hsCRP Explained: What Inflammation Means for Your Heart
Everything you need to know about C-Reactive Protein. From interpreting your test results to the latest treatments, learn how to manage your inflammatory health
HEART
Dr. T.S. Didwal, M.D.(Internal Medicine)
12/25/202512 min read
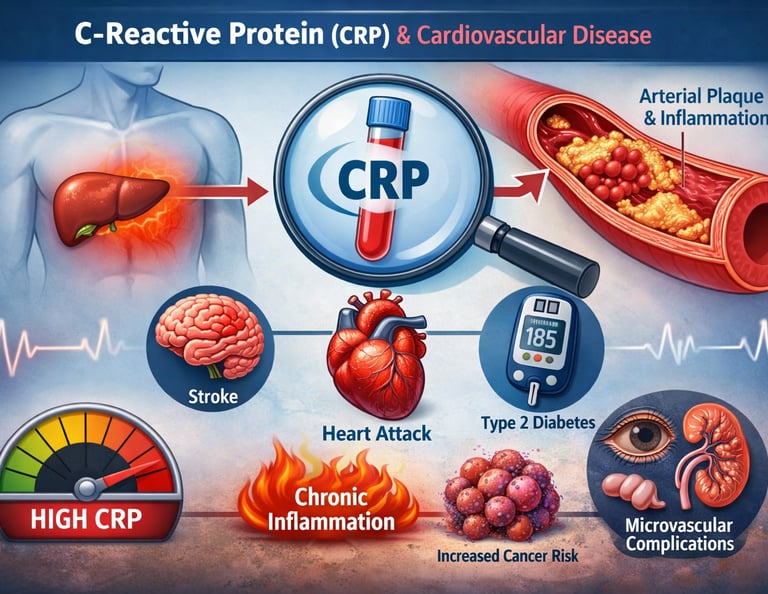
For decades, heart disease risk has been judged largely by numbers we can easily measure—cholesterol, blood pressure, and blood sugar. Yet many people who suffer heart attacks have cholesterol levels that look “normal.” This unsettling paradox has forced scientists to ask a deeper question: What are we missing? Increasingly, the answer points to chronic inflammation, quietly smoldering inside blood vessels long before symptoms appear. At the center of this discovery is high-sensitivity C-reactive protein (hsCRP), a blood marker that reveals low-grade inflammation invisible to routine tests.
In 2025, landmark research and the American College of Cardiology (ACC) Scientific Statement confirmed that inflammation is not merely a bystander but a core driver of atherosclerosis and cardiovascular events, independent of traditional risk factors (Mensah et al., 2025). Large cohort studies now show that individuals—particularly women and patients with diabetes—can face substantial heart risk despite optimal cholesterol and glucose control if hsCRP remains elevated (Ridker et al., 2025; Basil et al., 2025).
This growing body of evidence is reshaping preventive cardiology. Measuring hsCRP offers clinicians a clearer window into residual inflammatory risk, helping identify people who might otherwise be falsely reassured. Understanding inflammation is no longer optional—it is becoming essential to truly personalized heart-disease prevention.
Clinical Pearls
The "Residual Risk" Shift: Achieving target LDL levels is only half the battle; if your hsCRP remains above 2.0 mg/L, your risk for a cardiac event remains high, necessitating a look at targeted anti-inflammatory options.
The SMuRF-less Paradox: Never ignore high inflammation in "healthy" patients. In women without standard modifiable risk factors (SMuRFs), elevated hsCRP is a powerful, independent predictor of future heart disease that traditional screenings miss.
The "Snapshot" Rule: Inflammation is dynamic. Because hsCRP is highly sensitive, a single high reading may reflect a recent minor infection or intense exercise; always confirm a "chronic" state with a second test 2–4 weeks later.
Atherosclerosis as Biology, Not Just Plumbing: 2025 research emphasizes that heart disease isn't just "clogged pipes" caused by fat; it is a biological immune response where inflammation acts as the fuel that makes arterial plaques unstable and prone to rupture.
The Diabetes-Inflammation Link: In Type 2 Diabetes, hsCRP often predicts microvascular damage (to eyes and kidneys) more accurately than blood sugar ($HbA1c$) alone, marking inflammation as the primary link between metabolic dysfunction and vascular decay.
Dual-Path Prevention: The gold standard of care is now the simultaneous reduction of both lipids and inflammation. Addressing one without the other is akin to wearing a seatbelt but driving without brakes.
Why C-Reactive Protein Matters for Your Heart Health
C-reactive protein is an inflammatory marker produced by your liver in response to inflammation throughout your body. Think of it as your body's alarm system—when tissues are damaged or under stress, your liver produces more CRP.
High-sensitivity C-reactive protein (hsCRP) is a more precise measurement of CRP that can detect lower levels of inflammation in your bloodstream. This enhanced sensitivity makes it far more useful for cardiovascular risk assessment than standard CRP testing.
Here's why this matters: systemic inflammation has been increasingly recognized as a fundamental driver of atherosclerosis (plaque buildup in arteries), which directly leads to heart attacks and strokes.
The 2025 ACC Scientific Statement: The New Gold Standard
Study Overview: Mensah et al. (2025)
The American College of Cardiology recently published a landmark scientific statement on inflammation and cardiovascular disease that consolidates our evolving understanding of this critical relationship (Mensah et al., 2025).
Key Takeaways:
Inflammation is now recognized as a central mechanism in the development of cardiovascular disease, independent of traditional risk factors
hsCRP testing has emerged as a valuable tool for risk stratification in clinical practice
The statement emphasizes that measuring inflammatory markers alongside conventional risk factors provides superior predictive accuracy for identifying patients who will develop heart disease
Healthcare providers are encouraged to consider hsCRP levels when making treatment decisions for at-risk populations
Why This Matters: This ACC statement represents a paradigm shift, moving beyond the traditional "cholesterol-focused" approach to a more nuanced understanding of how chronic inflammation drives cardiovascular events. The recognition of systemic inflammation as an independent risk factor opens new doors for prevention and early intervention.
Women Without Traditional Risk Factors: The "SMuRF-Less but Inflamed" Paradox
Study Overview: Ridker et al. (2025)
One of the most intriguing findings from 2025 involves women who seem healthy by conventional standards but show elevated inflammatory markers. Ridker and colleagues (2025) investigated what they cleverly termed the "SMuRF-less but inflamed" phenomenon—a catchy way of describing patients with no standard modifiable risk factors who nonetheless have increased cardiovascular risk due to elevated C-reactive protein levels.
Key Takeaways:
Approximately 5-10% of women have no conventional cardiovascular risk factors (no high cholesterol, no hypertension, no diabetes) yet have elevated hsCRP levels
These "inflamed-but-otherwise-healthy" women have significantly higher rates of cardiovascular events compared to women with low CRP levels and no risk factors
hsCRP testing is essential for identifying this high-risk population that would be completely missed by traditional risk assessment tools
The findings challenge the assumption that cardiovascular risk is determined solely by cholesterol, blood pressure, and glucose metabolism
Women with elevated hsCRP but low lipid levels may still benefit from anti-inflammatory interventions
Clinical Implications: This research highlights a critical gap in current cardiovascular screening practices (Ridker et al., 2025). Many women with significant heart disease risk are being reassured that they're healthy when, in fact, ongoing inflammation is quietly damaging their arteries. The study underscores the importance of personalized medicine and comprehensive risk stratification.
Type 2 Diabetes: When Inflammation and Metabolic Dysfunction Collide
Study Overview: Basil et al. (2025)
Patients with type 2 diabetes represent a particularly vulnerable population for cardiovascular disease, and Basil and colleagues (2025) examined precisely how hsCRP levels refine risk assessment in this group.
Key Takeaways:
Patients with type 2 diabetes show distinctly elevated hsCRP levels compared to non-diabetic populations
Elevated hsCRP in diabetic patients predicts cardiovascular complications even after adjusting for traditional risk factors like HbA1c levels and lipid profiles
Inflammatory markers provide independent prognostic information beyond standard glycemic control measures
The relationship between hsCRP and cardiovascular risk is particularly strong in this population, suggesting that chronic inflammation may be a key link between diabetes and heart disease
Clinical management of diabetic patients should incorporate hsCRP testing as part of routine cardiovascular risk assessment
Why This Matters for Diabetics: Patients with type 2 diabetes often focus exclusively on controlling blood sugar, but recent evidence (Basil et al., 2025; Stanimirovic et al., 2022) demonstrates that managing systemic inflammation is equally crucial for preventing heart attacks and strokes. Two diabetic patients with identical glucose control might have vastly different cardiovascular risk profiles based on their inflammatory status.
The Diabetes-Inflammation Connection: A Deeper Look
Study Overview: Stanimirovic et al. (2022)
While slightly older than the 2025 studies, Stanimirovic and colleagues' (2022) comprehensive review provides essential context for understanding the role of C-reactive protein in diabetic inflammation.
Key Takeaways:
Type 2 diabetes is fundamentally a state of chronic low-grade inflammation that affects multiple organ systems
CRP serves as both a marker and potentially an active participant in the inflammatory cascade that damages blood vessels
The inflammatory pathway connects insulin resistance, glucose dysmetabolism, and cardiovascular disease in diabetic patients
Understanding this inflammatory mechanism opens possibilities for targeted interventions beyond traditional diabetes medications
Anti-inflammatory approaches to diabetes management might prevent microvascular and macrovascular complications
The Bigger Picture: This review demonstrates that diabetes isn't simply about blood sugar—it's about a pervasive inflammatory state that threatens multiple organs simultaneously.
Microvascular Complications and Hidden Inflammation
Study Overview: Dhadwad & Yadav (2025)
The relationship between hsCRP levels and microvascular complications (small blood vessel damage) in diabetic patients reveals yet another dimension of inflammation's impact. Dhadwad and Yadav (2025) investigated how inflammatory markers predict the development of complications like diabetic retinopathy (eye damage), nephropathy (kidney damage), and neuropathy (nerve damage).
Key Takeaways:
Elevated hsCRP strongly associates with the presence and severity of microvascular complications in diabetes patients
Inflammatory markers may predict which diabetic patients will develop complications, even before standard clinical indicators appear
The connection between systemic inflammation and microvascular damage suggests that anti-inflammatory therapy might prevent these debilitating complications
Early identification of patients with high hsCRP levels could enable preventive interventions before irreversible damage occurs
Inflammatory markers provide valuable insight into the mechanisms driving diabetic complications beyond glucose toxicity
Chronic Inflammation, Insulin Resistance, and Cancer Risk: An Unexpected Connection
Study Overview: Zheng et al. (2025)
Perhaps most provocatively, Zheng and colleagues (2025) examined the temporal relationship between chronic inflammation and insulin resistance and their combined cumulative effect on cancer risk. This longitudinal cohort study reveals that chronic inflammation and metabolic dysfunction don't just threaten heart health—they increase cancer risk through interconnected biological mechanisms.
Key Takeaways:
Chronic inflammation and insulin resistance share common pathways and often occur together in the same individuals
The combined effect of elevated hsCRP and insulin resistance on cancer risk exceeds what either factor alone would predict
This suggests a potential vicious cycle: systemic inflammation promotes insulin resistance, which further amplifies inflammatory signals, increasing risk for both cardiovascular disease and cancer
Early intervention targeting inflammatory markers and metabolic health might prevent multiple chronic diseases simultaneously
The findings underscore the importance of viewing health holistically—addressing inflammation has implications far beyond heart disease
Relevance to Your Health: This research (Zheng et al., 2025) suggests that maintaining low inflammatory status is crucial not just for heart health but for comprehensive disease prevention across multiple conditions.
Real-World Evidence: The PLUTUS Study on Systemic Inflammation in America
Study Overview: Lv et al. (2025)
The PLUTUS study (Lv et al., 2025) provides real-world evidence on the prevalence and clinical characteristics of patients with hsCRP testing and test-confirmed systemic inflammation among individuals with atherosclerotic cardiovascular disease with or without chronic kidney disease in the United States.
Key Takeaways:
High-sensitivity CRP testing has become increasingly prevalent in clinical practice for patients with established atherosclerotic disease
A substantial proportion of U.S. patients with atherosclerotic cardiovascular disease show confirmed systemic inflammation despite standard treatments
Patients with both cardiovascular disease and chronic kidney disease face particularly elevated inflammatory burden
The combination of CVD and CKD creates a synergistic inflammatory environment that substantially increases risk for cardiovascular events
Current standard therapies may not adequately address the inflammatory component of atherosclerotic disease
Clinical Translation: This study demonstrates that inflammation remains a significant health problem in real-world patient populations, suggesting that opportunities exist to improve outcomes through targeted anti-inflammatory approaches.
How to Interpret Your hsCRP Results: A Practical Guide
Understanding what your hsCRP level means is crucial for informed discussions with your healthcare provider:
Less than 1.0 mg/L: Low risk of cardiovascular disease
1.0 to 3.0 mg/L: Intermediate risk; warrants monitoring and lifestyle modifications
Greater than 3.0 mg/L: Higher risk; consider discussion with your doctor about interventions
Greater than 10 mg/L: May indicate acute infection or severe inflammation; requires investigation
Important Note: A single hsCRP measurement represents a snapshot in time. Your inflammatory status can fluctuate based on stress, infection, exercise, diet, and sleep. Repeat testing often provides more reliable information than isolated measurements.
Key Takeaways from the 2025 Research
Inflammation is independent: Chronic inflammation, measured by hsCRP, predicts cardiovascular disease independently of traditional risk factors like cholesterol and blood pressure.
Women need targeted screening: Women without conventional risk factors but with elevated hsCRP face significant heart disease risk and deserve comprehensive screening.
Diabetes demands inflammatory assessment: Patients with type 2 diabetes should have hsCRP testing as part of routine cardiovascular evaluation, separate from glucose control monitoring.
Complications extend beyond the heart: Chronic inflammation and insulin resistance increase risk for microvascular complications, cancer, and potentially other chronic diseases.
Real-world inflammation persists: Despite standard treatments, many cardiovascular patients in the U.S. maintain elevated inflammatory markers, suggesting opportunities for improved management.
Early detection matters: hsCRP testing identifies at-risk patients before they develop symptomatic disease, enabling preventive interventions.
FAQ: Common Questions About hsCRP and Cardiovascular Health
Q: Should everyone get hsCRP testing? A: The 2025 ACC statement recommends hsCRP testing for those with borderline cardiovascular risk or established risk factors. Discussion with your healthcare provider about individual need is essential.
Q: Can I lower my hsCRP levels naturally? A: Yes! Exercise, anti-inflammatory diet patterns (Mediterranean or DASH), weight loss, adequate sleep, stress management, and smoking cessation all reduce CRP levels.
Q: Is elevated hsCRP the same as an active infection? A: No. Acute infection causes very high CRP levels (often >10 mg/L), while chronic cardiovascular inflammation typically produces modest elevations (1.0-3.0 mg/L). Your doctor can differentiate these.
Q: Do statins reduce hsCRP? A: Yes. Statins have both lipid-lowering and anti-inflammatory effects, reducing hsCRP levels in many patients.
Q: Can I have normal cholesterol but dangerous inflammation? A: Absolutely. The 2025 research shows this occurs in 5-10% of the population. This is precisely why comprehensive risk assessment matters.
Q: How often should I retest hsCRP? A: There's no universal standard, but annual testing for at-risk individuals or those on interventions is reasonable. Discuss frequency with your healthcare provider.
Q: Does exercise reduce hsCRP quickly? A: Regular aerobic exercise reduces CRP levels significantly over weeks to months. High-intensity interval training appears particularly effective.
Q: Are there medications that reduce inflammation without affecting cholesterol? A: Research into targeted anti-inflammatory agents continues. Some patients benefit from colchicine or other anti-inflammatory approaches, though these remain specialized.
What You Can Do Today: Practical Steps to Reduce Inflammation
Dietary Approaches
Emphasize antioxidant-rich foods: berries, leafy greens, nuts, and seeds
Choose omega-3 fatty acids: fatty fish (salmon, sardines), flaxseeds, walnuts
Reduce processed foods, refined carbohydrates, and sugary beverages
Consider the Mediterranean diet or DASH diet pattern, both with strong evidence for anti-inflammatory effects
Lifestyle Modifications
Exercise regularly: Aim for 150 minutes of moderate aerobic activity weekly
Manage stress: Meditation, yoga, and mindfulness reduce inflammatory markers
Prioritize sleep: 7-9 hours nightly supports immune regulation and reduces inflammation
Maintain healthy weight: Even modest weight loss reduces systemic inflammation
Medical Considerations
Discuss hsCRP testing with your healthcare provider, especially if you have risk factors or are a woman without conventional risk markers
If elevated, work with your doctor on a comprehensive management plan
Consider preventive medications if recommended based on your individual risk profile
The Future of Inflammation Management
The 2025 research landscape suggests several emerging directions:
Targeted Anti-Inflammatory Therapy: Modern cardiovascular management has shifted toward a "dual-pathway" strategy that addresses both lipids and inflammation. Statins (e.g., Atorvastatin) remain the foundation, lowering LDL cholesterol while providing moderate anti-inflammatory benefits. However, for patients with "residual inflammatory risk," targeted therapies like low-dose Colchicine are now utilized to specifically inhibit inflammasome pathways without altering cholesterol.1 Emerging IL-6 Inhibitors (e.g., Ziltivekimab) offer even more potent CRP reduction, particularly for high-risk patients with kidney disease, while SGLT2 Inhibitors provide a metabolic approach by reducing systemic stress in diabetic and heart failure populations.
Personalized Medicine: As our understanding of inflammatory mechanisms deepens, risk stratification will become increasingly individualized, moving beyond one-size-fits-all approaches.
Multi-Disease Prevention: Addressing inflammation simultaneously prevents cardiovascular disease, diabetes complications, and potentially cancer—suggesting that anti-inflammatory approaches offer remarkable efficiency for comprehensive health.
Technology Integration: Emerging biomarkers and continuous monitoring devices may enable real-time inflammatory status tracking, allowing rapid intervention when inflammation rises.
Call to Action: Take Control of Your Inflammatory Status
The evidence is clear: C-reactive protein matters for your heart health, and 2025's research reveals that traditional risk assessment alone misses critical information about cardiovascular risk.
Here's what you should do:
Schedule a conversation with your healthcare provider about whether hsCRP testing is appropriate for you, especially if you're a woman without obvious risk factors, have diabetes, or have a family history of heart disease.
Assess your lifestyle: Review the dietary and lifestyle modifications above. Small changes compound into significant improvements in inflammatory status.
Stay informed: Share this research with your healthcare team. 2025's evidence should influence how they approach your cardiovascular risk assessment.
Think long-term: Managing inflammation isn't about perfect compliance—it's about consistent, sustainable changes that keep your arteries healthy for decades.
Get tested: If your doctor recommends hsCRP testing, follow through. Knowledge about your inflammatory status empowers informed decision-making.
Your heart health isn't determined by fate—it's shaped by what you do today. The emerging understanding of inflammation's role in cardiovascular disease offers unprecedented opportunity for prevention and early intervention.
Important Clinical Note on Anti-Inflammatory Therapies:
While targeted anti-inflammatory agents such as colchicine and emerging IL-6 pathway inhibitors have demonstrated cardiovascular benefit in selected high-risk patients, they are not appropriate for universal use. Colchicine should be avoided or used with caution in individuals with advanced renal or hepatic impairment, significant drug–drug interactions (notably with strong CYP3A4 or P-glycoprotein inhibitors), or a history of severe gastrointestinal intolerance. Biologic anti-inflammatory therapies may increase susceptibility to infection and require careful patient selection and monitoring. All anti-inflammatory treatments should be prescribed only after exclusion of acute infection and as part of a clinician-guided, individualized risk–benefit assessment, rather than as standalone or preventive therapy in low-risk individuals.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Individual circumstances vary, and treatment decisions should always be made in consultation with qualified healthcare professionals.
Related Articles
Beyond Cholesterol: Life-Saving Latest Blood Tests to Prevent Heart Attacks | DR T S DIDWAL
The Metabolic Triad: Why Diabetes, Obesity & CVD Are One Epidemic | DR T S DIDWAL
What’s New in the 2025 Blood Pressure Guidelines? A Complete Scientific Breakdown | DR T S DIDWAL
References
Basil, B., Mohammed, J. A., Mba, I. N., et al. (2025). High-sensitivity c-reactive protein and cardiovascular disease risk assessment in a population of type 2 diabetes mellitus patients. BMC Cardiovascular Disorders, 25, 498. https://doi.org/10.1186/s12872-025-04975-3
Dhadwad, J., & Yadav, P. (2025). Association of hsCRP levels with microvascular complications in [Title continues]. Journal of Clinical and Diagnostic Research, 19(9), OC15–OC18. https://doi.org/10.7860/JCDR/2025/79982/21517
Lv, L., Rajpura, J., Liu, M., Strum, M., Chastek, B., Johnson, J., & Gluckman, T. J. (2025). Prevalence and clinical characteristics of patients with hsCRP testing and test-confirmed systemic inflammation among individuals with atherosclerotic cardiovascular disease with or without chronic kidney disease in the United States (PLUTUS). American Journal of Preventive Cardiology, 21, 100950. https://doi.org/10.1016/j.ajpc.2025.100950
Mensah, G. A., Arnold, N., Prabhu, S. D., Ridker, P. M., & Welty, F. K. (2025). Inflammation and cardiovascular disease: 2025 ACC scientific statement: A report of the American College of Cardiology. Journal of the American College of Cardiology. https://doi.org/10.1016/j.jacc.2025.08.047
Ridker, P. M., Figtree, G. A., Moorthy, M. V., Mora, S., & Buring, J. E. (2025). C-reactive protein and cardiovascular risk among women with no standard modifiable risk factors: Evaluating the 'SMuRF-less but inflamed'. European Heart Journal, ehaf658. Advance online publication. https://doi.org/10.1093/eurheartj/ehaf658
Stanimirovic, J., Radovanovic, J., Banjac, K., Obradovic, M., Essack, M., Zafirovic, S., Gluvic, Z., Gojobori, T., & Isenovic, E. R. (2022). Role of C-reactive protein in diabetic inflammation. Mediators of Inflammation, 2022, 3706508. https://doi.org/10.1155/2022/3706508
Zheng, X., Wang, Y., Chen, Y., et al. (2025). Temporal relationship between chronic inflammation and insulin resistance and their combined cumulative effect on cancer risk: A longitudinal cohort study. BMC Public Health, 25, 1501. https://doi.org/10.1186/s12889-025-22632-4