Bone as an Endocrine Organ: Does Osteocalcin Influence Weight Regulation?
Learn how osteocalcin, a bone-derived hormone, may affect weight regulation, metabolism, and insulin sensitivity in humans.
DIABETESMETABOLISM
Dr. T.S. Didwal, M.D.(Internal Medicine)
2/12/202613 min read
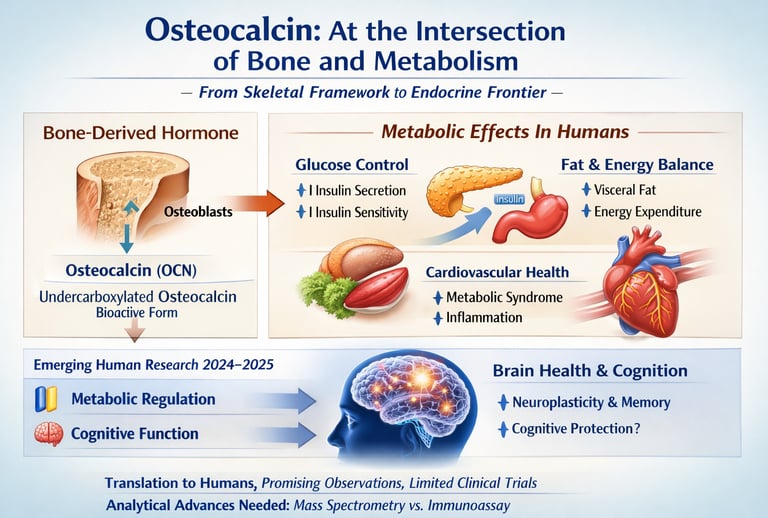
For much of modern medicine, bone was viewed primarily as a structural scaffold—an inert framework providing mechanical stability and mineral storage. That paradigm has shifted dramatically. Over the past two decades, and increasingly through 2024–2025 research, bone has emerged as a dynamic endocrine organ, capable of influencing glucose metabolism, energy balance, cardiovascular risk, and even brain function. At the center of this transformation is osteocalcin, a peptide hormone synthesized by osteoblasts that circulates systemically and interacts with multiple peripheral tissues (Determe et al., 2025; Nowicki & Jakubowska-Pietkiewicz, 2024).
Experimental models demonstrate that osteocalcin enhances insulin secretion, improves insulin sensitivity, and modulates energy expenditure. However, while murine studies show robust metabolic effects, translation to human physiology has been more nuanced. Observational human data consistently report inverse associations between circulating osteocalcin—particularly undercarboxylated osteocalcin—and type 2 diabetes risk and metabolic syndrome (Martiniakova et al., 2024; Consolim-Colombo & Lopes, 2025). Yet interventional trials remain limited, and receptor-mediated mechanisms such as GPRC6A signaling are still under investigation in human tissues.
Similarly, emerging data suggest osteocalcin may cross the blood–brain barrier and influence cognitive pathways, but clinical validation in neurodegenerative disease is preliminary (Ding et al., 2025). Analytical variability across immunoassays further complicates interpretation, underscoring the importance of standardised mass spectrometry–based measurements (Determe et al., 2025).
Thus, osteocalcin represents not a completed revolution, but an evolving frontier—where bone biology intersects with metabolic and neurological medicine, guided by growing but carefully interpreted human evidence.
Clinical pearls
1. The Paradox of Carboxylation
While carboxylated osteocalcin (cOCN) is essential for bone mineralization and structural integrity, it is the undercarboxylated form (ucOCN) that serves as the bioactive hormone. Clinicians must recognize that "bone health" and "metabolic health" are driven by two different states of the same protein.
Think of osteocalcin like a battery. When it is "plugged into" your bones, it makes them strong. But when it is "unplugged" and floating in your blood, it acts like a hormone that tells your body how to burn sugar and stay sharp. You need both states for total health.
2. The GPRC6A Receptor Cross-Talk
The systemic effects of ucOCN are mediated primarily through the GPRC6A receptor, found in pancreatic beta cells, Leydig cells, and skeletal muscle. This receptor acts as a metabolic "master switch," making osteocalcin a key player in the bone-pancreas-testis endocrine axis.
Your bones are constantly "talking" to your pancreas and muscles using a special chemical signal. When this signal reaches your organs, it flips a switch that helps your body produce insulin and build muscle more effectively.
3. Blood-Brain Barrier (BBB) Permeability
Unlike many peripheral hormones, ucOCN is capable of crossing the Blood-Brain Barrier. It binds to neurons in the hippocampus, stimulating the synthesis of neurotransmitters (like dopamine and serotonin) and enhancing Brain-Derived Neurotrophic Factor (BDNF) expression.
Most things in your blood are blocked from entering your brain, but osteocalcin has a "backstage pass." Once inside, it helps your brain cells grow and communicate, which is why healthy bones are now being linked to better memory and a lower risk of dementia.
4. Exercise Intensity and Osteoblast Mechanical Loading
High-intensity mechanical loading (resistance training or high-impact plyometrics) is required to trigger significant bone remodeling. This process activates osteoclasts to create an acidic environment that "de-carboxylates" osteocalcin, releasing the bioactive ucOCN into the bloodstream more effectively than low-impact aerobic activity.
To get the metabolic benefits of your bones, you have to "challenge" them. While walking is great, lifting weights or doing high-impact movements (like jumping) puts more pressure on your bones. This pressure acts like a "squeeze," releasing more of the health-boosting osteocalcin into your system.
5. The Vitamin K2 "Traffic Cop"
Vitamin K2 (specifically MK-7) is the essential cofactor for gamma-glutamyl carboxylase. Without adequate K2, osteocalcin cannot be properly carboxylated to stay in the bone matrix, leading to "calcium paradox" issues where calcium migrates from the bones into the arterial walls.
Vitamin K2 acts like a traffic cop for calcium. It makes sure osteocalcin stays in your bones to keep them strong. If you don't have enough K2, calcium can get "lost" and end up in your arteries, where it doesn't belong, instead of staying in your skeleton.
6. Mass Spectrometry vs. Standard Immunoassays
Traditional ELISA and ECLIA immunoassays often lack the specificity to distinguish between ucOCN and cOCN fragments. For precise metabolic staging, LC-MS/MS (Liquid Chromatography-Mass Spectrometry) is the gold standard, as it provides absolute quantification of the bioactive undercarboxylated form.
Standard blood tests for bone health can be a bit "blurry." They see the whole protein but can't tell the difference between the active and inactive parts. Newer, high-tech lab tests act like a high-definition microscope, giving your doctor a much clearer picture of how your bones are affecting your metabolism.
Osteocalcin: A Bone Protein with Multiple Endocrine Functions
For decades, bone was considered primarily a structural tissue—a static framework supporting our bodies. However, cutting-edge research from 2025 has fundamentally transformed our understanding of bone as a dynamic endocrine organ. At the center of this revolution is osteocalcin, a bone-derived protein that extends far beyond skeletal function to regulate glucose metabolism, cardiovascular health, and even neurological function.
This comprehensive guide explores the latest 2025 research on osteocalcin's multiple endocrine functions, synthesizing findings from leading international researchers including Determe, Hauge, Ding, and colleagues. Whether you're a healthcare professional, researcher, or patient seeking to understand how bone health connects to metabolic disease, this article provides evidence-based insights into one of medicine's most exciting discoveries.
What is Osteocalcin? Understanding the Bone-Derived Factor
Osteocalcin (OCN) is a bone matrix protein synthesized primarily by osteoblasts during bone formation. Its name derives from its abundance in bone tissue, but this nomenclature tells only part of the story. What makes osteocalcin truly remarkable is its bioactive circulating form, which functions as a hormone with receptors throughout the body.
"Osteocalcin represents a paradigm shift in understanding bone physiology—from a static structural tissue to an active endocrine organ orchestrating whole-body metabolism." — Current Research Consensus
The Carboxylated vs. Undercarboxylated Forms
Critical to understanding osteocalcin's endocrine functions is the distinction between two molecular forms:
Carboxylated Osteocalcin (cOCN): The inactive form that remains within bone matrix
Undercarboxylated Osteocalcin (ucOCN): The bioactive form circulating in blood, acting as an endocrine factor
The undercarboxylated form is the biologically active molecule responsible for most systemic effects. This distinction is crucial because traditional immunoassays often fail to differentiate between these forms, leading to measurement discrepancies. Recent technological advances using mass spectrometry now enable precise quantification of each form, providing clinicians with more accurate biomarkers for metabolic assessment.
2025 Research Summary: Global Perspectives on Osteocalcin
1. Determe et al. (2025): Osteocalcin Analytical Innovation
Key Focus: This comprehensive review by Determe et al. (2025) addresses a critical gap in osteocalcin research: analytical measurement accuracy. The authors examine multiple immunoassay platforms (RIA, EIA, ECLIA, IRMA, ELISA) and innovative techniques like OS-ELISA and phage Immuno-PCR.
Key Finding: Mass spectrometry-based techniques enable precise differentiation and quantification of carboxylated, undercarboxylated, and fragmented osteocalcin forms, essential for accurate clinical diagnosis and monitoring.
2.Martiniakova et al. (2024) Osteocalcin in Bone and Metabolic Disease
Key Focus: This systematic review by Martiniakova et al. (2024) synthesises evidence on osteocalcin's therapeutic potential across multiple disease states, demonstrating its relevance not only to metabolic diseases but also to bone disorders and autoimmune conditions.
Key Finding: Elevated undercarboxylated osteocalcin correlates inversely with type 2 diabetes risk, suggesting osteocalcin supplementation or bone-targeted therapies may offer novel treatment pathways for metabolic disorders.
3. Ding et al. (2025): Undercarboxylated Osteocalcin as Biomarker
Key Focus: Ding and colleagues pioneer the investigation of undercarboxylated osteocalcin as a clinical biomarker and potential therapeutic agent, particularly in neurodegenerative conditions.
Key Finding: Circulating levels of undercarboxylated osteocalcin show promise as a biomarker for cognitive decline risk, and therapeutic elevation of ucOCN may represent a novel strategy for slowing neurodegenerative disease progression.
4. Consolim-Colombo & Lopes (2025): Osteocalcin and Metabolic Syndrome
Key Focus: This article specifically examines osteocalcin's role in metabolic syndrome—the cluster of cardiometabolic risk factors including hypertension, dyslipidemia, and central obesity.
Key Finding: Low serum osteocalcin levels independently predict increased metabolic syndrome risk, suggesting osteocalcin assessment can be incorporated into cardiovascular risk stratification protocols.
5. Zhang et al. (2025): Vitamin K2 and Bone Turnover
Key Focus: Zhang's systematic review and meta-analysis synthesises evidence on how vitamin K2 supplementation affects osteocalcin carboxylation and bone turnover markers in populations with osteoporosis.
Key Finding: Vitamin K2 supplementation significantly increases undercarboxylated osteocalcin levels and improves bone density markers in postmenopausal women, suggesting a pharmacological approach to optimizing osteocalcin's endocrine functions.
6. Nowicki & Jakubowska-Pietkiewicz (2024): Osteocalcin Beyond Bones
Key Focus: This review emphasizes the paradigm shift from viewing osteocalcin as merely a bone matrix protein to understanding it as a systemic endocrine regulator affecting multiple organ systems.
Key Finding: Osteocalcin's pleiotropic effects across bone, pancreas, adipose tissue, and brain underscore the importance of bone-derived factors in whole-body physiology and the potential for bone-targeted interventions to treat diverse metabolic and neurological disorders.
Osteocalcin and Diabetes Management: Clinical Applications
One of the most clinically significant discoveries in 2025 research is osteocalcin's direct relationship with diabetes risk and glycemic control. Multiple studies demonstrate that higher circulating osteocalcin levels, particularly in the undercarboxylated form, correlate with improved insulin sensitivity and lower type 2 diabetes risk.
Mechanisms of Action in Glucose Homeostasis
Osteocalcin stimulates insulin secretion through direct action on pancreatic beta cells expressing osteocalcin receptors. Simultaneously, it enhances insulin sensitivity in muscle and adipose tissue through GPRC6A receptor activation. This dual mechanism makes osteocalcin a critical regulator of glucose metabolism at multiple levels.
Clinical Implications for Diabetic Patients
Research suggests that monitoring undercarboxylated osteocalcin levels could provide clinicians with an early indicator of metabolic dysfunction before overt diabetes develops. Furthermore, optimizing osteocalcin status through bone-targeted interventions may represent a novel approach to diabetes prevention and management.
For patients already diagnosed with type 2 diabetes, enhancing osteocalcin function through appropriate vitamin K status, exercise that stimulates bone turnover, and potentially targeted medications could improve glycemic control and reduce cardiovascular complications.
Metabolic Syndrome and Cardiovascular Health
The 2025 research by Consolim-Colombo and Lopes highlights osteocalcin's emerging role in preventing metabolic syndrome, the constellation of risk factors that dramatically increase cardiovascular disease and stroke risk.
The Osteocalcin-Metabolic Syndrome Connection
Low serum osteocalcin has been identified as an independent risk factor for metabolic syndrome development. This relationship appears mediated through multiple pathways:
Improved lipid metabolism: Osteocalcin reduces fat accumulation and improves HDL cholesterol
Enhanced endothelial function: Promotes vascular health and reduces arterial stiffness
Decreased inflammation: Suppresses systemic inflammatory markers associated with cardiometabolic disease
Optimized blood pressure: Influences vascular tone and endothelial function
This research suggests a paradigm shift in cardiovascular prevention: maintaining optimal bone health and osteocalcin status should be considered a cornerstone of cardiovascular disease prevention, alongside traditional approaches like statins, ACE inhibitors, and lifestyle modification.
Neurodegenerative Diseases and Cognitive Health
Perhaps the most exciting frontier in 2025 osteocalcin research is its emerging role in cognitive health and neurodegenerative disease prevention. Ding and colleagues' groundbreaking work demonstrates that undercarboxylated osteocalcin can cross the blood-brain barrier and exert direct neuroprotective effects.
Osteocalcin's Neurological Functions
Osteocalcin promotes neuroplasticity—the brain's ability to form new neural connections—and supports memory consolidation through interactions with brain-derived neurotrophic factor (BDNF) signaling. Additionally, osteocalcin demonstrates anti-inflammatory and antioxidant properties in neural tissue, potentially protecting against neurodegenerative cascades.
Clinical Potential in Cognitive Decline
Research suggests that lower osteocalcin levels correlate with increased cognitive decline risk and may predict Alzheimer's disease progression. This opens entirely new treatment avenues: rather than directly targeting amyloid or tau pathology, optimizing systemic osteocalcin levels through bone-targeted interventions might provide neuroprotection through systemic metabolic optimization.
For populations at risk of neurodegenerative disease, ensuring adequate vitamin K status, regular weight-bearing exercise to stimulate bone turnover, and potentially targeted pharmacological approaches to elevate osteocalcin represent emerging preventive strategies grounded in solid mechanistic and epidemiological evidence.
Vitamin K2 and Bone Health Optimization: The Missing Link
Vitamin K2 (menaquinone) plays a crucial role in bone health and osteocalcin function that has historically been underappreciated in clinical practice. Zhang and colleagues' 2025 meta-analysis provides compelling evidence for vitamin K2's ability to enhance osteocalcin carboxylation, the biochemical modification essential for osteocalcin's bioactivity.
How Vitamin K2 Activates Osteocalcin
Vitamin K serves as a cofactor for gamma-carboxylase enzymes that add carboxyl groups to osteocalcin's glutamic acid residues. This carboxylation is essential for osteocalcin's ability to bind minerals and function as an endocrine factor. In vitamin K deficiency, osteocalcin remains undercarboxylated and dysfunctional, despite adequate protein synthesis.
Clinical Evidence for K2 Supplementation
Zhang's meta-analysis of postmenopausal women reveals:
Increased undercarboxylated osteocalcin: Vitamin K2 supplementation significantly elevates the bioactive circulating form
Improved bone density: Enhanced carboxylation correlates with superior bone mineral density responses
Reduced fracture risk: Long-term supplementation studies demonstrate fracture risk reduction, particularly for vertebral fractures
Enhanced metabolic markers: Improved glucose tolerance and lipid profiles suggest systemic metabolic benefits
For individuals seeking to optimize osteocalcin function, ensuring adequate vitamin K2 status should be considered. Dietary sources include fermented foods, certain cheeses, and grass-fed dairy products.
Advanced Measurement Techniques: From Immunoassay to Mass Spectrometry
A significant contribution of Determe and colleagues' 2025 review is systematic evaluation of analytical methods for osteocalcin measurement. This is clinically critical because measurement accuracy directly impacts clinical decision-making.
Traditional Immunoassay Limitations
Radioimmunoassay (RIA), enzyme immunoassay (EIA), electrochemiluminescence (ECLIA), and ELISA platforms have historically dominated osteocalcin measurement. However, these methods suffer from critical limitations:
Emerging Mass Spectrometry Approaches
Liquid chromatography-tandem mass spectrometry (LC-MS/MS) and related approaches now enable:
For clinical adoption, research-grade mass spectrometry osteocalcin measurements should gradually replace traditional immunoassays, particularly in specialized metabolic clinics and research centers.
Frequently Asked Questions About Osteocalcin
1. What is osteocalcin?
Osteocalcin is a protein produced by osteoblasts during bone formation. While traditionally considered a bone matrix protein, research over the past two decades suggests it may also function as a hormone influencing glucose metabolism, energy regulation, and possibly brain function. Its endocrine role is well established in animal models and increasingly studied in humans.
2. What is the difference between carboxylated and undercarboxylated osteocalcin?
Carboxylated osteocalcin (cOCN): Primarily binds to bone matrix.
Undercarboxylated osteocalcin (ucOCN): Circulates in blood and is believed to be the metabolically active form.
However, the exact biological role of these forms in humans remains under investigation, and assay variability complicates interpretation.
3. Does osteocalcin help with weight loss?
Animal studies show that osteocalcin can increase energy expenditure and reduce fat mass. In humans, higher circulating osteocalcin levels are associated with better metabolic profiles and lower fat mass, but direct causation or therapeutic weight-loss effects have not been conclusively demonstrated.
4. How does osteocalcin affect diabetes risk?
Observational studies show that higher osteocalcin levels are associated with improved insulin sensitivity and lower type 2 diabetes risk. However, interventional studies are limited, and osteocalcin testing is not currently recommended in diabetes guidelines.
5. Can osteocalcin improve brain health?
Emerging research suggests osteocalcin may cross the blood–brain barrier and influence cognition in animal models. Human data are preliminary, and its role in preventing neurodegenerative diseases remains investigational.
6. Should I test my osteocalcin levels?
Osteocalcin testing is mainly used in research and bone turnover assessment. It is not currently a standard screening tool for metabolic or cardiovascular disease.
7. Does vitamin K2 increase osteocalcin?
Vitamin K is required for osteocalcin carboxylation. Supplementation can alter osteocalcin forms, particularly in osteoporosis. However, whether this translates into metabolic benefits in humans remains uncertain.
8. Is osteocalcin a treatment target?
Osteocalcin is an emerging therapeutic target in metabolic research, but no approved treatments currently target it directly.
Key Takeaways: Osteocalcin's Role in Modern Medicine
Paradigm Shift: Bone is an endocrine organ, and osteocalcin is a systemic hormone with effects far beyond skeletal function
Metabolic Health: Osteocalcin directly regulates glucose metabolism, insulin sensitivity, and lipid homeostasis, making it central to diabetes prevention
Cardiovascular Protection: Low osteocalcin predicts metabolic syndrome and cardiovascular disease risk, suggesting that bone health is cardiovascular health
Brain Health: Emerging evidence demonstrates osteocalcin's neuroprotective functions, potentially preventing cognitive decline and neurodegenerative diseases
Vitamin K2 Optimization: Vitamin K2 supplementation enhances osteocalcin carboxylation and bioactivity
Measurement Accuracy: Mass spectrometry-based osteocalcin assessment provides superior clinical insights compared to traditional immunoassays
Therapeutic Potential: Bone-targeted interventions may offer novel approaches to treating diverse metabolic and neurological disorders
Lifestyle Integration: Weight-bearing exercise, adequate calcium and vitamin K2, and stable metabolism support optimal osteocalcin status
The Future of Osteocalcin-Based Medicine
As 2025 research demonstrates, we stand at the threshold of a medical revolution centered on understanding bone as a metabolic and endocrine organ. Osteocalcin represents a novel therapeutic target for conditions as diverse as type 2 diabetes, metabolic syndrome, cardiovascular disease, and cognitive decline.
The convergence of evidence from Determe, Martiniakova, Ding, Consolim-Colombo, Zhang, and Nowicki's 2025 and 2024 research suggests that future medicine will integrate bone health optimization as a cornerstone of metabolic disease prevention and treatment. Rather than treating metabolic disorders in isolation, clinicians will increasingly consider systemic bone-metabolic health as the foundation.
Ready to Optimize Your Osteocalcin Status?
✓ Ensure adequate vitamin K2 intake
✓ Engage in regular weight-bearing exercise
✓ Maintain optimal calcium and vitamin D status
✓ Request osteocalcin testing from your healthcare provider
✓ Discuss bone-targeted interventions for metabolic health
Author’s Note
Osteocalcin represents one of the most fascinating evolutions in modern endocrinology—the recognition that bone is not merely structural, but metabolically active and hormonally integrated with multiple organ systems. As a clinician and researcher in internal medicine, my goal in writing this article was to synthesize the most recent 2024–2025 evidence into a clear, clinically grounded narrative that bridges molecular biology and bedside relevance.
While experimental data—particularly from animal models—demonstrate compelling endocrine effects of osteocalcin on glucose metabolism, energy regulation, and neurobiology, translation to human physiology remains an active area of investigation. Observational associations are robust, but interventional trials and long-term outcome data are still emerging. For this reason, osteocalcin should currently be viewed as a promising biomarker and therapeutic target under investigation rather than a guideline-endorsed clinical tool.
I have aimed to present a balanced interpretation of the literature, acknowledging both the excitement surrounding bone-derived endocrine signaling and the methodological limitations that continue to shape the field—particularly assay variability and differences between murine and human physiology.
As research advances, the integration of bone health into metabolic and cardiovascular medicine may redefine preventive strategies. Until then, scientific rigor, cautious interpretation, and evidence-based practice must remain our foundation.
Disclaimer: This article is for educational and informational purposes only and should not be considered medical advice. Always consult with qualified healthcare professionals before making changes to your health regimen or treatment plan. The information presented reflects current research as of February 2026 and may be subject to change as new evidence emerges.
Related Articles
How to Build a Disease-Proof Body: Master Calories, Exercise & Longevity | DR T S DIDWA
References
Consolim-Colombo, F. M., & Lopes, H. F. (2025). Osteocalcin and metabolic syndrome. Scripta Medica, 56(3), 547–555. https://doi.org/10.5937/scriptamed56-59319
Determe, W., Hauge, S. C., Demeuse, J., Massonnet, P., Grifnée, E., Huyghebaert, L., Dubrowski, T., Schoumacher, M., Peeters, S., Le Goff, C., Evenepoel, P., Hansen, D., & Cavalier, E. (2025). Osteocalcin: A bone protein with multiple endocrine functions. Clinica Chimica Acta; International Journal of Clinical Chemistry, 567, 120067. https://doi.org/10.1016/j.cca.2024.120067
Ding, Y.-y., Yang, Y.-y., Sun, L.-h., Liu, J.-m., & Tao, B. (2025). Clinical potential of undercarboxylated osteocalcin in metabolic and neurodegenerative diseases: From biomarker to therapeutic target. LabMed Discovery, 2(2), 100074. https://doi.org/10.1016/j.lmd.2025.100074
Martiniakova, M., Biro, R., Kovacova, V., Babikova, M., Zemanova, N., Mondockova, V., & Omelka, R. (2024). Current knowledge of bone-derived factor osteocalcin: Its role in the management and treatment of diabetes mellitus, osteoporosis, osteopetrosis and inflammatory joint diseases. Journal of Molecular Medicine (Berlin, Germany), 102(4), 435–452. https://doi.org/10.1007/s00109-024-02418-8
Nowicki, J. K., & Jakubowska-Pietkiewicz, E. (2024). Osteocalcin: Beyond bones. Endocrinology and Metabolism, 39(3), 399–406. https://doi.org/10.3803/EnM.2023.1895
Zhang, Z., Li, Y., Li, J., Yuan, Y., Liu, K., & Shi, X. (2025). The effect of vitamin K2 supplementation on bone turnover biochemical markers in postmenopausal osteoporosis patients: A systematic review and meta-analysis. Frontiers in Endocrinology, 16, Article 1703116. https://doi.org/10.3389/fendo.2025.1703116