Forget BMI: Metabolic Health Is the Real Key to Heart Disease Risk
Is weight the only factor in heart disease? Discover why recent 2025 research suggests glucose tolerance and fat distribution are the real keys to cardiovascular protection.
HEARTMETABOLISM
Dr. T.S. Didwal, M.D.(Internal Medicine)
1/16/202610 min read
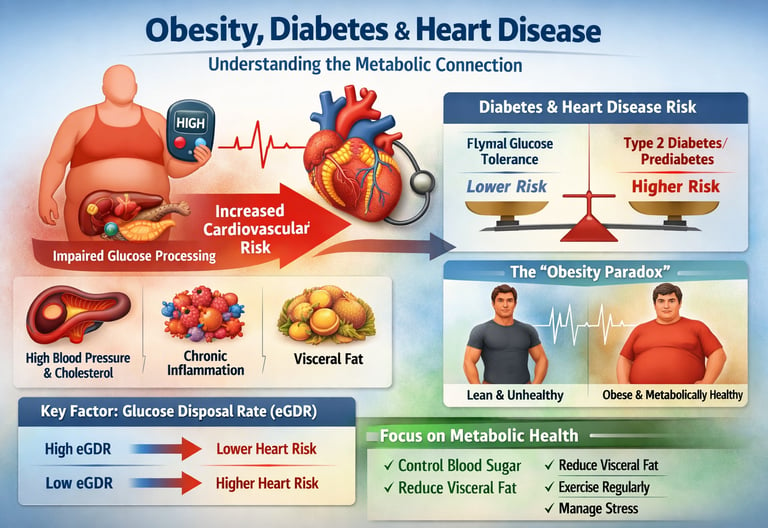
Heart disease, diabetes, and obesity are often treated as separate health problems—but emerging research reveals they are deeply interconnected parts of a single metabolic crisis. Modern studies show that disorders like insulin resistance, impaired glucose tolerance, and visceral fat accumulation do not simply coexist; they amplify each other, dramatically increasing cardiovascular disease risk even before diabetes is diagnosed (Wang et al., 2022). In fact, new data suggest that the way your body processes glucose may be more important for heart health than your actual body weight.
Recent 2024–2025 research highlights a surprising reality: two people with the same BMI can have completely different cardiovascular outcomes depending on their metabolic status. Individuals with obesity but normal glucose tolerance show far lower rates of heart disease than obese individuals with prediabetes or type 2 diabetes, challenging the long-held belief that weight alone determines risk (Asgari et al., 2024). Even more intriguing, estimated glucose disposal rate—a measure of how efficiently your body clears sugar from the bloodstream—appears to predict cardiovascular events better than traditional markers like cholesterol or blood pressure (Liao et al., 2025).
These findings point to a powerful conclusion: metabolic health—not weight alone—drives cardiovascular risk. Understanding your glucose tolerance and insulin sensitivity may be the key to protecting your heart.
CLINICAL PEARLS
1. Prioritize Metabolic Function Over the Scale
Clinical data increasingly supports the "Metabolically Healthy Obese" (MHO) concept as a transient but vital distinction. While weight is a factor, your glucose tolerance status (how your body handles sugar) is a more accurate predictor of heart disease than your Body Mass Index (BMI). In short: a leaner person with poorly managed blood sugar may actually face higher cardiovascular risks than a heavier person with perfect metabolic markers.
2. Abdominal Fat is an "Active" Organ, Not Just Storage
Research emphasizes that visceral fat—the fat deep inside your abdomen—acts like an endocrine organ.1 It releases pro-inflammatory cytokines that directly irritate the lining of your blood vessels. Measuring your waist-to-hip ratio often provides a more "heart-honest" assessment than total body weight, as it specifically tracks this inflammatory tissue.
3. Glucose Disposal Rate: Your Heart’s "Efficiency Metric"
Emerging research highlights the estimated Glucose Disposal Rate (eGDR) as a crucial new metric.2 Think of this as your body's "cleanup efficiency." The faster and more effectively your muscles and tissues can pull glucose out of your bloodstream, the less damage occurs to your arterial walls. High eGDR is essentially a "protective shield" for your cardiovascular system.3
4. Beware the "Obesity Paradox" in Treatment
The "Obesity Paradox" suggests that some obese patients with diabetes have better heart outcomes than thinner patients.4 Scientifically, this is often attributed to the protective effects of aggressive medical management and the fact that "lean" diabetes can sometimes represent a more aggressive form of the disease (where the body fails to produce enough insulin). If you are overweight, don't be discouraged; your proactive management can effectively "offset" much of the risk traditionally associated with your weight.
5. Resistance Training is "Metabolic Medicine"
Since skeletal muscle is the primary site for glucose disposal, building muscle mass is one of the most direct ways to improve insulin sensitivity.5 By increasing the "sink" where sugar can be stored, you reduce the circulating glucose that causes vascular inflammation. Even without weight loss, increasing muscle quality significantly lowers your cardiovascular risk profile
The Metabolic Connection: How Your Body's Sugar Processing Affects Your Heart
What Is Insulin Resistance, and Why Should You Care?
Your body's ability to process blood glucose—called glucose tolerance—is fundamental to cardiovascular health. Insulin resistance occurs when your body becomes less responsive to insulin, the hormone that helps cells absorb glucose. Think of it like cells developing selective hearing: they're not listening to insulin's messages as effectively anymore.
According to Wang and colleagues' groundbreaking 2022 study published in Diabetes Care, the relationship between insulin resistance and cardiovascular disease risk isn't straightforward—it depends significantly on your glucose tolerance status. This nationwide prospective cohort study tracked thousands of individuals over time, revealing that insulin resistance's impact on heart disease risk varies dramatically depending on whether someone has normal glucose tolerance, prediabetes, or type 2 diabetes.
Key Takeaway: The danger level of insulin resistance changes depending on your overall glucose management. Someone with prediabetes and insulin resistance faces different cardiovascular risks than someone with type 2 diabetes and the same insulin resistance levels.
Glucose Disposal Rate: A Predictor You Might Not Know About
More recent research from 2025 introduces an important metric called estimated glucose disposal rate (eGDR). Liao and colleagues examined the association between glucose disposal rate and cardiovascular diseases in patients with diabetes or prediabetes, revealing that how efficiently your body clears glucose from your bloodstream is a powerful predictor of heart disease risk.
When your body efficiently removes glucose from your blood—high glucose disposal rate—your heart stays healthier. Conversely, poor glucose disposal is an independent risk factor for cardiovascular complications, separate from traditional markers like cholesterol or blood pressure.
Key Takeaway: Your doctor might soon be measuring glucose disposal rate alongside other cardiovascular risk factors. This metric captures something important that standard tests might miss.
The Obesity Paradox: Why Weight Isn't the Whole Story
Beyond Body Weight: Understanding the Complexity
Here's where things get really interesting. For decades, we've operated under a simple assumption: obesity increases cardiovascular risk. While that's generally true, the reality is more nuanced. Recent research has uncovered what experts call the obesity paradox—the observation that some obese individuals show surprising resistance to cardiovascular disease, while some leaner individuals develop heart disease readily.
The 15-Year Follow-Up Study on Obesity and Glucose Status
Asgari and colleagues conducted a comprehensive pooled cohort analysis examining how obesity impacts cardiovascular outcomes differently depending on glucose tolerance status over 15 years of follow-up. Their research, published in 2024, reveals a critical insight: the cardiovascular danger of obesity isn't universal—it's amplified in people with impaired glucose tolerance or type 2 diabetes.
Individuals who are obese but maintain normal glucose tolerance show significantly lower cardiovascular risk compared to obese individuals with prediabetes or type 2 diabetes. This suggests that what happens metabolically matters more than the number on the scale.
Key Takeaway: Two people of identical weight and body composition may face vastly different cardiovascular risks depending on their metabolic health and glucose tolerance. Metabolic function matters as much as body weight.
Obesity Indices and Cardiovascular Risk Factors in Type 2 Diabetes
Mahesh et al.( 2025 ) assessed various obesity indices—including BMI, waist circumference, and body fat distribution—alongside cardiovascular risk factors in people with type 2 diabetes mellitus. Their findings highlight that traditional measures of obesity don't capture the full picture of cardiovascular danger.
Body fat distribution (where you carry weight) proved more predictive of cardiovascular risk than total weight alone. Central abdominal obesity—carrying excess weight around the midsection—showed stronger associations with cardiovascular risk factors like high blood pressure and abnormal cholesterol than overall body weight.
Key Takeaway: Where you carry extra weight matters more for heart health than how much weight you carry. Abdominal fat is more metabolically dangerous than fat stored elsewhere.
The Modern Perspective: The Obesity Paradox in Diabetes
The most recent research from Thakker et al. (2025) in the journal Current Diabetes Reports directly addresses the obesity paradox in patients with diabetes mellitus. Their comprehensive review reveals that some obese diabetic patients experience better cardiovascular outcomes than their leaner counterparts—a phenomenon that challenges our conventional understanding.
This paradox appears strongest in people receiving appropriate medical treatment for diabetes, particularly those on certain medications that may have protective effects. The implication? Successfully managing your glucose metabolism and insulin sensitivity might partially offset the cardiovascular dangers of excess weight.
Key Takeaway: The relationship between obesity and heart disease in diabetes is complex. Metabolic control and treatment quality can significantly influence cardiovascular outcomes independent of weight.
Beyond Body Mass: Comprehensive Obesity and Cardiovascular Health
A Holistic Framework for Understanding Cardiovascular Risk
Welsh et al. (2024 ) provide a comprehensive framework for understanding how obesity affects cardiovascular health. Their review emphasizes that cardiovascular risk in obese individuals stems from multiple pathways: insulin resistance, systemic inflammation, altered lipid metabolism, and increased blood pressure.
The authors stress that obesity is best understood not as a simple cosmetic or weight issue, but as a complex metabolic disorder affecting multiple organ systems, particularly the heart and blood vessels. Visceral fat—the dangerous fat surrounding internal organs—acts almost like an endocrine organ, releasing inflammatory molecules that directly damage cardiovascular tissue.
Key Takeaway: Obesity affects your cardiovascular system through multiple biological pathways. Reducing cardiovascular risk requires addressing these underlying mechanisms, not just reducing weight.
What Do These Studies Mean for You? Practical Applications
Getting Your Glucose Tolerance Tested
If you're concerned about cardiovascular health, ask your doctor about:
Fasting glucose levels
Hemoglobin A1C (measures average blood sugar over 3 months)
Oral glucose tolerance test (OGTT) to assess how your body handles glucose
Estimated glucose disposal rate (eGDR) if available
These tests provide a more complete picture than weight alone.
Assessing Your Metabolic Risk Beyond the Scale
Check with your healthcare provider about measuring:
Waist circumference (abdominal fat distribution)
Triglyceride-to-HDL ratio (reflects insulin resistance)
Blood pressure
Inflammatory markers like C-reactive protein
Making Lifestyle Changes That Address Root Causes
The research consistently shows that improving glucose tolerance and insulin sensitivity provides cardiovascular protection regardless of weight changes. Effective strategies include:
Regular physical activity (especially resistance training and aerobic exercise)
Dietary improvements focusing on whole foods, fiber, and reduced processed sugars
Weight management as part of overall metabolic health (not the sole focus)
Stress management and adequate sleep (both affect glucose metabolism)
Medical management if recommended (certain diabetes medications have cardiovascular protective effects)
Frequently Asked Questions About Obesity, Diabetes, and Heart Disease
Q: Can you be obese but metabolically healthy?
A: The research suggests it's possible but increasingly rare. Most obese individuals show some degree of insulin resistance and metabolic dysfunction. However, obese people with well-controlled blood glucose and good metabolic health do show lower cardiovascular risk than those with impaired glucose tolerance. The key is demonstrating good glucose tolerance despite excess weight.
Q: Is weight loss always necessary for cardiovascular protection?
A: While weight loss is generally beneficial, the research shows that improving glucose metabolism and insulin sensitivity provides cardiovascular protection even without dramatic weight loss. Small improvements in metabolic function can significantly reduce cardiovascular risk. That said, weight loss amplifies these benefits.
Q: Why do some overweight people have heart disease while some obese people don't?
A: The obesity paradox reflects the fact that metabolic health (particularly glucose tolerance and insulin sensitivity) matters as much as weight. People who maintain good glucose control despite excess weight face lower risk. Additionally, individual variations in visceral fat distribution, genetics, physical fitness, and medical treatment significantly influence outcomes.
Q: How important is where I carry excess weight?
A: Very important. Research shows central obesity (excess weight around the abdomen) is more dangerous for cardiovascular health than weight carried in other areas. Visceral fat is metabolically more harmful because it releases inflammatory molecules directly affecting your cardiovascular system.
Q: Can medication help reduce cardiovascular risk in obese diabetic patients?
A: Yes. Certain diabetes medications—particularly newer classes—have demonstrated cardiovascular protective effects. Some appear to partially mitigate the cardiovascular dangers of obesity in people with type 2 diabetes. Discuss these options with your healthcare provider.
Q: What's more important: losing weight or improving glucose control?
A: Both matter, but the research suggests improving glucose tolerance and insulin sensitivity might be slightly more protective for your heart. Ideally, you'd achieve both through lifestyle changes and, if necessary, medication.
Key Takeaways: What You Need to Know
Glucose Tolerance Determines Risk: The same degree of obesity or insulin resistance poses different cardiovascular risks depending on your glucose tolerance status. Someone with prediabetes faces higher risk than someone with normal glucose tolerance.
Metabolic Health Trumps Weight: Your body's ability to process glucose and maintain insulin sensitivity may be more important for heart health than your absolute weight.
Location of Fat Matters: Central obesity and visceral fat are more dangerous than fat stored elsewhere, regardless of total body weight.
Glucose Disposal Rate Is Predictive: How efficiently your body clears glucose from your bloodstream is a powerful predictor of cardiovascular risk—sometimes better than traditional measures.
The Obesity Paradox Is Real: Some obese individuals with good metabolic control show better cardiovascular outcomes than expected, highlighting the importance of metabolic function over weight alone.
Multiple Pathways to Protection: Reducing cardiovascular risk requires addressing insulin resistance, inflammation, lipid abnormalities, and blood pressure—not just weight loss.
Individual Variation Is Significant: Genetics, body fat distribution, physical fitness, medication use, and metabolic control all influence how obesity affects your specific cardiovascular risk.
Author’s Note
As a physician and medical educator, my goal in writing this article is to bridge the gap between complex metabolic science and practical, real-world health decisions. Cardiovascular disease, diabetes, and obesity are often discussed in isolation, yet the latest research clearly shows they are deeply interconnected through shared metabolic pathways. Understanding these connections empowers clinicians, patients, and health learners to move beyond outdated assumptions—such as relying solely on body weight or BMI—and instead focus on metabolic health markers that more accurately reflect cardiovascular risk.
The studies referenced in this article highlight an important paradigm shift: glucose tolerance, insulin sensitivity, and visceral fat distribution are stronger predictors of long-term cardiovascular outcomes than weight alone. This means that meaningful improvements in heart health are achievable through targeted metabolic interventions, even without dramatic weight loss.
I hope this article encourages readers to assess their health holistically, ask better questions during clinical consultations, and pursue evidence-based strategies that strengthen both metabolic and cardiovascular resilience. As new research continues to refine our understanding, my commitment remains the same—to translate emerging science into clear, actionable guidance that supports long-term health and disease prevention.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Individual circumstances vary, and treatment decisions should always be made in consultation with qualified healthcare professionals.
Related Articles
Managing Diabesity: A Complete Guide to Weight Loss and Blood Sugar Control | DR T S DIDWAL
The BMI Paradox: Why "Normal Weight" People Still Get High Blood Pressure | DR T S DIDWAL
Breakthrough Research: Leptin Reduction is Required for Sustained Weight Loss | DR T S DIDWAL
The Metabolic Triad: Why Diabetes, Obesity & CVD Are One Epidemic | DR T S DIDWAL
Obesity 2025: Revolutionary Research Advances in Treatment and Management | DR T S DIDWAL
References
Asgari, S., Molavizadeh, D., Soltani, K., Khalili, D., Azizi, F., & Hadaegh, F. (2024). The impact of obesity on different glucose tolerance status with incident cardiovascular disease and mortality events over 15 years of follow-up: A pooled cohort analysis. Diabetology & Metabolic Syndrome, 16(27). https://doi.org/10.1186/s13098-023-01253-0
Liao, J., Wang, L., Duan, L., et al. (2025). Association between estimated glucose disposal rate and cardiovascular diseases in patients with diabetes or prediabetes: a cross-sectional study. Cardiovascular Diabetology, 24, 13. https://doi.org/10.1186/s12933-024-02570-y
Mahesh, D., Kumar, G., Gupta, A. K., Singh, V. K., & Singh, V. D. (2025). Assessment of obesity indices and cardiovascular risk factors in type 2 diabetes mellitus: A pilot study from a tertiary care centre in India. Research Journal of Pharmacy and Technology, 18(2), 878–884. https://doi.org/10.52711/0974-360X.2025.00129
Thakker, J., Khaliq, I., Ardeshna, N. S., et al. (2025). The obesity paradox of cardiovascular outcomes in patients with diabetes mellitus. Current Diabetes Reports, 25, 35. https://doi.org/10.1007/s11892-025-01592-4
Wang, T., Li, M., Zeng, T., Hu, R., Xu, Y., Xu, M., Zhao, Z., Chen, Y., Wang, S., Lin, H., Yu, X., Chen, G., Su, Q., Mu, Y., Chen, L., Tang, X., Yan, L., Qin, G., Wan, Q., Gao, Z., & Lu, J. (2022). Association between insulin resistance and cardiovascular disease risk varies according to glucose tolerance status: A nationwide prospective cohort study. Diabetes Care, 45(8), 1863–1872. https://doi.org/10.2337/dc22-0202
Welsh, A., Hammad, M., & Piña, I. L. (2024). Obesity and cardiovascular health. European Journal of Preventive Cardiology, 31(8), 1026–1035. https://doi.org/10.1093/eurjpc/zwae025