Combined Aerobic–Resistance Training as the Gold Standard for Inflammation Reduction in Type 2 Diabetes
New 2026 research reveals that not all exercise is equal for Type 2 Diabetes. Discover why combined training and resistance exercise outperform traditional cardio in reducing inflammatory markers like CRP and IL-6.
EXERCISEDIABETES
Dr. T.S. Didwal, M.D.(Internal Medicine)
2/13/202612 min read
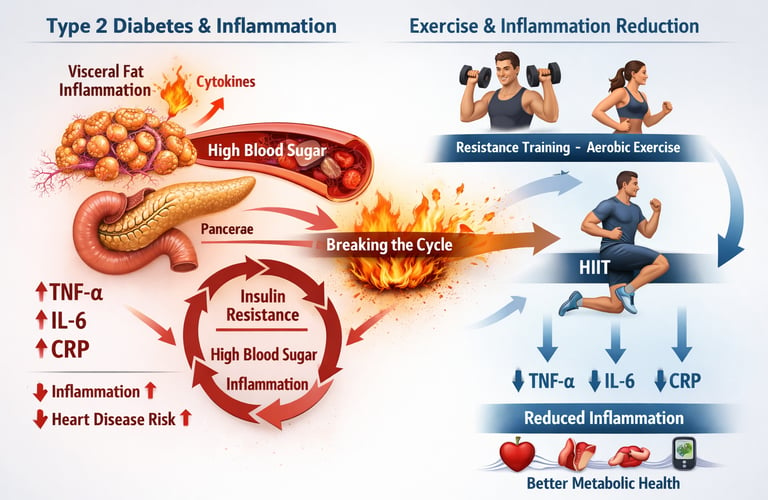
Type 2 diabetes mellitus (T2DM) is no longer viewed solely as a disorder of glucose metabolism—it is increasingly recognized as a state of chronic low-grade systemic inflammation. Elevated inflammatory markers such as tumor necrosis factor-alpha (TNF-α), interleukin-6 (IL-6), and C-reactive protein (CRP) are not just laboratory abnormalities; they actively drive insulin resistance, endothelial dysfunction, and accelerated cardiovascular disease (Khalafi et al., 2025). In individuals with overweight and obesity, excess visceral adipose tissue behaves like an endocrine organ, releasing pro-inflammatory cytokines that perpetuate metabolic dysfunction (Tan et al., 2024).
This inflammatory burden creates a vicious cycle: inflammation worsens insulin signaling, impaired insulin signaling elevates blood glucose, and hyperglycemia further amplifies oxidative and inflammatory stress. Breaking this cycle is central to modern diabetes management. While pharmacologic therapies target glucose pathways, emerging evidence suggests that exercise functions as a powerful immunometabolic intervention, capable of directly reducing systemic inflammation (Dong et al., 2026).
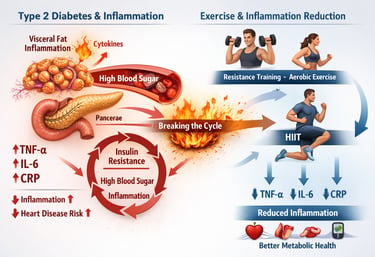
Recent systematic reviews and network meta-analyses demonstrate that not all exercise is equal. Resistance training, combined with aerobic-resistance programs, and high-intensity interval training (HIIT) show differing magnitudes of anti-inflammatory effects, with some modalities producing sustained reductions in TNF-α, IL-6, and CRP independent of weight loss (Kadoglou et al., 2025).
The question is no longer whether exercise helps—but which type of exercise most effectively extinguishes the inflammatory fire underlying type 2 diabetes.
Clinical pearls .
1. The "Metabolic Multiplier" Effect
Resistance training (RT) induces skeletal muscle hypertrophy, which increases the expression of glucose transporter type 4 (GLUT4) and elevates resting metabolic rate (RMR).
Think of muscle as "active tissue." When you lift weights or use resistance bands, you are building a bigger engine for your body. This bigger engine burns more sugar even while you are sleeping, helping to naturally lower your A1c and snuff out the "hidden fire" of inflammation.
2. HIIT for the Time-Crunched Inflammatory Response
High-Intensity Interval Training (HIIT) provides a potent stimulus for rapid reductions in CRP and TNF-$\alpha$ by improving mitochondrial biogenesis and cardiorespiratory fitness ($VO_2$ max) in shorter durations than Moderate-Intensity Continuous Training (MICT).
You don't need to spend an hour on a treadmill to see results. Short bursts of higher-effort exercise (like brisk uphill walking for 1 minute followed by 2 minutes of slow walking) can "reset" your immune system faster than long, slow workouts. It’s about quality and intensity over total minutes.
3. The Superiority of "The Hybrid Approach"
Combined training (Aerobic + Resistance) demonstrates superior efficacy in network meta-analyses because it addresses both systemic vascular inflammation (via aerobic) and peripheral insulin sensitivity (via resistance).
If you only walk, you’re missing half the benefit. If you only lift weights, you’re missing the other half. The "Gold Standard" is a mix. Combining both types of exercise acts like a double-layered shield against the complications of diabetes
4. Muscle as an "Endocrine Organ" (Myokines)
Contracting skeletal muscles release "myokines" like IL-6 (which, in an exercise context, acts anti-inflammatory) and IL-10, which directly inhibit the pro-inflammatory effects of TNF-alpha produced by visceral fat.
Patient-Friendly Tone: Your muscles are actually a pharmacy! Every time they contract during exercise, they release natural medicine into your bloodstream that travels through your body to heal inflammation and protect your heart.
5. The "Gender Gap" in Resistance Training
Women with obesity often show a more pronounced anti-inflammatory response to progressive resistance training (PRT) due to specific shifts in the androgen-to-estrogen ratio and fat distribution changes.
For women managing T2DM, strength training is a secret weapon. It is particularly effective at targeting the stubborn inflammation associated with hormonal changes and body composition, making it just as important—if not more so—than traditional cardio.
6. Consistency Trumps Intensity for CRP
Long-term reduction in C-Reactive Protein (CRP) is more closely correlated with exercise adherence and frequency rather than a single high-intensity "bout," suggesting that cumulative metabolic stress is the driver of systemic change.
You don't have to be an athlete to win this battle. The research shows that showing up 3 to 4 times a week for a moderate session is better for your inflammation levels than doing one "heroic" workout once a week. Consistency is the key that unlocks the anti-inflammatory vault.
Understanding Exercise, Inflammation, and Diabetes Management
Inflammation is like a hidden fire burning inside people with type 2 diabetes mellitus, particularly those dealing with overweight and obesity. This chronic inflammation triggers a cascade of health problems, from insulin resistance to cardiovascular complications. But here's where exercise comes in as your secret weapon.
In this comprehensive guide, we'll explore four groundbreaking research studies that illuminate exactly which exercise types—whether resistance training, aerobic exercise, combined training, or high-intensity interval training (HIIT)—work best for reducing inflammation in people with type 2 diabetes and obesity-related inflammation.
Study 1: Dong, Zhang & Lu (2026) — Comparative Effects of Different Exercise Types in Type 2 Diabetes with Overweight and Obesity
The most recent research from Dong, Zhang, and Lu (2026) provides a cutting-edge systematic review and network meta-analysis examining how different exercise interventions affect inflammatory markers in individuals with type 2 diabetes mellitus who are overweight or obese. This study synthesized data from multiple randomized controlled trials to create a comprehensive comparison of various exercise types.
The research team meticulously analyzed studies focusing on how aerobic exercise, resistance training, combined exercise programs, and other physical activity interventions influence markers like inflammatory cytokines and systemic inflammation.
Key Findings and Takeaways
Resistance training demonstrated particularly potent effects on reducing inflammatory markers in individuals with type 2 diabetes and obesity
Combined training programs (mixing aerobic and resistance exercise) showed superior efficacy compared to single-modality approaches
The reduction in inflammatory biomarkers directly correlated with improvements in insulin sensitivity and metabolic health
Exercise duration and intensity both played critical roles in the anti-inflammatory response
Participants who maintained consistent exercise adherence experienced more substantial reductions in systemic inflammation
For people with type 2 diabetes, this study underscores that a one-size-fits-all approach to exercise simply doesn't work. Instead, a personalized exercise strategy combining multiple exercise modalities produces the best anti-inflammatory effects and metabolic improvements.
Study 2: Khalafi et al. (2025) — Comparative Efficacy of Different Exercise Modes on Inflammatory Markers
Khalafi and colleagues (2025) conducted an extensive pairwise and network meta-analysis in Obesity Reviews, comparing the efficacy of different exercise modes for managing inflammatory markers specifically in type 2 diabetes mellitus patients. This sophisticated meta-analytical approach allowed researchers to not only compare exercises head-to-head but also rank them by overall effectiveness.
The study included numerous randomized controlled trials examining how aerobic training, resistance exercise, interval training, and other physical activity protocols influence critical inflammatory biomarkers including TNF-α, IL-6, and CRP.
The Khalafi et al. (2025) research provides several critical takeaways:
High-intensity interval training (HIIT) emerged as exceptionally effective for rapidly reducing inflammatory markers despite shorter exercise duration compared to traditional steady-state aerobic exercise
Resistance training consistently demonstrated significant benefits for reducing pro-inflammatory cytokines and improving metabolic parameters
Combined exercise interventions that incorporated both aerobic and resistance components yielded the most comprehensive reductions in systemic inflammation
The intensity of exercise appeared more influential than volume in determining anti-inflammatory effects
Cardiovascular function improvements occurred alongside inflammatory marker reduction, suggesting multi-system benefits
For people managing type 2 diabetes, this research suggests that you don't necessarily need to spend hours exercising. Strategic, high-intensity exercise interventions can deliver impressive anti-inflammatory benefits in shorter timeframes, making exercise adherence more achievable for busy individuals.
Study 3: Tan et al. (2024) — Exercise Types and Inflammatory Markers in Women with Overweight and Obesity
Published in the Journal of Science and Medicine in Sport, Tan, Yan, Zhang, and colleagues (2024) conducted a systematic review and network meta-analysis with a specific focus on women with overweight and obesity. This research is particularly valuable because inflammatory responses to exercise can vary between sexes due to hormonal and metabolic differences.
The study examined randomized controlled trials investigating how various exercise protocols influenced inflammatory biomarkers in female participants, considering factors like menopausal status, hormonal profiles, and body composition.
Key Findings and Takeaways
Women with overweight and obesity showed particularly strong anti-inflammatory responses to resistance training compared to aerobic-only approaches
Combined training programs demonstrated superior effectiveness for reducing multiple inflammatory markers simultaneously
Progressive resistance exercise with adequate recovery periods produced sustained reductions in inflammatory cytokines over time
Exercise adherence rates among women improved when programs incorporated varied exercise modalities rather than repetitive single-type routines
Body composition improvements (particularly lean muscle gain) correlated directly with inflammatory marker reduction
This study highlights that women with type 2 diabetes and obesity-related inflammation may benefit especially from strength training and resistance exercises. These modalities not only reduce inflammatory markers but also build metabolic muscle tissue, creating a powerful dual benefit for long-term metabolic health and inflammatory control.
Study 4: Kadoglou et al. (2025) — Anti-Inflammatory Effects of Resistance Training in Type 2 Diabetes
The most recent contribution from Kadoglou, Georgiou, Balaskas, and team (2025), published in Biomolecules, provides a focused systematic review and meta-analysis dedicated specifically to resistance training and its anti-inflammatory effects in type 2 diabetes patients. This targeted approach allows for deeper examination of how strength training works at the cellular and systemic levels.
The research synthesized evidence from multiple randomized controlled trials examining various resistance training protocols, from traditional weight lifting to bodyweight resistance exercises.
Key Findings and Takeaways
Resistance training produces sustained reductions in pro-inflammatory markers including TNF-α, IL-6, and CRP in type 2 diabetes patients
Progressive resistance exercise triggers anti-inflammatory immune responses through multiple mechanisms, including increased muscle-derived IL-10 (an anti-inflammatory cytokine)
Strength gains from resistance training create a "metabolic benefit multiplier"—as people gain muscle, their resting metabolic rate increases, further reducing inflammatory burden
Resistance training improves glycemic control while simultaneously reducing systemic inflammation, addressing both major complications of type 2 diabetes
Even moderate-intensity resistance exercise produces meaningful anti-inflammatory effects, making this approach accessible to people across different fitness levels
The Kadoglou research illuminates why resistance training works so effectively. When you perform resistance exercise, your muscles produce anti-inflammatory mediators and increase their sensitivity to insulin, creating a powerful metabolic reset that reduces the inflammatory environment associated with type 2 diabetes.
Comparative Analysis: Which Exercise Type Works Best?
Based on all four research studies, here's how different exercise types stack up:
Resistance Training
Consistently ranked as highly effective across all four studies
Produces the most sustainable inflammatory marker reduction over time
Creates lasting metabolic improvements through muscle tissue gains
Particularly effective for women with obesity (per Tan et al., 2024)
Demonstrates powerful benefits even at moderate intensity (per Kadoglou et al., 2025)
Combined Training (Aerobic + Resistance)
Ranked as most effective in multiple studies
Addresses both cardiovascular fitness and metabolic health
Produces comprehensive reductions in multiple inflammatory markers simultaneously
Improves overall exercise adherence due to variety
High-Intensity Interval Training (HIIT)
Exceptionally efficient for time-constrained individuals
Produces rapid inflammatory marker reduction (per Khalafi et al., 2025)
May enhance insulin sensitivity more quickly than traditional aerobic exercise
Requires careful progression and monitoring in deconditioned individuals
Aerobic Exercise
Beneficial but often less effective than resistance training alone
Remains important for cardiovascular health
Works well as part of combined training protocols
The Winner: Combined Training with Progressive Resistance
When synthesizing findings across all four systematic reviews and meta-analyses, combined exercise programs emphasizing progressive resistance training emerge as the most comprehensive approach. This makes intuitive sense: by combining strength building (which creates metabolic muscle) with cardiovascular training (which improves heart health), you address multiple inflammatory pathways simultaneously.
The Science Behind Exercise and Inflammation Reduction
Understanding Inflammatory Markers in Type 2 Diabetes
TNF-α (Tumour Necrosis Factor-alpha): A pro-inflammatory cytokine that increases insulin resistance
IL-6 (Interleukin-6): An inflammatory signaling molecule that contributes to systemic inflammation
CRP (C-Reactive Protein): A marker of systemic inflammation strongly associated with cardiovascular disease risk
In type 2 diabetes, elevated inflammatory markers create a vicious cycle: inflammation impairs insulin signaling, which raises blood sugar, which triggers more inflammation.
How Exercise Interrupts the Inflammation Cycle
Exercise interrupts this cycle through multiple mechanisms:
Muscle-Derived Anti-Inflammatory Mediators: During exercise, muscles release myokines (muscle-derived signaling molecules) that reduce systemic inflammation
Improved Insulin Sensitivity: Exercise makes cells respond better to insulin, reducing the metabolic stress that triggers inflammation
Metabolic Muscle Building: Resistance training builds lean muscle mass, which dramatically reduces metabolic inflammation
Visceral Fat Reduction: All exercise types reduce abdominal fat, a major source of inflammatory compounds
Immune System Modulation: Appropriate exercise intensity triggers anti-inflammatory immune responses
Practical Implementation: How to Start Your Anti-Inflammatory Exercise Program
Getting Started with Resistance Training
If you're new to resistance exercise, begin with:
Bodyweight exercises (squats, push-ups, lunges)
Light resistance bands
Machines (which provide safety and ease of use)
Progressive increases in load and intensity over weeks and months
Building Your Combined Training Program
A balanced weekly exercise prescription for type 2 diabetes management might include:
2-3 days of resistance training (targeting major muscle groups)
2-3 days of aerobic activity (brisk walking, cycling, swimming)
1-2 sessions of flexibility and recovery
Important Considerations
Consistency matters more than intensity—sustainable exercise adherence outweighs sporadic intense workouts
Individual variability exists—some people respond more dramatically to specific exercise modalities
Medical supervision is important when starting, especially if you're on diabetes medications
Gradual progression prevents injury and promotes long-term sustainability
Frequently Asked Questions (FAQs)
Q: How quickly will I see improvements in inflammatory markers?
A: Most research shows measurable reductions in inflammatory markers within 4-8 weeks of consistent exercise participation. Some inflammatory cytokines respond faster than others, with CRP often showing improvements within weeks.
Q: Is it ever too late to start exercising if I have type 2 diabetes?
A: Absolutely not. Studies included participants across wide age ranges, and benefits appear consistent regardless of age. Always consult your healthcare provider before starting a new exercise program.
Q: Do I need an expensive gym membership?
A: No. Resistance training can be accomplished with bodyweight exercises, resistance bands, or household items. Effective exercise depends on consistency and appropriate intensity, not facility quality.
Q: Which exercise type produces the fastest inflammatory marker reduction?
A: According to Khalafi et al. (2025), high-intensity interval training produces rapid results. However, resistance training produces the most sustainable long-term reductions.
Q: Can exercise alone manage my type 2 diabetes?
A: Exercise is powerful but most effective as part of comprehensive management including nutrition, stress management, and sleep. Always work with your healthcare team.
Q: Why is resistance training particularly beneficial for women with obesity?
A: According to Tan et al. (2024), resistance training uniquely builds lean muscle mass, which increases resting metabolic rate and improves insulin sensitivity—effects particularly pronounced in women.
Q: How much exercise do I need to see inflammatory marker improvements?
A: The Khalafi et al. (2025) research suggests that even moderate-intensity exercise produces benefits. You don't need marathon-length workouts—consistency and appropriate intensity matter most.
Q: What if I have joint problems or physical limitations?
A: Water-based resistance exercise, chair-based workouts, and modified resistance training can provide anti-inflammatory benefits even for people with physical limitations. Consult a physical therapist for personalized modifications.
Key Takeaways: What You Need to Know
Multiple exercise types reduce inflammation, but combined training emphasizing resistance produces the most comprehensive benefits
Resistance training alone produces significant anti-inflammatory effects and may be particularly valuable for women with obesity and type 2 diabetes
High-intensity interval training offers time-efficient inflammatory marker reduction for motivated individuals
Exercise consistency and personalization matter more than following a generic program
Benefits appear within 4-8 weeks with consistent participation
Exercise-induced inflammation reduction directly improves insulin sensitivity and metabolic health
Progressive resistance training creates sustainable anti-inflammatory effects through muscle tissue gains
Moderate-intensity exercise produces meaningful benefits—you don't need extreme intensity
Individual responses vary—working with healthcare providers helps identify your optimal exercise prescription
Long-term sustainability depends on finding an exercise approach you genuinely enjoy
Call to Action: Take Control of Your Inflammatory Health
The research is clear: exercise is one of the most powerful tools for reducing inflammatory markers in type 2 diabetes. You don't need to be a fitness expert or have access to fancy equipment—you simply need to start.
Author’s Note
As a clinician in internal medicine and a long-standing student of metabolic science, I have witnessed firsthand how type 2 diabetes is too often reduced to a single number—HbA1c. Yet beneath dysglycemia lies a far more complex and clinically significant process: chronic low-grade systemic inflammation. Elevated inflammatory mediators such as TNF-α, IL-6, and CRP are not incidental findings; they are active drivers of insulin resistance, endothelial dysfunction, and cardiometabolic progression.
This article was written to bridge a critical gap between emerging immunometabolic research and practical clinical application. The studies discussed here—systematic reviews and network meta-analyses—represent some of the highest tiers of evidence currently available in exercise science. However, data alone does not change outcomes. Translation into actionable strategies does.
My goal was to synthesize current evidence into a clear, clinically meaningful framework that empowers patients and informs healthcare professionals alike. Exercise is not merely a lifestyle recommendation—it is a biologically potent intervention capable of modulating inflammatory pathways, improving insulin sensitivity, and restoring metabolic resilience.
Importantly, this discussion does not replace individualized medical care. Exercise prescriptions must be tailored to comorbidities, medications, functional capacity, and patient preferences.
If this article encourages even one individual to view movement not as a burden but as a therapeutic tool, then it has achieved its purpose. Science continues to evolve, but one principle remains consistent: appropriately prescribed physical activity is one of the most powerful anti-inflammatory strategies available in modern medicine.
Medical Disclaimer
The information in this article, including the research findings, is for educational purposes only and does not constitute medical advice, diagnosis, or treatment. Before starting aN exercise program, you must consult with a qualified healthcare professional, especially if you have existing health conditions (such as cardiovascular disease, uncontrolled hypertension, or advanced metabolic disease). Exercise carries inherent risks, and you assume full responsibility for your actions. This article does not establish a doctor-patient relationship.
Related Articles
Bone as an Endocrine Organ: Does Osteocalcin Influence Weight Regulation? | DR T S DIDWAL
The Metabolic Engine: Why Lower Body Strength Is Central to Fat Oxidation | DR T S DIDWAL
How Exercise Rewires Metabolism: Molecular Control of Lipolysis and Lipid Metabolism | DR T S DIDWAL
How to Build a Disease-Proof Body: Master Calories, Exercise & Longevity | DR T S DIDWAL
References
Dong, M., Zhang, X., & Lu, S. (2026). Comparative effects of different exercise types on inflammatory markers in type 2 diabetes mellitus patients with overweight and obesity: A systematic review and network meta-analysis. BMC Endocrine Disorders. https://doi.org/10.1186/s12902-026-02193-2
Kadoglou, N. P. E., Georgiou, C., Balaskas, N., Panayiotou, C., Vardas, M., Mitsis, A., & Antonopoulos, C. N. (2025). The anti-inflammatory effects of resistance training in patients with type 2 diabetes: A systematic review and meta-analysis. Biomolecules, 15(10), 1417. https://doi.org/10.3390/biom15101417
Khalafi, M., Habibi Maleki, A., Symonds, M. E., Azali Alamdari, K., Ehsanifar, M., & Rosenkranz, S. K. (2025). Comparative efficacy of different exercise modes on inflammatory markers in patients with type 2 diabetes mellitus: A systematic review with pairwise and network meta-analyses. Obesity Reviews, 26(10), Article e13954. https://doi.org/10.1111/obr.13954
Tan, L., Yan, W., Zhang, B., Zhao, Z., Lipowski, M., & Ossowski, Z. (2024). Comparative efficacy of different exercise types on inflammatory markers in women with overweight and obesity: A systematic review and network meta-analysis of randomized controlled trials. Journal of Science and Medicine in Sport, 27(7), 458–465. https://doi.org/10.1016/j.jsams.2024.03.007