Reversing Heart Age: What New Research Reveals About Arterial Stiffness
Explore recent research on arterial stiffness, vascular aging, and how lifestyle and cardiometabolic risk management improve arterial flexibility.
HEART
Dr. T.S. Didwal, M.D.(Internal Medicine)
1/27/202612 min read
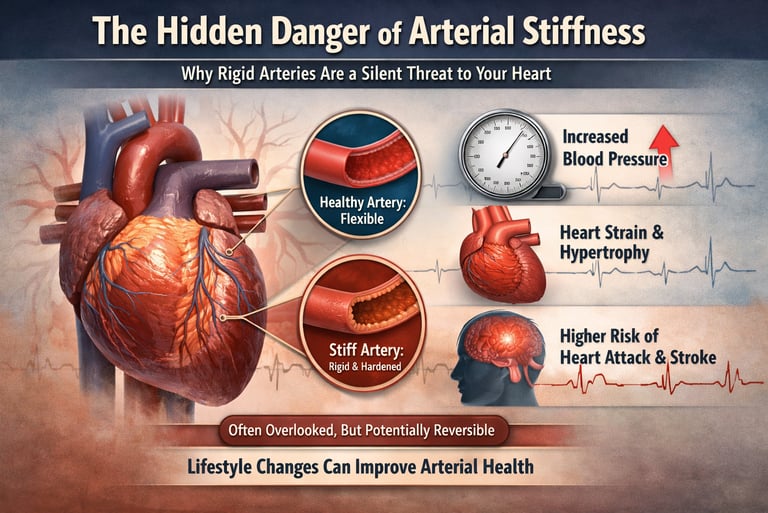
Heart disease rarely begins with a sudden blockage or dramatic symptoms—it often starts silently, years earlier, within the walls of the arteries themselves. Long before cholesterol plaques rupture or blood pressure spirals out of control, arteries may lose one of their most vital properties: flexibility. This gradual loss of arterial elasticity, known as arterial stiffness, is now recognized as a powerful and independent predictor of cardiovascular morbidity and mortality, rivaling traditional risk factors such as hypertension and dyslipidemia (Xuereb et al., 2023).
Healthy arteries expand and recoil with each heartbeat, buffering pressure fluctuations and protecting the heart from excessive workload. When this elastic function deteriorates, pressure waves travel faster and reflect prematurely toward the heart, elevating central systolic pressure and increasing myocardial stress—a process central to the development of left ventricular hypertrophy, heart failure, and stroke (Kim, 2025). Importantly, arterial stiffness does not merely accompany cardiometabolic disease; mounting evidence suggests it actively accelerates vascular aging and disease progression in individuals with obesity, type 2 diabetes, and metabolic syndrome (De la Maza-Bustindui et al., 2025).
What makes arterial stiffness particularly concerning is its stealth. Many individuals with “controlled” blood pressure or acceptable lipid levels may already have significantly stiffened arteries, placing them at elevated cardiovascular risk that standard assessments fail to detect. Fortunately, emerging research offers a hopeful counterpoint: arterial stiffness is not always permanent. Lifestyle interventions—especially structured exercise—along with aggressive management of cardiometabolic risk factors, have demonstrated measurable improvements in arterial compliance within months (Wu et al., 2025). As scientific understanding evolves, arterial stiffness is shifting from an overlooked consequence of aging to a modifiable therapeutic target, redefining how cardiovascular risk is identified and managed in modern medicine.
Clinical pearls
1. The Hemodynamic "Shock Absorber"
Arteries function as a Windkessel (pressure reservoir), converting the heart's intermittent pulsatile output into continuous peripheral flow. Arterial stiffness increases Pulse Wave Velocity (PWV), causing pressure waves to reflect back too quickly, which elevates Central Systolic Blood Pressure and increases left ventricular afterload.
Think of your arteries as your heart’s "shock absorbers." Healthy arteries are bouncy and soak up the pressure of every heartbeat. When they stiffen, they act like a brick wall; the pressure bounces right back at your heart, forcing it to work twice as hard and causing internal wear and tear.
2. The Multi-Factor Synergy (The 1+1=3 Rule)
The reversibility of arterial compliance is non-linear and dependent on the simultaneous mitigation of multiple cardiometabolic hits. Managing dyslipidemia (lipids) or hyperglycemia (glucose) in isolation yields inferior results compared to a comprehensive "bundle" approach that addresses oxidative stress and low-grade systemic inflammation together.
You can’t fix a "stiff heart" by only fixing one problem. Improving your cholesterol is great, but your arteries won't regain their flexibility unless you tackle blood sugar and weight at the same time. It’s like a four-legged stool—if you only fix one leg, the seat is still shaky. Success comes from the "combo pack" of healthy habits.
3. Endothelial "Shear Stress" & HIIT
High-Intensity Interval Training (HIIT) induces superior improvements in Endothelial Function compared to moderate-intensity exercise. The rapid fluctuations in blood flow create "shear stress" against the vessel walls, triggering the release of Nitric Oxide, a potent vasodilator that helps remodel the arterial matrix and reduce stiffness.
Short bursts of faster movement (HIIT) act like a "workout" for the inside lining of your blood vessels. This "rhythmic stretching" tells your body to release natural chemicals that relax and widen your pipes. While a steady walk is good, giving your heart a "high-intensity nudge" for just a minute at a time is what actually helps "re-train" your arteries to stay flexible.
4. Metabolic "Caramelization" (AGEs)
Chronic hyperglycemia promotes the formation of Advanced Glycation End products (AGEs), which create covalent cross-links between collagen fibers in the arterial wall. This "cross-linking" creates a rigid extracellular matrix that is mechanically resistant to expansion, independent of blood pressure levels.
High blood sugar literally "caramelizes" your arteries. Just like sugar turns brittle and sticky when heated, excess sugar in your blood coats the proteins in your vessel walls, making them "crunchy" and stiff instead of soft and stretchy. Controlling your sugar isn't just about diabetes; it's about keeping your internal "rubber bands" from snapping.
5. The Window of Reversibility
Arterial remodeling is a dynamic process. While advanced structural calcification is difficult to undo, early-stage stiffness driven by functional impairment (smooth muscle tone and endothelial dysfunction) is highly plastic. Recent data suggests significant improvements in Augmentation Index (AIx) can be captured within a 12-week clinical window.
Your heart’s flexibility isn't "gone for good." There is a window of opportunity where you can actually reverse the damage before it turns into permanent scarring. The latest research shows that if you start a focused plan today, your body can begin "softening" your arteries and improving your blood flow markers in about 90 days.
Arterial Stiffness and Cardiovascular Health: What Recent Research Reveals About Your Heart's Flexibility
What Is Arterial Stiffness? Breaking Down the Science
Arterial stiffness refers to the reduced elasticity of arteries, where blood vessels lose their ability to expand and contract smoothly in response to blood pressure changes. Think of it like a rubber hose that hardens over time—it no longer flexes as intended, compromising function.
This condition significantly impacts pulsatile hemodynamics, which describes how blood pressure waves travel through your circulatory system. When arteries stiffen, these pressure waves don't dissipate smoothly, leading to elevated central blood pressure and increased strain on the heart.
Key risk factors for arterial stiffness include:
Advanced age
Hypertension (high blood pressure)
Type 2 diabetes
Dyslipidemia (abnormal cholesterol levels)
Obesity
Smoking
Chronic inflammation
Sedentary lifestyle
Study 1: Arterial Stiffness and Pulsatile Hemodynamics in Cardiometabolic Disorders
Kim's 2025 research published in CardioMetabolic Syndrome Journal provides critical insights into the relationship between arterial stiffness and pulsatile hemodynamics in patients with cardiometabolic disorders. This study demonstrates that stiffened arteries directly compromise the body's ability to manage blood pressure fluctuations effectively.
The research emphasizes that arterial stiffness acts as both a marker and a mediator of cardiovascular disease in individuals with metabolic syndrome, insulin resistance, and obesity. The study found that abnormal hemodynamic patterns resulting from stiff arteries increase the workload on the left ventricle of the heart, potentially leading to left ventricular hypertrophy (thickening of the heart muscle).
Critical insight: Patients with cardiometabolic disorders show accelerated arterial stiffening, making this population especially vulnerable to sudden cardiovascular events and heart failure. Early detection and intervention targeting arterial function could prevent progression to severe cardiovascular disease.
If you have metabolic syndrome, prediabetes, or obesity, your arteries may already be showing signs of stiffening. This research suggests that monitoring arterial stiffness biomarkers through clinical assessments could help identify your cardiovascular risk earlier than traditional methods.
Study 2: Impact of Cardiometabolic Risk Factors and Management on Arterial Stiffness Reversal
De la Maza-Bustindui and colleagues (2025) published groundbreaking research in npj Cardiovascular Health examining whether arterial stiffness can actually be reversed through proper management of cardiometabolic risk factors. This is perhaps the most hopeful finding in recent research—suggesting that damage to your arteries may not be permanent.
The study demonstrates that aggressive management of blood pressure, glucose control, lipid profiles, and body weight can halt the progression and potentially reverse arterial stiffness in patients with established cardiometabolic disease. The research found that patients who achieved optimal control of multiple risk factors showed measurable improvements in arterial compliance and elastic modulus (measures of arterial flexibility).
Major discovery: The reversibility of arterial stiffness wasn't uniform across all patients—those who made comprehensive lifestyle changes combined with appropriate medical therapy showed the most dramatic improvements.
This research provides powerful motivation: your current trajectory toward arterial stiffening isn't inevitable. By addressing multiple cardiometabolic risk factors simultaneously—not just one or two—you can potentially restore elasticity to your arteries. This suggests that comprehensive programs addressing weight management, blood pressure control, diabetes management, and cholesterol reduction offer the best hope for improvement.
Study 3: Comparative Effectiveness of Exercise Interventions on Arterial Stiffness
Wu and team (2025) conducted a systematic review and network meta-analysis in Frontiers in Cardiovascular Medicine, analyzing the comparative effectiveness of various exercise interventions for reducing arterial stiffness in individuals at cardiovascular risk. This comprehensive analysis synthesized evidence from multiple studies to identify which types of physical activity work best.
The meta-analysis revealed that aerobic exercise, resistance training, and combined exercise programs all reduce arterial stiffness, but they're not equally effective. Key findings include:
High-intensity interval training (HIIT) showed particularly promising results for reducing arterial stiffness and improving endothelial function (the health of the inner lining of arteries)
Sustained aerobic exercise (like brisk walking or jogging) provided consistent, measurable improvements in arterial compliance
Resistance training alone was less effective than aerobic approaches, but valuable when combined with cardiovascular exercise
Exercise duration and intensity matter—more substantial improvements occurred with 150+ minutes weekly of moderate-intensity activity or equivalent high-intensity work
Important nuance: The effectiveness of exercise depended significantly on baseline fitness level, age, and disease severity. Individuals with severe arterial stiffness needed longer intervention periods to see measurable improvements.
If you're asking, "Will exercise really help my stiffened arteries?" this research answers yes—but with caveats. Regular, consistent aerobic exercise, especially including higher-intensity intervals, appears most effective. However, you don't need to become an athlete; the research supports benefits from walking and moderate activity when sustained consistently.
Study 4: Mapping Arterial Stiffness Metabolic Biomarkers—A Bibliometric Analysis
Chen et al.(2025) conducted a comprehensive bibliometric analysis in Frontiers in Medicine, mapping research trends and identifying key metabolic biomarkers associated with arterial stiffness. This analysis surveyed the entire landscape of arterial stiffness research to identify emerging patterns and promising biomarkers.
The bibliometric analysis identified several metabolic biomarkers strongly associated with arterial stiffness, including:
Advanced glycation end products (AGEs): Compounds formed when blood glucose remains elevated, directly damaging arterial walls
Inflammatory markers (C-reactive protein, interleukin-6): Chronic inflammation accelerates arterial stiffening
Oxidative stress markers: Free radicals damage the cells maintaining arterial elasticity
Lipid peroxidation products: Abnormal cholesterol oxidation contributes to arterial dysfunction
Endothelial dysfunction markers: Impaired function of the arterial lining predicts stiffening progression
The analysis revealed that research increasingly recognizes arterial stiffness as a multifactorial condition involving interconnected metabolic, inflammatory, and oxidative pathways rather than a single cause.
Understanding these biomarkers helps explain why managing multiple cardiometabolic risk factors matters more than controlling any single factor. If you have elevated blood glucose, inflammation, or oxidative stress, addressing all three simultaneously produces better results than focusing on one alone. Some of these biomarkers may become part of routine clinical assessment to identify who truly needs intervention.
Study 5: Arterial Stiffness and Its Impact on Cardiovascular Health
Xuereb, Magri, and Xuereb's 2023 research in Current Cardiology Reports synthesized evidence on how arterial stiffness affects overall cardiovascular health across the lifespan. This comprehensive review highlights arterial stiffness as a critical link between aging, chronic disease, and heart disease risk.
This review establishes arterial stiffness as a fundamental mechanism connecting multiple cardiovascular risk factors. Key conclusions include:
Arterial stiffness is both a cause and consequence of cardiovascular disease—it develops from disease processes but also accelerates their progression
Age-related arterial stiffening is partly inevitable but accelerated by cardiometabolic risk factors
Measurement of arterial stiffness using indices like pulse wave velocity (PWV) and augmentation index (AIx) provides independent prognostic information beyond traditional risk factors
Early intervention targeting arterial function may prevent or delay progression to overt cardiovascular disease
This research positions arterial stiffness not as a minor detail but as a central feature of cardiovascular health. It suggests that traditional risk assessment—looking only at cholesterol, blood pressure, and diabetes—may miss crucial information. Your arteries' actual mechanical function matters for predicting outcomes.
The Interconnected Picture: How These Studies Work Together
These five studies collectively paint a comprehensive picture of arterial stiffness in modern cardiovascular medicine:
From cause to consequence: Research shows that cardiometabolic risk factors like obesity, diabetes, and hypertension cause arterial stiffening through multiple pathways involving metabolic dysfunction, inflammation, and oxidative stress. Once present, stiffened arteries worsen these same conditions, creating a vicious cycle.
From problem to solution: The most encouraging finding across these studies is that the cycle can be interrupted. Exercise interventions combined with management of cardiometabolic risk factors can measurably improve arterial compliance and potentially reverse early-stage arterial stiffness.
From research to clinical practice: Growing recognition of specific metabolic biomarkers suggests that future clinical practice will increasingly use targeted biomarker assessment to guide personalized intervention strategies for arterial stiffness.
Practical Implications: What Should You Do?
Assessment
If you have cardiovascular risk factors, discuss with your healthcare provider whether assessment of arterial stiffness through measurement of pulse wave velocity (PWV) or augmentation index (AIx) would provide valuable information about your specific risk.
Lifestyle Interventions
Based on this research, comprehensive lifestyle change offers the most promise:
Exercise: Aim for 150+ minutes weekly of moderate-intensity aerobic activity or equivalent high-intensity exercise. Consider including intervals of higher-intensity work when safe for your fitness level.
Weight management: Even modest weight loss (5-10% of body weight) can improve arterial stiffness, particularly in individuals with obesity or metabolic syndrome.
Blood pressure control: Target blood pressure less than 130/80 mmHg if tolerated. Better blood pressure control directly improves arterial compliance.
Glucose management: Whether through weight loss, physical activity, or medications, achieving target blood glucose levels and HbA1c (a measure of average blood sugar over three months) reduces arterial stiffening.
Cholesterol management: Maintain healthy lipid profiles through diet, exercise, and medications if needed.
Medical Management
Work with your healthcare provider to optimize medications for managing hypertension, diabetes, dyslipidemia, and other cardiovascular risk factors. The research suggests that aggressive management of all modifiable risk factors produces better results than partial control.
Frequently Asked Questions About Arterial Stiffness
Q: Is arterial stiffness reversible?
A: Yes, according to 2025 research by De la Maza-Bustindui and colleagues. Early-stage arterial stiffness can be reversed through comprehensive management of cardiometabolic risk factors. However, reversal requires attention to multiple factors simultaneously—blood pressure, weight, glucose control, and cholesterol—not just one or two. Advanced arterial stiffness may be harder to reverse completely, though improvement is still possible.
Q: How is arterial stiffness measured?
A: The gold standard measurement is pulse wave velocity (PWV), which measures how fast blood pressure waves travel through arteries. Another common measure is the augmentation index (AIx), which reflects how much pressure waves bounce back from small arteries. Non-invasive techniques like applanation tonometry can assess these measures in clinical settings.
Q: How common is arterial stiffness?
A: Very common, particularly in individuals over age 50 and in those with cardiovascular risk factors. Many people with hypertension, diabetes, or obesity have measurable arterial stiffness without knowing it.
Q: Can young people develop arterial stiffness?
A: Yes. While aging increases risk, aggressive cardiometabolic risk factors—particularly diabetes, severe obesity, or sustained hypertension—can cause arterial stiffness at younger ages.
Q: What's the connection between arterial stiffness and heart attacks?
A: Stiffened arteries increase work on the heart, raise central blood pressure, and impair the heart's ability to respond to stress. This increases risk for heart attacks, strokes, and heart failure. Arterial stiffness also reflects underlying damage to artery walls that increases atherosclerosis (plaque buildup) risk.
Q: Do I need special tests if I have arterial stiffness?
A: Management focuses on reducing cardiometabolic risk factors rather than treating arterial stiffness directly. Standard monitoring of blood pressure, weight, blood glucose, and cholesterol is essential. Your doctor may recommend other tests based on your specific situation and cardiovascular risk profile.
Q: How long does it take to see improvements with exercise and lifestyle changes?
A: Research suggests measurable improvements in arterial function can occur within 8-12 weeks of consistent exercise and lifestyle changes, though more substantial improvements typically require 3-6 months or longer.
Key Takeaways: Essential Points to Remember
Arterial stiffness is a critical marker of cardiovascular health, reflecting damage to your arteries' elasticity from various disease processes and risk factors.
It's not inevitable or irreversible, particularly when addressed early with comprehensive lifestyle and medical intervention.
Multiple risk factors matter more than any single factor—simultaneous attention to weight, blood pressure, glucose control, and cholesterol produces better outcomes than partial approaches.
Exercise is proven effective, particularly aerobic activity including higher-intensity intervals, with benefits appearing within weeks to months.
Emerging research on metabolic biomarkers suggests future clinical practice will increasingly use targeted assessment to guide personalized treatment approaches.
Monitoring and early detection matter—discussing assessment of arterial stiffness with your healthcare provider may reveal risk you couldn't otherwise see.
Author’s Note
This article is intended to translate complex and rapidly evolving cardiovascular research into clear, clinically meaningful insights for readers seeking a deeper understanding of arterial health. Arterial stiffness is often discussed in academic circles but remains underrecognized in everyday clinical conversations, despite its strong and independent association with cardiovascular morbidity and mortality. The goal of this piece is to bridge that gap—connecting rigorous scientific evidence with practical implications that matter to patients, clinicians, and health-conscious readers alike.
The studies cited herein were selected for their methodological strength, recency, and relevance to real-world cardiometabolic health. Particular emphasis was placed on research published between 2023 and 2025 to reflect the most current understanding of arterial stiffness as both a marker and mediator of cardiovascular disease. Where possible, findings were synthesized across disciplines—including vascular physiology, exercise science, and metabolic medicine—to present an integrated view rather than isolated results.
Importantly, this article does not suggest that arterial stiffness should be viewed in isolation or managed through a single intervention. Instead, the evidence consistently points toward a comprehensive approach that addresses multiple cardiometabolic risk factors simultaneously. While lifestyle modification and medical management can meaningfully improve arterial function—especially in early stages—individual responses vary, and clinical decisions should always be personalized.
This work is educational in nature and not a substitute for professional medical advice. Readers are encouraged to discuss cardiovascular risk assessment and management strategies with qualified healthcare providers. As research continues to evolve, so too will our understanding of arterial health, offering new opportunities for earlier detection, targeted intervention, and improved cardiovascular outcomes.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Individual circumstances vary, and treatment decisions should always be made in consultation with qualified healthcare professionals.
Related Articles
hsCRP in Cardiovascular Disease: Should It Be Measured for Risk Assessment in 2026? | DR T S DIDWAL
Your Body Fat Is an Endocrine Organ—And Its Hormones Shape Your Heart Health | DR T S DIDWAL
hsCRP Explained: What Inflammation Means for Your Heart | DR T S DIDWAL
What’s New in the 2025 Blood Pressure Guidelines? A Complete Scientific Breakdown | DR T S DIDWAL
Low-Fat vs. Low-Carb: Which Diet is Best for Weight Loss? | DR T S DIDWAL
5 Steps to Reverse Metabolic Syndrome: Diet, Habit, & Lifestyle Plan | DR T S DIDWAL
The Role of Cholesterol in Health and Disease: Beyond the "Bad" Label | DR T S DIDWAL
Lowering Cholesterol with Food: 4 Phases of Dietary Dyslipidemia Treatment | DR T S DIDWAL
The Best Dietary Fat Balance for Insulin Sensitivity, Inflammation, and Longevity | DR T S DIDWAL
References
Chen, B., Wirawan, K. F., Luo, L., Zhang, J., & Li, T. (2025). Mapping arterial stiffness metabolic biomarkers: A bibliometric analysis. Frontiers in Medicine, 12, Article 1557731. https://doi.org/10.3389/fmed.2025.1557731
De la Maza-Bustindui, N. S., León-Álvarez, M., Ponce-Acosta, C., et al. (2025). Impact of cardiometabolic risk factors and its management on the reversion and progression of arterial stiffness. npj Cardiovascular Health, 2, 36. https://doi.org/10.1038/s44325-025-00074-6
Kim, H.-L. (2025). Arterial stiffness and pulsatile hemodynamics in cardiometabolic disorders. CardioMetabolic Syndrome Journal, 5(2), 60–72. https://doi.org/10.51789/cmsj.2025.5.e11
Wu, R. S., Zhang, Y., Yuan, X. W., Yan, X., & Fu, X. L. (2025). Comparative effectiveness of exercise interventions on arterial stiffness in individuals at risk for cardiovascular disease: A systematic review and network meta-analysis. Frontiers in Cardiovascular Medicine, 12, 1489382. https://doi.org/10.3389/fcvm.2025.1489382
Xuereb, R. A., Magri, C. J., & Xuereb, R. G. (2023). Arterial stiffness and its impact on cardiovascular health. Current Cardiology Reports, 25, 1337–1349. https://doi.org/10.1007/s11886-023-01951-1