
Emerging Pharmaceutical Approaches
Researchers are developing senolytic drugs that selectively eliminate senescent cells, potentially providing a direct intervention against inflammaging. Additionally, therapeutic agents targeting specific inflammasome components show promise in preclinical and early clinical work
.
Frequently Asked Questions About Chronic Inflammation and Aging
Q: Can you completely eliminate age-related inflammation? A: While you can't achieve zero inflammation, you can dramatically reduce the excessive burden of chronic inflammation characteristic of aging in industrialized populations. Many people successfully normalize inflammatory markers through comprehensive lifestyle modification.
Q: At what age does inflammaging typically begin? A: Age-associated inflammation begins accumulating relatively early—often measurable in the 30s and 40s—but accelerates notably after 60. However, the rate of accumulation depends heavily on lifestyle factors.
Q: How can I measure my inflammatory status? A: Blood tests measuring C-reactive protein (CRP), interleukin-6 (IL-6), and tumor necrosis factor-alpha (TNF-α) provide useful snapshots of low-grade inflammation. Discuss testing options with your healthcare provider.
Q: Is inflammation always bad? A: No. Acute inflammation in response to injury or infection is protective and necessary. The problem is persistent, non-resolving chronic inflammation that serves no protective purpose.
Q: Can lifestyle changes really reduce age-related inflammation at my age? A: Yes. Research consistently shows that comprehensive lifestyle modifications reduce inflammatory markers even in older adults. It's never too late to begin.
Q: How long does it take to see improvements in inflammatory markers? A: Changes in chronic inflammation can become measurable in weeks to months with consistent lifestyle modification, though deeper tissue-level changes take longer.
Key Takeaways: Essential Points About Inflammation and Aging
Chronic inflammation drives aging - Rather than aging causing inflammation, chronic low-grade inflammation accelerates aging and age-related diseases.
Inflammaging is not inevitable - The high prevalence of age-associated inflammation in industrialized nations reflects lifestyle factors rather than genetic destiny. Populations in non-industrialized areas show dramatically lower inflammatory burden despite similar ages.
Multiple pathways amplify age-related inflammation - Senescent cells, dysbiotic microbiomes, intestinal barrier dysfunction, and hyperactive innate immune signaling all contribute to inflammaging.
Lifestyle factors create modern inflammaging - Processed diets, sedentary behavior, chronic stress, poor sleep, and environmental exposures characteristic of industrialized life directly amplify age-related inflammation.
Intervention is highly effective - Chronic inflammation responds dramatically to diet modification, regular physical activity, sleep optimization, stress management, and emerging pharmaceutical approaches.
Multiple diseases share a common inflammatory root - Understanding inflammation and aging as interconnected explains why addressing inflammation simultaneously improves multiple age-related conditions.
Early intervention matters - While people of any age can benefit from inflammation-reducing interventions, beginning earlier provides compounding benefits over decades.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Individual circumstances vary, and treatment decisions should always be made in consultation with qualified healthcare professionals.
Related Articles
Targeting Inflammaging: A Precision Strategy for Healthier Aging and Longevity | DR T S DIDWAL
Exercise and Longevity: The Science of Protecting Brain and Heart Health as You Age | DR T S DIDWAL
The Science of Healthy Brain Aging: Microglia, Metabolism & Cognitive Fitness | DR T S DIDWAL
The Aging Muscle Paradox: How Senescent Cells Cause Insulin Resistance and The Strategies to Reverse It | DR T S DIDWAL
VO2 Max & Longevity: The Ultimate Guide to Living Longer | DR T S DIDWAL
Waist-Calf Ratio: The Longevity Metric Most People Aren’t Tracking | DR T S DIDWAL
Blue Zones Secrets: The 4 Pillars of Longevity for a Longer, Healthier Lifepost | DR T S DIDWAL
Anabolic Resistance: Why Muscles Age—and How to Restore Their Growth Response | DR T S DIDWAL
Author’s Note
As a consultant physician and medical researcher, my work is rooted in evidence-based practice and a deep commitment to translating complex scientific findings into practical, actionable guidance for patients and readers. Chronic inflammation, metabolic dysfunction, and accelerated aging are not isolated phenomena—they are interconnected biological processes shaped profoundly by lifestyle, environment, and cellular health.
This article synthesizes current insights from cutting-edge research, including emerging 2024–2025 literature on senescence biology, mitochondrial function, gut dysbiosis, and inflammaging pathways. The goal is not only to explain the mechanisms behind chronic inflammation, but also to empower individuals with proven strategies to reduce inflammation naturally and adopt an anti-inflammatory lifestyle that supports long-term vitality, disease prevention, and healthy aging.
I believe that aging is not merely a chronological progression but a modifiable biological process. The science of geroprotection—through nutrition, exercise, sleep, stress regulation, and targeted medical interventions—offers a powerful opportunity to reshape health trajectories across the lifespan. Every chapter I write, whether for clinical education or public awareness, is grounded in the same principle: health should be informed by science and guided by sustainability.
Thank you for taking the time to engage with this content. I hope it inspires you to explore, question, and take proactive steps toward better health.
References
Falzone, L., Candido, S., Docea, A. O., & Calina, D. (2023). Editorial: Inflammation and aging in chronic and degenerative diseases: Current and future therapeutic strategies. Frontiers in Pharmacology, 13, 1122786. https://doi.org/10.3389/fphar.2022.1122786
Huang, H., Ren, J., & Liu, G. H. (2025). Insights and interventions in age-associated inflammation. Current Opinion in Genetics & Development, 91, 102306. https://doi.org/10.1016/j.gde.2024.102306
Naddaf, M. (2025). Ageing is linked to inflammation - but only in the industrialized world. Nature, 10.1038/d41586-025-02085-w. Advance online publication. https://doi.org/10.1038/d41586-025-02085-w
Bender, E.C., Tareq, H.S. & Suggs, L.J. Inflammation: a matter of immune cell life and death. npj Biomed. Innov. 2, 7 (2025). https://doi.org/10.1038/s44385-025-00010-4