High Blood Pressure? Why the TyG Index Is a Powerful Hidden Marker of Metabolic Risk
Is insulin resistance driving your high blood pressure? Discover why the TyG index is a game-changer for hypertension prevention. Learn how to use your routine blood work to uncover hidden heart health risks today.
HEARTMETABOLISM
Dr. T.S. Didwal, M.D.(Internal Medicine)
1/26/202612 min read
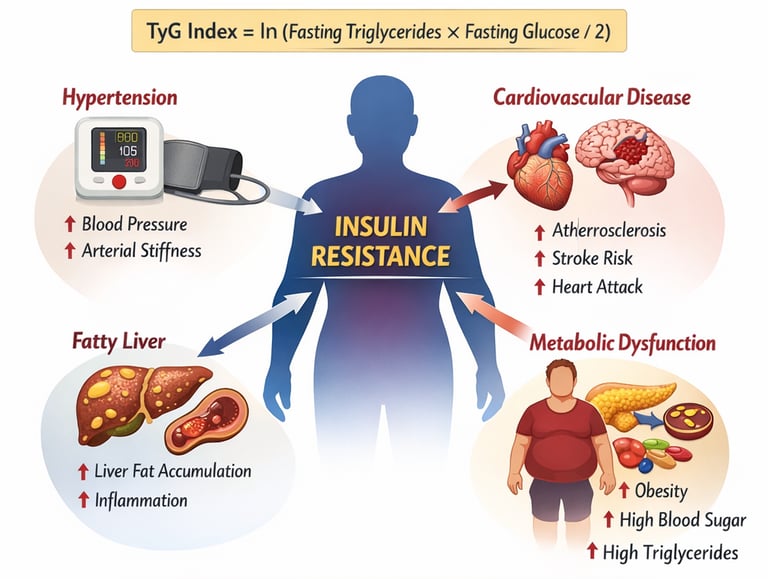
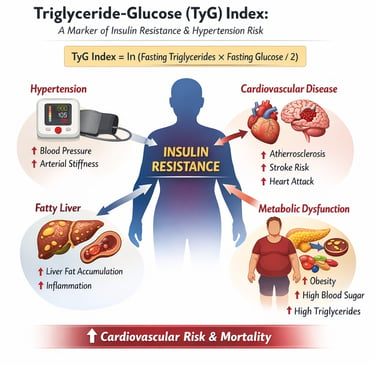
High blood pressure rarely appears out of nowhere. Long before a sphygmomanometer records elevated numbers, subtle metabolic disturbances are already reshaping vascular function, renal sodium handling, and autonomic tone. One of the most compelling markers capturing this hidden metabolic risk is the triglyceride–glucose (TyG) index—a simple calculation derived from routine fasting triglyceride and glucose values that serves as a robust surrogate for insulin resistance.
Once considered primarily a diabetes-related phenomenon, insulin resistance is now recognized as a central driver of hypertension development, even in individuals without overt hyperglycemia. Over the past few years, a growing body of research has consistently linked higher TyG index values to both pre-hypertension and established hypertension across diverse populations, including postmenopausal women, Asian cohorts, and individuals with metabolic syndrome (Zhang et al., 2025; Wang et al., 2026). Importantly, meta-analytic data confirm that this association is not isolated or incidental, but reproducible across studies and regions (Lukito et al., 2024).
What makes the TyG index particularly powerful is its clinical accessibility. Unlike complex insulin clamp studies or specialized biomarkers, TyG requires no additional testing, no extra cost, and no advanced technology—yet it reliably identifies individuals at heightened cardiometabolic risk. Prospective data from large biobank cohorts further demonstrate that elevated TyG-related indices predict not only hypertension, but also future cardiovascular events and mortality, underscoring their prognostic significance (He et al., 2026).
As hypertension guidelines increasingly emphasize early risk identification and prevention, understanding the TyG index may help clinicians and patients detect—and intervene on—cardiometabolic dysfunction years before irreversible vascular damage occurs (Hao et al., 2026).
Clinical pearls
1. The "Hidden Driver" Pearl
The Science: Hypertension is often a downstream symptom of hyperinsulinemia (excess insulin). When your body becomes resistant to insulin, your kidneys hold onto more sodium, and your sympathetic nervous system stays in "overdrive."
Think of your blood pressure as the smoke and insulin resistance as the fire. By monitoring your TyG index, you are looking at the "fire" itself. Addressing the metabolic root cause can often make blood pressure much easier to manage.
2. The "Menopause Transition" Pearl
The Science: The decline of estrogen during menopause shifts fat distribution and alters lipid metabolism, making the TyG index a more sensitive predictor of heart risk than traditional BMI in postmenopausal women.
If you are postmenopausal, your "old" health markers might stay the same even as your internal risks change. The TyG index is a specialized "early warning system" for women in this life stage, catching risks that a standard blood pressure cuff might miss.
3. The "Pre-Hypertension" Window
The Science: Research shows that TyG index elevations often precede the clinical diagnosis of high blood pressure. It acts as a marker for endothelial dysfunction—the point where blood vessels lose their flexibility but haven't yet "hardened."
An elevated TyG index is an invitation, not a sentence. If your index is high but your blood pressure is still "normal-high," you have a golden window of opportunity to use lifestyle changes to prevent a diagnosis of hypertension entirely.
4. The "Standard Lab" Advantage
The Science: Unlike the HOMA-IR test (which requires a specialized insulin assay that can be expensive or inconsistent), the TyG index uses fasting glucose and triglycerides—two of the most standardized and stable tests in modern medicine.
You likely already have the "ingredients" for this test in your previous blood work. You don't need a fancy, expensive new lab; you just need to apply the TyG formula to the results sitting in your patient portal right now.
5. The "Metabolic Synergy" Pearl
The Science: The TyG index is a "synergy" marker. High glucose alone or high triglycerides alone are risky, but when both are elevated, they have a multiplicative effect on arterial stiffness and cardiovascular mortality.
Don't look at your labs in isolation. Even if your glucose is "only a little high" and your triglycerides are "just over the limit," the TyG index shows how those two numbers work together to stress your heart.
Understanding the Triglyceride-Glucose Index and Its Connection to Hypertension: What Recent Research Reveals
High blood pressure affects nearly half of American adults, yet many don't realize that hidden metabolic problems could be driving their condition. Among the most overlooked culprits? A marker called the triglyceride-glucose index, or TyG index for short.
Recent research is shining a spotlight on this relatively simple measurement—one that combines two routinely checked blood markers to predict hypertension risk with surprising accuracy. Whether you're dealing with elevated blood pressure, concerned about metabolic syndrome, or simply want to understand your cardiovascular health better, understanding the triglyceride-glucose index could be a game-changer for your medical conversations and personal health decisions.
What Is the Triglyceride-Glucose Index?
The TyG index is a simple mathematical calculation combining two blood markers you likely see on your lab results:
Fasting triglycerides (measured in mg/dL)
Fasting blood glucose (also in mg/dL)
The formula is straightforward: TyG index = ln(triglycerides × glucose / 2). The result gives clinicians and researchers a single number that reflects your body's insulin resistance—how well your cells respond to the hormone insulin.
Why is this important? Insulin resistance is a silent driver of hypertension, metabolic dysfunction, and cardiovascular disease. The beauty of the TyG index is that it's inexpensive, readily available from standard blood work, and doesn't require special testing. In other words, your doctor may already have the information needed to calculate it without ordering additional labs.
Study 1: Zhang et al. (2025) – Triglyceride-Glucose Index in Postmenopausal Women
Zhang, Jiang, Ma, and Liu's 2025 cross-sectional study published in Frontiers in Nutrition examined a population often overlooked in hypertension research: postmenopausal women. This demographic matters because the loss of estrogen during menopause significantly alters metabolism and cardiovascular risk.
The researchers investigated the association between triglyceride-glucose index and its obesity indicators with hypertension in this specific group. Their findings demonstrated that the TyG index and related obesity indicators were independently associated with increased hypertension risk in postmenopausal women.
Postmenopausal women represent a particularly vulnerable population for developing hypertension and metabolic dysfunction. The triglyceride-glucose index emerged as a practical tool for identifying women at elevated risk—even before they develop clinical metabolic syndrome.
Key Takeaway: Postmenopausal women with elevated TyG index values should work with their healthcare providers on insulin resistance management and metabolic health optimization through lifestyle and, when appropriate, medical interventions.
Study 2: Wang et al. (2026) – Triglyceride-Glucose Series Indices in China
Wang, Li, Li, and colleagues' 2026 study published in Scientific Reports expanded the scope of triglyceride-glucose index research by examining triglyceride-glucose series indices (meaning multiple TyG-related calculations) in a Chinese population from Anhui province.
This study went further than examining just hypertension alone—the researchers investigated the association of triglyceride-glucose series indices with both hypertension and pre-hypertension. Their data revealed strong associations between these metabolic markers and both diagnosed high blood pressure and its precursor condition.
Pre-hypertension (often called elevated blood pressure) represents a critical window for intervention. Many people with pre-hypertension can prevent progression to clinical hypertension through lifestyle modifications. By identifying TyG index abnormalities, clinicians can catch at-risk individuals earlier.
Additionally, examining multiple triglyceride-glucose series indices rather than a single calculation provides a more nuanced picture of metabolic dysfunction and cardiovascular risk.
Key Takeaway: Both hypertension and pre-hypertension show strong associations with triglyceride-glucose series indices, suggesting that TyG-based screening could enable earlier intervention and prevention strategies, particularly in Asian populations.
Study 3: Lukito et al. (2024) – Systematic Review and Meta-Analysis
When individual studies point in the same direction, meta-analysis and systematic reviews synthesize that evidence to reveal the big picture. Lukito, Kamarullah, Huang, and Pranata's 2024 systematic review and meta-analysis published in Narra Journal did exactly that for the triglyceride-glucose index and hypertension connection.
By pooling data from multiple studies, their analysis confirmed a significant association between triglyceride-glucose index and hypertension across diverse populations. The meta-analysis approach provides stronger evidence than any single study alone.
Meta-analyses carry substantial weight in medical research because they combine evidence across numerous studies, reducing the influence of any single study's limitations. The fact that multiple independent research groups found similar associations between the TyG index and hypertension strengthens confidence in the relationship.
This level of evidence supports incorporating TyG index assessment into routine hypertension risk evaluation.
Key Takeaway: Systematic review evidence confirms that the triglyceride-glucose index is consistently and significantly associated with hypertension across different populations, supporting its use as a practical screening and risk stratification tool.
Study 4: He et al. (2026) – Long-Term Cardiovascular Outcomes in Metabolic Syndrome
He, Huang, Ni, and colleagues' 2026 study, published in Cardiovascular Diabetology, took the research further by examining prospective associations of triglyceride-glucose related indices with cardiovascular disease and mortality in individuals with metabolic syndrome, using data from the prestigious UK Biobank.
Unlike cross-sectional studies (which capture a single moment in time), this prospective approach followed individuals over time to see who actually developed cardiovascular disease and mortality outcomes. Their findings demonstrated that triglyceride-glucose related indices predicted not just hypertension, but serious cardiovascular events and death.
This study matters because it shows consequences beyond blood pressure numbers alone. People with elevated TyG index values face increased risk of heart attacks, strokes, and cardiovascular death. For patients with metabolic syndrome—a cluster of conditions including hypertension, elevated glucose, abnormal lipids, and obesity—TyG index assessment becomes even more critical.
The UK Biobank population represents diverse demographics, making findings broadly applicable.
Key Takeaway: In individuals with metabolic syndrome, elevated triglyceride-glucose related indices predict serious cardiovascular disease outcomes and increased mortality, emphasizing that TyG index management has life-or-death implications beyond blood pressure control alone.
Study 5: Hao et al. (2026) – Diagnostic Criteria Considerations
Hao, Geng, and Ma's 2026 study published in the International Journal of General Medicine addressed a practical but often overlooked question: Does the relationship between TyG index and hypertension change depending on which diagnostic criteria for hypertension are used?
The study examined the association between triglyceride glucose index and hypertension according to different diagnostic criteria, recognizing that hypertension definitions vary internationally (American, European, and other guidelines may use slightly different blood pressure thresholds).
Their findings revealed that TyG index associations remained robust across different diagnostic criteria, though the strength of association occasionally varied by definition used.
Healthcare systems worldwide use different hypertension diagnostic criteria. A study showing that TyG index relationships hold across various definitions increases confidence in the marker's universal applicability. This matters for patients traveling internationally, for multinational studies, and for organizations developing global health policies.
Key Takeaway: The association between the triglyceride-glucose index and hypertension remains consistent across different diagnostic hypertension criteria, supporting the use of the TyG index in diverse clinical settings and healthcare systems worldwide.
What All Five Studies Reveal Together: Synthesis and Integration
Consistency Across Diverse Populations From postmenopausal women to Chinese populations to UK Biobank participants, triglyceride-glucose index associations with hypertension remain remarkably consistent. This suggests the relationship isn't limited to specific demographics but reflects fundamental metabolic biology.
Multiple Indicators Predict Risk Studies examining triglyceride-glucose series indices and obesity indicators alongside the basic TyG index suggest that a comprehensive assessment of metabolic dysfunction—not just one marker—provides the clearest picture of hypertension risk.
Early Detection and Prevention Opportunities The focus on pre-hypertension and hypertension prevention in these studies underscores that TyG index assessment enables intervention before irreversible cardiovascular damage occurs.
Serious Consequences Beyond Blood Pressure By linking elevated TyG index to actual cardiovascular disease and mortality outcomes, these studies elevate the importance of managing this marker from merely interesting to clinically urgent.
Practical, Accessible Assessment Tool All five studies highlight that the triglyceride-glucose index requires only standard blood work—no expensive specialized testing. This accessibility means virtually any healthcare system can implement TyG-based screening.
Understanding Insulin Resistance: The Mechanism Behind the Connection
To truly grasp why triglyceride-glucose index predicts hypertension, we need to understand insulin resistance.
When cells become resistant to insulin's effects, the pancreas responds by producing more insulin to maintain blood glucose levels. This situation, called hyperinsulinemia, triggers multiple problems:
Increased sodium retention by the kidneys, raising blood volume and pressure
Endothelial dysfunction, impairing the blood vessel's ability to relax
Activation of the sympathetic nervous system, increasing heart rate and vascular resistance
Vascular remodeling that makes arteries stiffer and narrower
Inflammatory activation throughout the cardiovascular system
The triglyceride-glucose index serves as a reliable proxy for insulin resistance because both elevated triglycerides and fasting glucose reflect the pancreas's struggle to maintain glucose control. By calculating the TyG index, clinicians are essentially measuring this hidden metabolic struggle.
Practical Implications: What This Means for Your Health
If your healthcare provider mentions an elevated triglyceride-glucose index, don't panic—but do take it seriously. This is an opportunity to:
Increase physical activity (even 30 minutes of walking most days substantially improves insulin sensitivity)
Modify dietary patterns (reduce refined carbohydrates, increase fiber and whole grains)
Achieve a healthy weight if overweight (even a 5-10% weight loss improves insulin resistance)
Manage stress (chronic stress worsens insulin resistance)
Improve sleep quality (poor sleep drives metabolic dysfunction)
Monitor blood pressure regularly at home
Work with your healthcare team on personalized management strategies
Frequently Asked Questions About Triglyceride-Glucose Index and Hypertension
Q: How is the triglyceride-glucose index calculated?
A: The TyG index uses this formula: ln(fasting triglycerides × fasting glucose) / 2, where "ln" means natural logarithm. Most electronic health records and research databases calculate this automatically, so you rarely need to do the math yourself.
Q: What counts as an elevated triglyceride-glucose index?
A: Different studies use slightly different cutoffs, typically ranging from 8.5 to 9.0. Your healthcare provider can interpret your specific result in context of your health status and other risk factors. Higher values indicate greater insulin resistance.
Q: Can I improve my triglyceride-glucose index?
A: Absolutely. Lifestyle modifications that improve insulin sensitivity—exercise, dietary changes, weight loss, stress management, and adequate sleep—all tend to lower TyG index values over time.
Q: Is triglyceride-glucose index better than other measures of insulin resistance?
A: The TyG index compares favorably to more complicated measures of insulin resistance like HOMA-IR while requiring only standard blood work. Different measures provide complementary information, so your provider might use multiple approaches depending on clinical context.
Q: Do I need to fast before getting a triglyceride-glucose index?
A: Yes—both triglycerides and glucose require fasting measurement (typically 8-12 hours without food) to be interpretable. Make sure your healthcare provider knows this applies to your lab work.
Q: Can triglyceride-glucose index predict who will develop hypertension?
A: Based on these five studies, yes—elevated TyG index predicts increased hypertension risk, particularly in postmenopausal women and those with metabolic syndrome. However, individual risk varies based on genetics, age, and other factors.
Q: Are there medications that improve triglyceride-glucose index?
A: Some diabetes and cholesterol medications may improve TyG index values, but lifestyle modification remains the cornerstone of management. Always discuss medication options with your healthcare provider.
Q: Is triglyceride-glucose index useful in younger people?
A: While these studies focused on middle-aged and older populations, the underlying biology of insulin resistance applies across ages. Catching and addressing elevated TyG index early could prevent decades of hypertension risk.
Key Takeaways: What You Need to Remember
The triglyceride-glucose index (TyG index) is a simple, inexpensive marker combining fasting triglycerides and glucose that reflects insulin resistance.
Five recent research studies confirm that an elevated TyG index is consistently associated with increased hypertension risk across diverse populations.
Postmenopausal women show particularly strong associations between the TyG index and hypertension, suggesting special attention for this vulnerable group.
Pre-hypertension and hypertension are both associated with TyG index abnormalities, creating opportunities for early intervention.
Long-term prospective data links elevated TyG index not just to hypertension but to cardiovascular disease and mortality—making this a serious health marker.
Different diagnostic criteria for hypertension don't change the fundamental TyG index and hypertension relationship, supporting global applicability.
Insulin resistance—the mechanism underlying the TyG index—drives hypertension through multiple pathways that affect blood vessels, kidney function, and nervous system activity.
Lifestyle modification targeting insulin sensitivity through exercise, diet, weight management, and stress reduction can improve the TyG index and blood pressure.
Healthcare providers should consider incorporating TyG index assessment into routine cardiovascular risk screening.
If you have an elevated TyG index, work with your healthcare team on personalized strategies to improve metabolic health and prevent serious cardiovascular complications.
Author’s Note
This article synthesizes evidence from recent peer-reviewed studies (2024–2026) examining the relationship between the triglyceride–glucose (TyG) index, insulin resistance, and hypertension. The TyG index is presented as a practical surrogate marker of metabolic dysfunction, derived from routinely available laboratory parameters, and evaluated across diverse populations and study designs, including cross-sectional analyses, meta-analyses, and prospective cohort data.
The purpose of this article is educational and informational, aiming to translate complex metabolic and cardiovascular research into clinically meaningful insights for healthcare professionals and scientifically informed readers. While current evidence supports a consistent association between elevated TyG index values and increased risk of hypertension and adverse cardiovascular outcomes, the findings discussed do not imply direct causality and should be interpreted within the context of individual patient risk profiles.
This content is not intended to replace personalized medical advice, diagnosis, or treatment. Clinical decisions should be based on comprehensive assessment by qualified healthcare professionals, incorporating patient history, physical examination, laboratory evaluation, and current clinical guidelines.
Related Articles
Forget BMI: Metabolic Health Is the Real Key to Heart Disease Risk | DR T S DIDWAL
hsCRP Explained: What Inflammation Means for Your Heart | DR T S DIDWAL
What’s New in the 2025 Blood Pressure Guidelines? A Complete Scientific Breakdown | DR T S DIDWAL
Low-Fat vs. Low-Carb: Which Diet is Best for Weight Loss? | DR T S DIDWAL
5 Steps to Reverse Metabolic Syndrome: Diet, Habit, & Lifestyle Plan | DR T S DIDWAL
The Role of Cholesterol in Health and Disease: Beyond the "Bad" Label | DR T S DIDWAL
Lowering Cholesterol with Food: 4 Phases of Dietary Dyslipidemia Treatment | DR T S DIDWAL
The Best Dietary Fat Balance for Insulin Sensitivity, Inflammation, and Longevity | DR T S DIDWAL
References
Hao, H., Geng, H., & Ma, M. (2026). Association between triglyceride glucose index and hypertension according to different diagnostic criteria. International Journal of General Medicine, 18, 43–53. https://doi.org/10.2147/IJGM.S499194
He, D., Huang, Y., Ni, X., et al. (2026). Prospective associations of triglyceride-glucose related indices with cardiovascular disease and mortality in individuals with metabolic syndrome: Evidence from the UK biobank. Cardiovascular Diabetology. https://doi.org/10.1186/s12933-025-03070-3
Lukito, A. A., Kamarullah, W., Huang, I., & Pranata, R. (2024). Association between triglyceride-glucose index and hypertension: A systematic review and meta-analysis. Narra Journal, 4(2), e951. https://doi.org/10.52225/narra.v4i2.951
Wang, A., Li, R., Li, X., et al. (2026). Association of the triglyceride-glucose series indices with hypertension and pre-hypertension in Anhui China. Scientific Reports, 16, 3165. https://doi.org/10.1038/s41598-025-33152-x
Zhang, B., Jiang, D., Ma, H., & Liu, H. (2025). Association between triglyceride-glucose index and its obesity indicators with hypertension in postmenopausal women: A cross-sectional study. Frontiers in Nutrition, 12, Article 1623697. https://doi.org/10.3389/fnut.2025.1623697