Beyond Cholesterol: Life-Saving Latest Blood Tests to Prevent Heart Attacks
Discover how cutting-edge cardiovascular biomarkers like ApoB, hs-CRP, and NT-proBNP detect heart disease early, guide treatment, and prevent heart attacks
HEART
Dr. T.S. Didwal, M.D.(Internal Medicine)
1/12/202613 min read
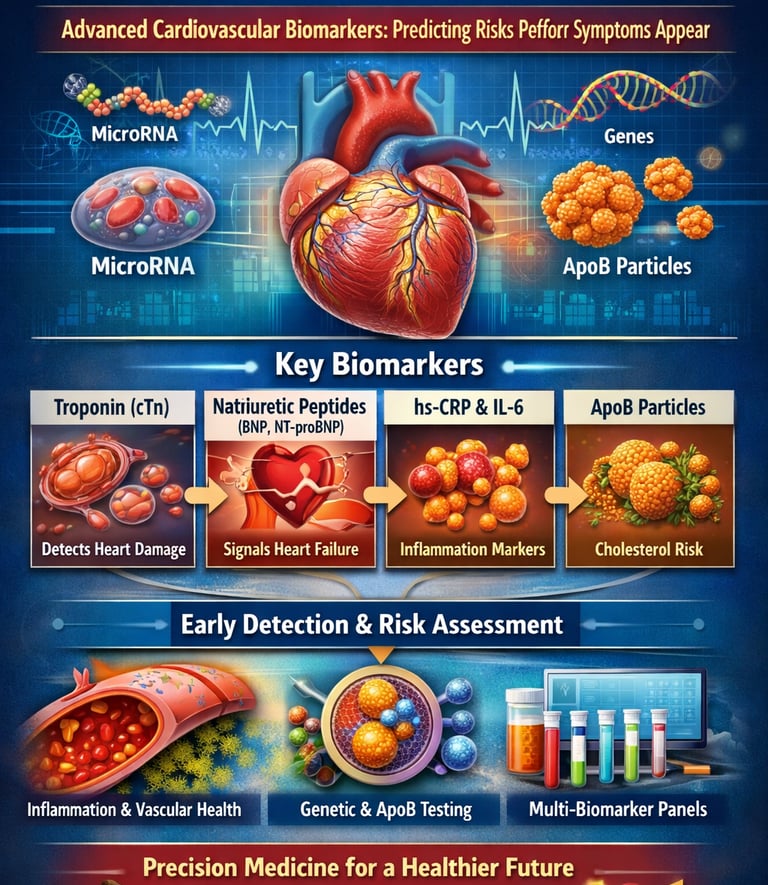
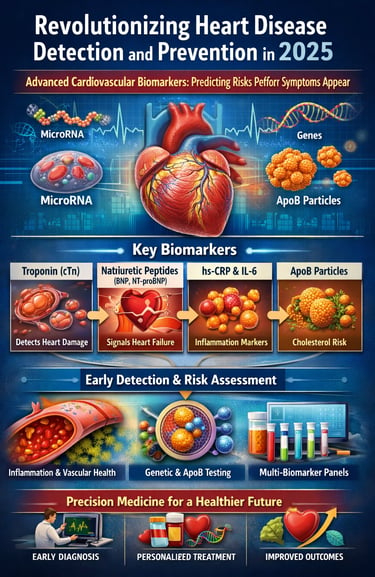
Heart disease remains the world’s leading killer—but today, science offers a powerful advantage that didn’t exist a decade ago. Advances in cardiovascular biomarker technology now allow clinicians to detect heart disease long before symptoms appear, catching problems at their earliest—and most reversible—stages. Modern biomarkers act like molecular “signals” released into the blood when inflammation rises, vessels stiffen, or heart cells experience stress or injury. Research shows these biomarkers can reveal hidden cardiovascular risk even when routine tests like cholesterol appear normal (Netala et al., 2025).
High-sensitivity troponins detect microscopic heart muscle injury that older tests could never identify (Nazir et al., 2025). Natriuretic peptides such as BNP and NT-proBNP warn of cardiac strain and evolving heart failure, often months before symptoms surface (Netala et al., 2025). Inflammatory biomarkers—including hs-CRP, IL-6, and MPO—uncover silent vascular inflammation, a major driver of plaque instability and heart attacks (Koo et al., 2025).
Even more revolutionary, ApoB particle counts now outperform LDL cholesterol for predicting coronary artery disease, shifting the future of preventive cardiology toward particle-based risk assessment (Morze et al., 2025). Together, these biomarkers offer a clearer, more precise picture of cardiovascular health—enabling earlier diagnosis, personalized prevention, and targeted treatment strategies that can radically change long-term outcomes.
Clinical Pearls
1. ApoB over LDL
Traditional cholesterol tests measure the weight of your LDL, but the latest 2025 research (Morze et al.) suggests we should be counting the particles. Think of LDL as the weight of passengers and ApoB as the number of cars on the road. Even if the passengers are light, a high number of cars (ApoB particles) increases the risk of a "crash" (plaque buildup) in your arteries.
Clinical Insight: Ask for an ApoB test to see your true particle count; it is a more precise predictor of heart disease than standard LDL.
2. hs-CRP
Heart disease isn't just about "clogged pipes"; it’s about "fire" (inflammation). The hs-CRP biomarker acts like a sensitive smoke detector. If this level is high, it means your immune system is attacking your artery walls, making any existing plaque much more likely to rupture and cause a heart attack.
Clinical Insight: A low cholesterol score doesn't mean you're safe if your inflammation (hs-CRP) is high. Treating inflammation is just as vital as treating lipids.
3. Lp(a)
Lp(a) is a "sticky" cholesterol particle determined entirely by your DNA, not your diet. 2025 guidelines emphasize that everyone should have this tested at least once in their life. While you can't change the number through exercise, knowing it is high allows your doctor to be much more aggressive with other protective measures.
Clinical Insight: If you have a family history of early heart attacks despite "healthy" lifestyles, an Lp(a) test could reveal the hidden genetic culprit.
4. NT-proBNP
If your heart were an engine, NT-proBNP would be the gauge that measures internal pressure. When the heart muscle is stretched or overworked—common in heart failure or untreated high blood pressure—it releases this "stress hormone" into the blood.
Clinical Insight: This is the gold standard for catching heart failure early, often before you even feel significant shortness of breath.
5. High-Sensitivity Troponin
In the past, troponin tests only caught large-scale heart attacks. Now, High-Sensitivity Troponins can detect "micro-leaks" from the heart muscle. This allows doctors to see if your heart is under chronic stress from things like extreme exercise, sleep apnea, or subtle coronary disease.
Clinical Insight: Tiny elevations in troponin are "warning shots." They give you and your doctor a window of opportunity to intervene before a major event occurs.
6. The "Whole Picture" (The Multi-Marker Approach)
The 2025-2026 consensus is that no single number tells the whole story. Your heart health is a puzzle involving damage (troponin), strain (BNP), inflammation (CRP), and particle count (ApoB). Using a multi-biomarker panel is like using GPS, radar, and a camera simultaneously to navigate—it provides a 360-degree view of your risk.
Clinical Insight: Don't obsess over one "bad" number. Look for the trends across your entire panel to understand your true cardiovascular trajectory.
Cardiovascular Biomarkers: Revolutionary Tools for Heart Disease Detection and Prevention
What Are Cardiovascular Biomarkers and Why Should You Care?
Think of cardiovascular biomarkers as your heart's early warning system. These are measurable substances in your blood, tissues, or other body fluids that signal what's happening inside your cardiovascular system. When something goes wrong—like inflammation, damaged heart cells, or metabolic dysfunction—these biomarkers change in detectable ways.
According to Netala et al. (2025), cardiovascular biomarkers serve as powerful tools for precision diagnosis and prognosis, enabling healthcare providers to move beyond one-size-fits-all approaches. Instead of waiting for symptoms to appear, these molecular messengers allow doctors to intervene early, potentially preventing heart attacks, strokes, and other life-threatening events.
The Evolution of Cardiac Biomarkers: From Basic to Precision
The landscape of cardiac biomarker testing has transformed dramatically. Traditional markers like cholesterol gave us important information, but modern biomarkers offer unprecedented insights into cardiovascular risk stratification and disease progression. Let's explore what cutting-edge research reveals about these game-changing diagnostic tools.
Breaking Down the Latest Research: Seven Studies Shaping the Future
1. Comprehensive Overview of Precision Cardiovascular Diagnostics
Netala and colleagues (2025) published a comprehensive review in the International Journal of Molecular Sciences examining how biomarkers enable precision medicine in cardiology. Their research categorizes cardiovascular biomarkers into several key groups:
Key Takeaways:
Cardiac troponins (cTn) remain the gold standard for detecting myocardial injury and diagnosing acute heart attacks
Natriuretic peptides (BNP and NT-proBNP) excel at identifying heart failure and assessing its severity
Inflammatory biomarkers like high-sensitivity C-reactive protein (hs-CRP) help predict future cardiovascular events
Emerging markers including microRNAs and metabolic biomarkers promise even earlier disease detection
Multi-biomarker approaches outperform single markers for comprehensive cardiovascular risk assessment
The researchers emphasize that integrating multiple biomarkers creates a more complete picture of heart health, allowing for personalized treatment strategies based on individual risk profiles (Netala et al., 2025).
2. Vascular and Cardiovascular Research Frontiers in 2025
Kishimoto and Higashi (2025) provided an updated perspective on vascular health biomarkers in Hypertension Research. Their review highlights how understanding vascular function through biomarkers can prevent cardiovascular complications before structural damage occurs.
Key Takeaways:
Endothelial dysfunction markers serve as early indicators of vascular disease
Advanced imaging combined with biomarker analysis improves hypertension management
Vascular inflammation biomarkers predict arterial stiffness and atherosclerosis progression
Novel markers related to oxidative stress and nitric oxide availability show promise for assessing vascular health
Integrated vascular-cardiovascular biomarker panels enhance risk prediction models
This research underscores that vascular health is inseparable from overall cardiovascular wellness, and biomarkers targeting blood vessel function provide critical preventive insights (Kishimoto & Higashi, 2025).
3. Early Detection and Risk Stratification Advances
Nazir and colleagues (2025) conducted an extensive literature review for Health Science Reports, focusing specifically on biomarkers for early cardiovascular disease detection and risk stratification. Their analysis reveals how emerging biomarkers are changing clinical practice.
Key Takeaways:
High-sensitivity troponins detect even minor heart muscle damage, enabling earlier intervention
Galectin-3 and ST2 emerge as valuable biomarkers for heart failure prognosis
Lipoprotein(a) (Lp(a)) testing identifies patients with genetically elevated cardiovascular risk
Coronary artery calcium scoring combined with biomarker panels improves risk prediction accuracy
Artificial intelligence integration with biomarker data enhances personalized risk assessment
The authors emphasize that combining traditional and novel biomarkers creates a more nuanced understanding of individual cardiovascular risk, particularly in asymptomatic populations (Nazir et al., 2025).
4. Inflammatory Markers as Cardiovascular Disease Predictors
Koo and colleagues (2025) conducted a systematic review published in Research in Cardiovascular Medicine, specifically examining advanced inflammatory biomarkers as predictors of cardiovascular diseases. Their work highlights inflammation's central role in heart disease development.
Key Takeaways:
High-sensitivity C-reactive protein (hs-CRP) consistently predicts future cardiovascular events across diverse populations
Interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α) correlate with atherosclerotic plaque instability
Myeloperoxidase (MPO) helps identify patients at risk for acute coronary events
Inflammatory cytokine panels outperform single markers for comprehensive risk assessment
Anti-inflammatory therapies guided by biomarker levels show promise in clinical trials
This systematic review reinforces that chronic inflammation drives cardiovascular disease progression, making inflammatory biomarkers essential for both diagnosis and treatment monitoring (Koo et al., 2025).
5. Biomarkers in Coronary Artery Disease Monitoring and Prognosis
Rai (2025) examined the current and future applications of biomarkers specifically for coronary artery disease (CAD) in Future Cardiology. This perspective article explores how biomarkers guide treatment decisions and predict outcomes in CAD patients.
Key Takeaways:
Serial troponin measurements help distinguish between stable and unstable coronary syndromes
BNP levels predict heart failure development in CAD patients
Growth differentiation factor-15 (GDF-15) emerges as a prognostic marker for adverse cardiovascular outcomes
Soluble ST2 levels correlate with cardiac remodeling after heart attacks
Future biomarker development will focus on personalized therapy selection and treatment response monitoring
Rai (2025) emphasizes that biomarkers are transitioning from purely diagnostic tools to guides for individualized therapy, helping clinicians choose the most effective interventions for each patient's unique biochemical profile.
6. Precision Cardiovascular Diagnostics Through Multiple Biomarkers
Returning to Netala and colleagues' (2025) comprehensive work, their research details how multi-biomarker strategies improve diagnostic accuracy. The study explores various biomarker categories working together synergistically.
Key Takeaways:
Cardiac-specific troponins I and T provide superior sensitivity for detecting minimal myocardial damage
NT-proBNP levels correlate strongly with heart failure severity and treatment response
D-dimer and fibrinogen help assess thrombotic risk in cardiovascular disease
Homocysteine and apolipoprotein measurements refine metabolic cardiovascular risk assessment
Point-of-care biomarker testing enables rapid emergency department decision-making
The researchers advocate for integrated biomarker panels that capture multiple pathophysiological pathways simultaneously, providing a comprehensive cardiovascular health snapshot (Netala et al., 2025).
7. ApoB-Containing Lipoproteins: Count, Type, and CAD Risk
Morze and colleagues (2025) published groundbreaking research in the European Heart Journal examining apolipoprotein B-containing lipoproteins (ApoB particles) and their relationship to coronary artery disease risk. This study represents a paradigm shift in understanding cholesterol-related cardiovascular risk.
Key Takeaways:
ApoB particle number predicts CAD risk more accurately than traditional LDL cholesterol measurements
Smaller, denser LDL particles carry higher cardiovascular risk than larger particles
ApoB/ApoA1 ratio outperforms conventional lipid ratios for risk stratification
Lipoprotein particle size analysis provides additional prognostic information beyond cholesterol content
Targeting ApoB reduction rather than just LDL-C may improve cardiovascular outcomes
This research challenges conventional wisdom about cholesterol testing, suggesting that counting the actual number of atherogenic particles (via ApoB measurement) provides superior risk assessment compared to measuring cholesterol content alone (Morze et al., 2025).
Understanding the Clinical Applications: From Lab to Life
How Do Doctors Use These Biomarkers?
Cardiovascular biomarkers serve multiple clinical purposes throughout the disease continuum:
Screening and Prevention: In asymptomatic individuals, biomarkers like hs-CRP, Lp(a), and ApoB identify those at elevated risk who might benefit from preventive interventions such as lifestyle modifications or medication. According to the research reviewed, combining traditional risk factors with novel biomarkers significantly improves cardiovascular risk prediction accuracy.
Diagnosis: When someone experiences chest pain or shortness of breath, cardiac troponins help emergency physicians quickly determine whether a heart attack is occurring. BNP levels distinguish between cardiac and non-cardiac causes of breathing difficulties. This rapid biomarker testing can literally save lives by guiding immediate treatment decisions.
Prognosis and Monitoring: After diagnosis, biomarkers help predict outcomes and monitor treatment effectiveness. Serial measurements of NT-proBNP in heart failure patients, for example, guide medication adjustments and indicate when hospitalization might be necessary. Inflammatory markers tracked over time reveal whether anti-inflammatory therapies are working.
Personalized Treatment Selection: Emerging applications include using biomarker profiles to select the most appropriate medications. For instance, patients with elevated inflammatory biomarkers might benefit more from anti-inflammatory therapies, while those with specific metabolic biomarker patterns might respond better to targeted metabolic interventions.
The Multi-Biomarker Approach: Why More Is Better
All seven studies emphasize a consistent theme: multi-biomarker panels outperform single markers. Why? Because cardiovascular disease involves multiple interconnected processes—inflammation, metabolic dysfunction, structural damage, and thrombosis. Measuring markers representing each pathway creates a more complete picture.
Think of it like weather forecasting. Temperature alone tells you something, but combining temperature with humidity, barometric pressure, and wind speed provides much better predictions. Similarly, combining troponins (damage), natriuretic peptides (stress), inflammatory markers (inflammation), and lipid particles (metabolic risk) offers superior cardiovascular risk assessment.
Emerging Biomarkers: The Next Generation
MicroRNAs and Genetic Biomarkers
Research highlighted by Netala et al. (2025) points to microRNAs as particularly promising emerging biomarkers. These small RNA molecules regulate gene expression and appear in altered patterns during cardiovascular disease development. Their advantages include high stability in blood samples and disease-specific expression patterns.
Genetic biomarkers like Lp(a) measurements, discussed across multiple studies, identify individuals with inherited cardiovascular risk factors. Unlike modifiable risk factors, genetic markers help identify people who need more aggressive preventive strategies regardless of their lifestyle.
Metabolic and Proteomic Biomarkers
Advanced metabolic profiling identifies specific metabolic biomarker patterns associated with cardiovascular risk. These metabolomic signatures reflect the complex biochemical environment promoting or protecting against heart disease. Similarly, proteomic biomarkers—measurements of multiple proteins simultaneously—provide comprehensive snapshots of cardiovascular health status.
Practical Implications: What This Means for Patients
Should You Ask Your Doctor About Advanced Biomarker Testing?
If you have cardiovascular risk factors—family history, high blood pressure, diabetes, obesity, or smoking history—discussing comprehensive biomarker testing with your physician makes sense. The research reviewed demonstrates that advanced markers like hs-CRP, Lp(a), ApoB, and NT-proBNP can refine your individual risk assessment beyond traditional cholesterol panels.
For people with established heart disease, serial biomarker monitoring helps optimize treatment. If you have heart failure, regular BNP testing guides medication adjustments. If you've had a heart attack, tracking troponins and inflammatory markers helps assess recovery and predict complications.
Understanding Your Test Results
Modern cardiovascular biomarker panels often include multiple measurements. Here's what some key markers indicate:
High-sensitivity troponin: Elevated levels indicate heart muscle damage, even minimal amounts
NT-proBNP or BNP: Higher values suggest heart strain or failure; levels correlate with severity
hs-CRP: Elevated inflammatory marker associated with increased cardiovascular event risk
ApoB: Number of atherogenic lipoprotein particles; higher numbers mean greater plaque-building risk
Lp(a): Genetically determined risk factor; elevated levels increase cardiovascular risk regardless of LDL cholesterol
Always discuss results with your healthcare provider within the context of your complete clinical picture. Biomarkers inform decisions but don't replace comprehensive medical evaluation.
Key Takeaways
Cardiovascular biomarkers enable earlier disease detection, more accurate risk prediction, and personalized treatment strategies compared to traditional assessment methods.
Multi-biomarker panels combining cardiac damage markers (troponins), stress markers (natriuretic peptides), inflammatory markers (hs-CRP, cytokines), and metabolic markers (ApoB, Lp(a)) provide superior risk assessment compared to single markers.
ApoB particle number predicts coronary artery disease risk more accurately than traditional LDL cholesterol measurements, representing a paradigm shift in lipid-related cardiovascular risk assessment.
Inflammatory biomarkers like hs-CRP, IL-6, and myeloperoxidase help identify patients at risk for cardiovascular events and guide anti-inflammatory therapy decisions.
Emerging biomarkers including microRNAs, genetic markers, and proteomic signatures promise even earlier disease detection and more precise treatment personalization.
Serial biomarker monitoring in patients with established cardiovascular disease guides treatment optimization and predicts complications, improving long-term outcomes.
Point-of-care biomarker testing and AI-enhanced interpretation are making advanced cardiovascular risk assessment more accessible and actionable in diverse clinical settings.
Frequently Asked Questions
Q: Are advanced cardiovascular biomarker tests covered by insurance?
A: Coverage varies by insurer and clinical indication. Traditional biomarkers like troponins and BNP are widely covered when medically indicated. Newer markers like hs-CRP, Lp(a), and ApoB may have variable coverage. Check with your insurance provider and discuss medical necessity with your physician.
Q: How often should cardiovascular biomarkers be tested?
A: Testing frequency depends on individual circumstances. For screening in asymptomatic people, many markers need testing only once or every few years. For monitoring established disease or treatment response, some markers might be measured monthly or quarterly. Your cardiologist will determine the appropriate schedule.
Q: Can biomarker levels be improved through lifestyle changes?
A: Many cardiovascular biomarkers respond to lifestyle modifications. Inflammatory markers like hs-CRP often decrease with weight loss, exercise, and anti-inflammatory diets. Natriuretic peptides may improve with heart failure treatment adherence. However, genetic markers like Lp(a) typically don't respond to lifestyle changes and may require medication.
Q: What's the difference between regular cholesterol tests and ApoB testing?
A: Traditional cholesterol panels measure the amount of cholesterol in lipoprotein particles. ApoB testing counts the actual number of atherogenic particles, regardless of cholesterol content. Research shows particle number better predicts cardiovascular risk because each ApoB particle can contribute to plaque formation.
Q: Are there any risks associated with biomarker testing?
A: Biomarker testing typically requires blood draws, which carry minimal risks (bruising, discomfort). The greater concern is interpreting results correctly and avoiding unnecessary anxiety or interventions based on single abnormal values. Always interpret biomarkers within your complete clinical context with professional guidance.
Q: Can biomarkers predict heart attacks before they happen?
A: While biomarkers can identify elevated risk and sometimes detect early damage, they cannot predict the exact timing of heart attacks. Elevated inflammatory markers, troponins, or unstable plaque indicators suggest increased near-term risk, prompting closer monitoring and preventive interventions to reduce event probability.
Take Action: Your Heart Health Journey Starts Here
The research is clear: cardiovascular biomarkers represent powerful tools for protecting your heart health. But knowledge without action changes nothing. Here's what you can do today:
Schedule a Comprehensive Cardiovascular Assessment: If you have risk factors or concerns about heart disease, talk with your doctor about comprehensive biomarker testing beyond basic cholesterol panels. Ask specifically about hs-CRP, ApoB, Lp(a), and other markers discussed in this article.
Know Your Numbers: Understand your cardiovascular biomarker values and what they mean for your personal risk profile. Keep records of serial measurements to track changes over time and treatment effectiveness.
Optimize Modifiable Risk Factors: While some biomarkers reflect genetic risk, many respond to lifestyle interventions. Regular exercise, heart-healthy nutrition, stress management, and smoking cessation positively influence inflammatory markers, metabolic biomarkers, and overall cardiovascular health.
Stay Informed: Cardiovascular biomarker research continues advancing rapidly. The studies reviewed here represent cutting-edge science from 2025, but new discoveries emerge constantly. Ask your healthcare provider about relevant new biomarkers and testing technologies.
Advocate for Precision Medicine: Discuss personalized treatment strategies based on your biomarker profile with your cardiologist. The future of cardiovascular care is individualized, and you deserve treatments optimized for your unique biochemical and genetic characteristics.
Author’s Note
As a physician and researcher, my goal in writing this article is to bridge the gap between rapidly evolving cardiovascular science and everyday clinical practice. Advances in biomarker technology are reshaping how we detect, monitor, and prevent heart disease—yet many patients and even clinicians remain unaware of their full potential. By summarizing the latest 2025 research in a clear and accessible way, I hope to empower readers with knowledge that can lead to earlier diagnosis, more precise risk assessment, and truly personalized treatment strategies.
Cardiovascular disease remains the leading global cause of death, but it is also one of the most preventable. Understanding biomarkers such as ApoB, hs-CRP, microRNAs, and high-sensitivity troponins allows us to look deeper than traditional cholesterol tests and uncover hidden risks long before symptoms appear. My intention is not to replace medical consultation but to encourage informed discussions between patients and healthcare providers.
If this article helps even one reader take proactive steps toward better heart health, then its purpose has been fulfilled.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Individual circumstances vary, and treatment decisions should always be made in consultation with qualified healthcare professionals.
Related Articles
Is Your Heart at Risk? How the TG/HDL Ratio Can Warn You Early | DR T S DIDWAL
The Metabolic Triad: Why Diabetes, Obesity & CVD Are One Epidemic | DR T S DIDWAL
What’s New in the 2025 Blood Pressure Guidelines? A Complete Scientific Breakdown | DR T S DIDWAL
References
Kishimoto, S., & Higashi, Y. (2026). Recent advances and emerging perspectives in vascular and cardiovascular research: A 2025 update. Hypertension Research. https://doi.org/10.1038/s41440-025-02540-1
Koo, T. H., Leong, X. B., & Mohamed, M. (2025). Systematic review of advanced inflammatory markers as predictors of cardiovascular diseases. Research in Cardiovascular Medicine, 14(1), 8–14. https://doi.org/10.4103/rcm.rcm_35_24
Morze, J., Melloni, G. E. M., Wittenbecher, C., Ala-Korpela, M., Rynkiewicz, A., Guasch-Ferré, M., Ruff, C. T., Hu, F. B., Sabatine, M. S., & Marston, N. A. (2025). ApoB-containing lipoproteins: count, type, size, and risk of coronary artery disease. European Heart Journal, 46(27), 2691–2701. https://doi.org/10.1093/eurheartj/ehaf207
Nazir, A., Nazir, A., Afzaal, U., Aman, S., Sadiq, S. U. R., Akah, O. Z., Jamal, M. S. W., & Hassan, S. Z. (2025). Advancements in biomarkers for early detection and risk stratification of cardiovascular diseases—A literature review. Health Science Reports, 8(5), e70878. https://doi.org/10.1002/hsr2.70878
Netala, V. R., Hou, T., Wang, Y., Zhang, Z., & Teertam, S. K. (2025). Cardiovascular biomarkers: Tools for precision diagnosis and prognosis. International Journal of Molecular Sciences, 26(7), 3218. https://doi.org/10.3390/ijms26073218
Rai, V. (2025). Current and future role of biomarkers in the monitoring and prognosis of coronary artery disease. Future Cardiology, 21(6), 331–333. https://doi.org/10.1080/14796678.2025.2477947