Is Your Heart at Risk? How the TG/HDL Ratio Can Warn You Early
Are traditional cholesterol tests enough? Explore why 2025 research favors the CHG index and TG/HDL ratio for predicting heart disease and insulin resistance.
HEARTMETABOLISM
Dr. T.S. Didwal, M.D.(Internal Medicine)
1/12/202612 min read
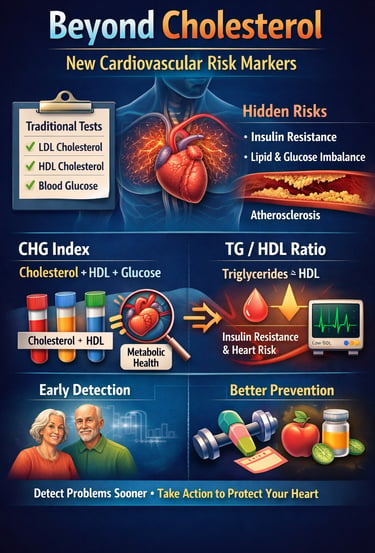
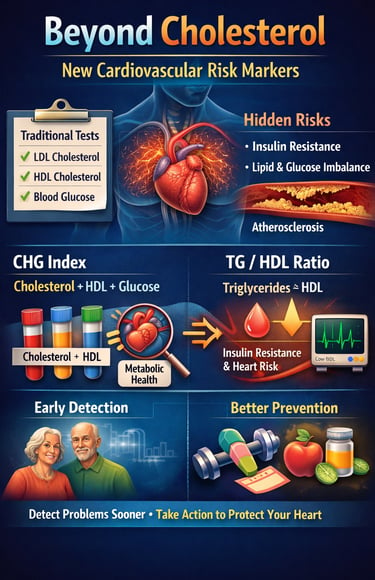
Have you ever looked at your blood test results and wondered if those numbers truly reflect your heart health? For years, we’ve been taught to focus on total cholesterol, LDL, HDL, and fasting glucose. But emerging research reveals a surprising truth: these familiar markers may miss early warning signs of cardiovascular disease, especially in people with subtle metabolic disturbances that traditional tests overlook (Mo et al., 2025).
Modern science now shows that heart disease doesn’t begin with a single abnormal number—it starts with a hidden metabolic imbalance involving insulin resistance, disrupted lipid metabolism, and impaired glucose regulation. These interconnected processes quietly damage arteries long before symptoms appear. That’s why newer composite markers like the triglyceride-to-HDL ratio and the CHG index are gaining attention: they capture the full metabolic picture rather than isolated snapshots (Kosmas et al., 2023).
Think of these indices as early warning systems—sensitive enough to detect risk years before a heart attack or stroke occurs. Studies even show that these combined markers outperform traditional cholesterol alone in predicting cardiovascular events, especially in high-risk individuals and those with underlying insulin resistance (He et al., 2025).
In short, heart disease risk assessment is evolving—and understanding these newer markers could literally save your life.
Clinical pearls
1. TG/HDL Ratio
Don't look at triglycerides or HDL in isolation. Think of triglycerides as the "trash" (excess fat) and HDL as the "clean-up crew." Dividing your triglycerides by your HDL gives you a ratio that tells you if your clean-up crew is overwhelmed. In 2026, we know that a ratio above 3.5 is a loud alarm for insulin resistance and heart risk.
Clinical Insight: A "normal" total cholesterol can hide a dangerous TG/HDL ratio. If your ratio is high, your arteries are likely accumulating "trash" faster than they can be cleaned.
2. CHG Index
The new CHG Index (Cholesterol, HDL, Glucose) is a game-changer because it recognizes that high sugar and high fat don't just add up—they multiply each other's damage. When glucose is high, it "syrup-coats" your cholesterol particles, making them stickier and more likely to lodge in your artery walls.
Clinical Insight: If you are managing both borderline blood sugar and high cholesterol, you cannot treat them as separate issues. Improving your glucose will directly make your cholesterol profile less dangerous.
3. TyG Index
The Triglyceride-Glucose (TyG) Index is your most sensitive radar for insulin resistance. Even if your "A1c" (3-month average sugar) looks okay, a high TyG index indicates that your body is struggling behind the scenes to keep those numbers stable.
Clinical Insight: Think of the TyG index as an early warning system. It often catches metabolic "engine trouble" years before a diagnosis of Type 2 Diabetes occurs.
4. Secondary Prevention
If you’ve already had a heart procedure (like a stent or PCI), your TG/HDL ratio is your best predictor of future success. The 2024–2025 data (Zhou et al.) shows that even if the "plumbing" is fixed, a high metabolic ratio means the "soil" is still fertile for growing new blockages.
Clinical Insight: After a heart procedure, your goal isn't just "clear pipes"; it’s a metabolic reset. Lowering your ratio through diet and exercise is what keeps that stent open long-term.
5. The Modified TyG
For those dealing with heart failure, the HDL-modified TyG index is a critical survival marker. It measures how well your body uses fuel (glucose) and filters out waste (HDL). When this index is off, it signals that the heart muscle isn't getting the "clean energy" it needs to pump effectively.
Clinical Insight: In high-risk cardiac patients, metabolic health is synonymous with heart strength. Improving these numbers can literally take the physical load off a weakened heart muscle.
Beyond Cholesterol: Understanding New Cardiovascular Risk Markers That Could Save Your Life
The Evolution of Cardiovascular Risk Assessment
For decades, doctors have relied on individual measurements—total cholesterol, LDL cholesterol (the "bad" kind), HDL cholesterol (the "good" kind), and triglycerides—to gauge cardiovascular risk. But here's the problem: these isolated numbers don't tell the complete story.
Think of it like trying to predict weather using only temperature. You'd miss crucial information about humidity, wind speed, and atmospheric pressure. Similarly, single biomarkers miss the complex metabolic interactions that truly drive heart disease, stroke, and other cardiovascular events.
The Cholesterol, High-Density Lipoprotein, and Glucose Index: A New Contender
What the Research Tells Us
A comprehensive cohort study by Mo et al. (2025) published in Cardiovascular Diabetology investigated a novel marker called the Cholesterol, High-Density Lipoprotein, and Glucose (CHG) index. This index combines three fundamental metabolic components to create a more nuanced risk assessment tool.
Key Study Details:
The research compared the CHG index against the well-established triglyceride-glucose (TyG) index
Researchers analyzed data from a large cohort to determine which marker better predicted cardiovascular disease outcomes
The study examined both coronary artery disease, myocardial infarction (heart attack), and cerebrovascular events (stroke)
Critical Findings: The CHG index demonstrated superior predictive value compared to traditional single biomarkers. By integrating total cholesterol, HDL-C levels, and blood glucose, this composite marker captures the interplay between lipid metabolism and glucose homeostasis—two processes intimately connected to atherosclerosis development.
Clinical Significance: This research suggests that physicians could identify at-risk patients earlier by using the CHG index, potentially allowing for more aggressive primary prevention strategies before cardiovascular events occur (Mo et al., 2025).
The Triglyceride-to-HDL Ratio: A Powerful Metabolic Signal
Understanding This Simple Yet Effective Marker
The triglyceride/HDL cholesterol ratio (TG/HDL-C) has emerged as one of the most accessible yet powerful indicators of metabolic syndrome and cardiovascular risk. Kosmas et al. (2023) provided a comprehensive review of this marker's clinical utility.
Study Highlights:
Published in Diagnostics, this review synthesized evidence supporting the TG/HDL-C ratio as a risk marker
The ratio reflects underlying insulin resistance, a key driver of metabolic disease
Optimal ratios vary by population, but elevated ratios consistently predict poor outcomes
Why This Ratio Matters: The TG/HDL-C ratio captures the balance between triglyceride-rich lipoproteins (which promote atherosclerosis) and protective HDL particles. A high ratio indicates dyslipidemia—an abnormal lipid profile strongly associated with type 2 diabetes, obesity, and cardiovascular disease.
Practical Application: Unlike complex calculations, you can compute this ratio from standard lipid panel results. Simply divide your triglyceride level by your HDL cholesterol level. Generally, ratios above 3.5 suggest increased metabolic and cardiovascular risk, though cutoffs may differ based on individual characteristics (Kosmas et al., 2023).
Patient-Friendly Perspective: Think of HDL as your body's cleanup crew, removing excess cholesterol from arteries. Triglycerides represent excess fuel storage. When triglycerides overwhelm your HDL cleanup crew, arterial damage accelerates—precisely what the TG/HDL-C ratio captures.
HDL-Modified TyG Index in Heart Failure Patients
A Specialized Marker for High-Risk Populations
Patients with acute decompensated heart failure (ADHF) face particularly high mortality risk. He et al. (2025) investigated whether an HDL-modified version of the triglyceride-glucose index could predict outcomes in this vulnerable population.
Research Overview:
Published in Frontiers in Endocrinology, this study examined both all-cause mortality and cardiovascular mortality
Researchers analyzed the independent and combined associations of the HDL-cholesterol-modified TyG index
The study followed ADHF patients to determine which metabolic markers best predicted survival
Key Discoveries: The HDL-modified TyG index showed robust associations with both all-cause and cardiovascular mortality. Importantly, this marker provided prognostic information beyond traditional risk factors, helping clinicians identify heart failure patients who need intensified monitoring and treatment.
Mechanistic Insights: The TyG index fundamentally assesses insulin resistance by combining fasting glucose and triglycerides. Adding HDL cholesterol enhances this assessment because HDL dysfunction frequently accompanies insulin resistance and predicts adverse outcomes in heart failure. Low HDL levels indicate impaired reverse cholesterol transport—the process by which excess cholesterol is removed from tissues and returned to the liver (He et al., 2025).
Clinical Implications: For heart failure specialists, this modified index offers a readily calculable tool using routine laboratory tests. Patients with elevated HDL-modified TyG index values might benefit from more aggressive lipid-lowering therapy, glycemic control, and close follow-up to prevent cardiovascular death.
The CHG Index: Validating a Novel Approach
Smith et al. (2025) introduced and validated the Cholesterol, High-Density Lipoprotein, Glucose (CHG) index as a novel composite marker. Their preprint study, available on medRxiv, represents cutting-edge research that hasn't yet undergone full peer review but offers exciting preliminary findings.
Study Design:
The formula for calculating the CHG index is: CHG index = Ln [TC (mg/dL) × FBG (mg/dL) / 2 × HDL (mg/dL)]
Developed a new calculation method combining cholesterol, HDL, and glucose
Validated the index against established cardiovascular outcomes
Compared predictive performance with existing markers
Preliminary Results: The CHG index demonstrated strong associations with major adverse cardiovascular events (MACE), including heart attack, stroke, and cardiovascular death. The authors propose specific cutoff values that could stratify patients into low, intermediate, and high-risk categories.
Innovation Factor: Unlike ratios that only capture lipid balance, the CHG index integrates glycemic status with lipid parameters. This holistic approach recognizes that cardiovascular disease stems from interconnected metabolic disturbances rather than isolated abnormalities.
Important Note: As a preprint, this research awaits peer review validation. However, the conceptual framework aligns with our evolving understanding of metabolic-cardiovascular disease as a unified process (Smith et al., 2025).
TG/HDL Ratio in Acute Coronary Syndrome
Predicting Outcomes After Intervention
When someone experiences acute coronary syndrome (ACS)—encompassing heart attacks and unstable angina—they typically undergo percutaneous coronary intervention (PCI), a procedure to open blocked arteries. But who remains at highest risk afterward? Zhou et al. (2024) tackled this question.
Research Focus:
Published in Scientific Reports, this study examined ACS patients who underwent PCI
Investigated whether the TG/HDL cholesterol ratio predicted major adverse cardiovascular events post-procedure
Analyzed both short-term and long-term outcomes
Major Findings: Elevated TG/HDL ratios independently predicted MACE occurrence after PCI, even when accounting for traditional risk factors. Patients with high ratios experienced more recurrent heart attacks, need for repeat procedures, and cardiovascular deaths.
Mechanistic Understanding: Even after opening blocked arteries, patients with unfavorable metabolic profiles continue accumulating arterial damage. The TG/HDL ratio reflects this ongoing atherogenic (plaque-forming) process, indicating patients who need aggressive secondary prevention measures.
Actionable Insights: Cardiologists can use post-PCI TG/HDL ratios to guide treatment intensity. Patients with elevated ratios might benefit from high-intensity statin therapy, addition of medications like PCSK9 inhibitors, and rigorous lifestyle modifications (Zhou et al., 2024).
Why These Combined Indices Matter More Than Single Biomarkers
Traditional cardiovascular risk assessment focused on individual measurements, but modern research reveals the limitations of this approach:
Metabolic Interconnections: Glucose metabolism and lipid metabolism aren't separate systems—they're deeply intertwined. Insulin resistance simultaneously elevates triglycerides, lowers HDL, and impairs glucose control. Composite indices capture these relationships.
Risk Amplification: Multiple mild abnormalities may pose greater risk than a single severe abnormality. Someone with moderately elevated cholesterol, slightly low HDL, and borderline glucose might face higher cardiovascular risk than someone with isolated severe hypercholesterolemia.
Personalized Medicine: Combined indices enable more nuanced risk stratification, moving beyond one-size-fits-all approaches toward precision medicine that accounts for individual metabolic profiles.
Understanding the Science Behind These Markers
Insulin Resistance: The Common Thread
Most composite cardiovascular markers reflect underlying insulin resistance—the condition where cells don't respond properly to insulin. This metabolic dysfunction triggers a cascade of problems:
Elevated triglycerides: Excess insulin promotes triglyceride production
Reduced HDL: Insulin resistance lowers beneficial HDL particles
Impaired glucose control: Cells can't effectively absorb glucose
Inflammatory state: Insulin resistance promotes chronic inflammation
Endothelial dysfunction: Blood vessel lining becomes damaged
Atherosclerosis Development
These metabolic changes accelerate atherosclerotic plaque formation—the underlying cause of most heart attacks and strokes:
Lipid accumulation: Excess triglyceride-rich particles infiltrate arterial walls
HDL dysfunction: Reduced HDL means less efficient cholesterol removal
Glycation damage: Elevated glucose causes proteins to become "sticky," damaging vessels
Inflammatory response: The body's immune system attacks arterial damage, paradoxically worsening it
Plaque rupture: Unstable plaques eventually rupture, triggering blood clots that cause heart attacks and strokes
Practical Implications for Your Health
Getting Tested
Most composite cardiovascular indices require only standard blood tests:
Fasting Lipid Panel:
Total cholesterol
LDL cholesterol
HDL cholesterol
Triglycerides
Glucose Testing:
Fasting blood glucose
Hemoglobin A1c (reflects 3-month glucose average)
Calculating Your Risk Markers
While your doctor should interpret results, understanding the calculations empowers informed conversations:
TG/HDL-C Ratio: Triglycerides (mg/dL) ÷ HDL cholesterol (mg/dL)
Example: Triglycerides = 150 mg/dL, HDL = 40 mg/dL Ratio = 150 ÷ 40 = 3.75 (elevated risk)
TyG Index: ln[triglycerides (mg/dL) × fasting glucose (mg/dL) / 2]
The CHG index calculation varies by specific formula used in research, requiring medical interpretation.
Quick Summary:
TG/HDL > 3.5 = Insulin resistance + high CV risk
CHG index predicts early atherosclerosis
TyG index = early signal for prediabetes
HDL-modified TyG predicts mortality in HF
Composite indices outperform single cholesterol values
Optimizing Your Metabolic Profile
Regardless of which marker your doctor uses, improving underlying metabolic health benefits all indices:
Dietary Strategies:
Reduce refined carbohydrates: White bread, sugary beverages, and sweets spike glucose and triglycerides
Increase fiber intake: Whole grains, vegetables, and legumes improve insulin sensitivity
Choose healthy fats: Olive oil, nuts, avocados, and fatty fish support favorable lipid profiles
Limit saturated fat: Red meat and full-fat dairy can worsen dyslipidemia
Consider Mediterranean or DASH diets: Both show robust cardiovascular benefits
Physical Activity:
Aerobic exercise: 150 minutes weekly of moderate-intensity activity lowers triglycerides and raises HDL
Resistance training: Building muscle improves insulin sensitivity
Consistency matters: Regular activity provides better metabolic benefits than sporadic intense sessions
Weight Management: Even modest weight loss (5-10% of body weight) dramatically improves insulin sensitivity, triglycerides, HDL, and glucose
Medication Options: When lifestyle changes aren't sufficient:
Statins: Lower cholesterol and reduce cardiovascular events
Fibrates: Specifically target triglyceride reduction
SGLT2 inhibitors or GLP-1 agonists: Improve glucose control with cardiovascular benefits
Omega-3 fatty acids: High-dose formulations reduce triglycerides
Key Takeaways
✅ Composite metabolic indices like the CHG index and TG/HDL ratio predict cardiovascular risk more accurately than single biomarkers
✅ The triglyceride-to-HDL cholesterol ratio offers a simple yet powerful assessment of metabolic health and heart disease risk
✅ HDL-modified versions of established indices provide enhanced prognostic information, especially in high-risk populations like heart failure patients
✅ These markers capture the interconnected nature of glucose metabolism and lipid metabolism in driving atherosclerosis
✅ Elevated ratios or indices signal underlying insulin resistance, the common metabolic disturbance linking obesity, diabetes, and cardiovascular disease
✅ Lifestyle modifications—particularly diet, exercise, and weight management—improve all composite cardiovascular markers
✅ These indices enable more personalized risk stratification, guiding treatment intensity based on individual metabolic profiles
✅ Patients with acute coronary syndrome or heart failure benefit from prognostic assessment using these combined biomarkers
Frequently Asked Questions
Q: Are these new indices better than traditional cholesterol testing?
A: These composite indices complement rather than replace traditional testing. They provide additional prognostic information by capturing metabolic interactions missed by single biomarkers. Your doctor will interpret them alongside conventional risk factors.
Q: What's considered a healthy TG/HDL-C ratio?
A: Optimal ratios are typically below 2.0, though cutoffs vary by population. Ratios above 3.5 generally indicate increased cardiovascular and metabolic risk. Discuss your specific target with your healthcare provider.
Q: Can I improve these markers without medication?
A: Absolutely! Diet, exercise, and weight management profoundly impact triglycerides, HDL cholesterol, and glucose control—the components of these indices. Many people achieve target values through comprehensive lifestyle changes alone.
Q: How often should these markers be checked?
A: For average-risk individuals, testing every 3-5 years is typically sufficient. Those with metabolic syndrome, diabetes, cardiovascular disease, or other risk factors need more frequent monitoring, often annually or even quarterly when optimizing treatment.
Q: Do these indices apply to everyone?
A: Research has validated these markers across diverse populations, but optimal cutoffs may vary by ethnicity, age, and other factors. Interpretation should always be individualized within the context of your complete medical picture.
Q: If my regular cholesterol is normal but these composite markers are elevated, what does that mean?
A: You may have metabolic disturbances that traditional testing misses. For instance, you could have normal total cholesterol but low HDL and high triglycerides—a pattern strongly associated with insulin resistance and cardiovascular risk. Composite markers detect these nuanced profiles.
Q: Are these tests expensive or hard to get?
A: No additional testing is needed! These indices are calculated from standard lipid panels and glucose tests typically covered by insurance. Your doctor can calculate them from routine blood work results.
Author’s Note
As a clinician and researcher, I have witnessed firsthand how many patients with “normal” cholesterol profiles still develop heart attacks, strokes, or silent metabolic deterioration. This disconnect between traditional testing and real-world outcomes is what motivated me to explore emerging cardiovascular risk markers.
Today’s science clearly shows that cardiovascular disease is not driven by a single number—it is the result of complex interactions between insulin resistance, lipid imbalance, inflammation, and glucose dysregulation. Composite indices like the CHG index, TG/HDL ratio, and HDL-modified TyG index represent a significant advancement toward more accurate risk identification. They allow clinicians to detect early metabolic disturbances that may remain hidden when we rely solely on LDL or total cholesterol.
My intention in writing this article is to translate rapidly evolving research into actionable, patient-friendly insights. These tools are not meant to replace traditional markers but to enhance them—offering deeper clarity and earlier warning signs so individuals can take preventive steps long before disease progresses.
By empowering patients with knowledge, we empower them with control over their cardiovascular future
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Individual circumstances vary, and treatment decisions should always be made in consultation with qualified healthcare professionals.
Related Articles
Reversing Heart Age: What New Research Reveals About Arterial Stiffness | DR T S DIDWAL
Forget BMI: Metabolic Health Is the Real Key to Heart Disease Risk | DR T S DIDWAL
High Blood Pressure? Why the TyG Index Is a Powerful Hidden Marker of Metabolic Risk | DR T S DIDWAL
hsCRP Explained: What Inflammation Means for Your Heart | DR T S DIDWAL
What’s New in the 2025 Blood Pressure Guidelines? A Complete Scientific Breakdown | DR T S DIDWAL
Low-Fat vs. Low-Carb: Which Diet is Best for Weight Loss? | DR T S DIDWAL
5 Steps to Reverse Metabolic Syndrome: Diet, Habit, & Lifestyle Plan | DR T S DIDWAL
The Role of Cholesterol in Health and Disease: Beyond the "Bad" Label | DR T S DIDWAL
Lowering Cholesterol with Food: 4 Phases of Dietary Dyslipidemia Treatment | DR T S DIDWAL
The Best Dietary Fat Balance for Insulin Sensitivity, Inflammation, and Longevity | DR T S DIDWAL
References
He, S., Xie, L., Xie, G., Jian, G., Jiang, K., Lu, Z., Zhang, S., Wang, Q., Lu, H., Xiong, Z., Wu, Z., Sheng, G., Lai, H., Wang, W., & Zou, Y. (2025). Independent and combined associations of high-density lipoprotein cholesterol-modified triglyceride-glucose index with all-cause and cardiovascular mortality in patients with acute decompensated heart failure. Frontiers in Endocrinology, 16, Article 1629066. https://doi.org/10.3389/fendo.2025.1629066
Kosmas, C. E., Rodriguez Polanco, S., Bousvarou, M. D., Papakonstantinou, E. J., Peña Genao, E., Guzman, E., & Kostara, C. E. (2023). The triglyceride/high-density lipoprotein cholesterol (TG/HDL-C) ratio as a risk marker for metabolic syndrome and cardiovascular disease. Diagnostics, 13(5), 929. https://doi.org/10.3390/diagnostics13050929
Mo, D., Zhang, P., Zhang, M., Xie, J., Wang, X., Li, Y., Chen, H., & Liu, X. (2025). Cholesterol, high-density lipoprotein, and glucose index versus triglyceride–glucose index in predicting cardiovascular disease risk: A cohort study. Cardiovascular Diabetology, 24, 116. https://doi.org/10.1186/s12933-025-02675-y
Smith, J. A., Lee, Q., Patel, R. K., & Gupta, M. (2025). A novel composite index for cardiovascular risk: The cholesterol, high-density lipoprotein, glucose (CHG) index (Version 1) [Preprint]. medRxiv. https://doi.org/10.1101/2025.04.02.25325143v1
Zhou, S., Qiu, M., Wang, K., Liu, Y., Zhang, L., Chen, R., Wu, J., & Yang, H. (2024). Triglyceride to high density lipoprotein cholesterol ratio and major adverse cardiovascular events in ACS patients undergoing PCI. Scientific Reports, 14, 31752. https://doi.org/10.1038/s41598-024-82064-9