hsCRP in Cardiovascular Disease: Should It Be Measured for Risk Assessment in 2026?
Explore the latest 2025–2026 research on high-sensitivity C-reactive protein (hsCRP). Learn how this inflammatory biomarker predicts plaque vulnerability and long-term cardiovascular risk beyond traditional cholesterol testing.
HEART
Dr. T.S. Didwal, M.D.(Internal Medicine)
2/1/202613 min read

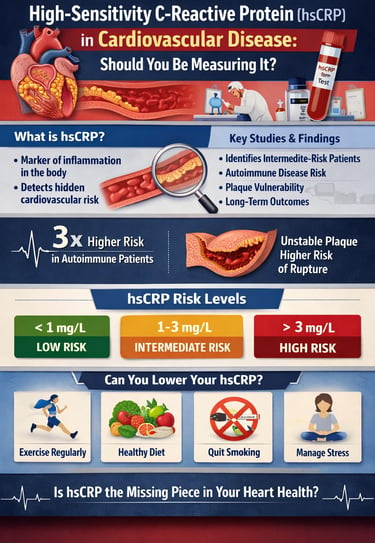
Cardiovascular disease often announces itself without warning—frequently as a first heart attack or sudden stroke in individuals who were previously considered “low risk.” Traditional risk factors such as LDL cholesterol, blood pressure, and diabetes explain much of this risk, yet they fail to capture a crucial driver of atherosclerosis: chronic vascular inflammation. Increasing evidence suggests that inflammation is not merely a bystander but an active participant in plaque formation, destabilization, and rupture. This realization has renewed interest in high-sensitivity C-reactive protein (hsCRP) as a clinically meaningful biomarker of cardiovascular risk.
Unlike standard CRP assays, hsCRP can detect low-grade inflammation long before symptoms appear, offering insight into the biological activity occurring within arterial walls. Large contemporary studies demonstrate that elevated hsCRP predicts myocardial infarction, stroke, and all-cause mortality independent of traditional risk factors—even decades before clinical events occur (Hartley et al., 2025). Imaging-based trials further reveal that hsCRP correlates with plaque vulnerability, not merely plaque burden, linking systemic inflammation to lesions most likely to rupture (Fröbert et al., 2025).
Importantly, hsCRP appears particularly valuable in populations where standard risk calculators fall short, including individuals with intermediate cardiovascular risk, patients with autoimmune inflammatory diseases, and survivors of acute coronary syndromes (Mehta et al., 2025; Shende et al., 2026). These findings challenge the notion that lipid levels alone define cardiovascular risk and support a more integrated, inflammation-aware approach to prevention.
As cardiology moves toward precision risk stratification, the key question is no longer whether inflammation matters—but whether clinicians should routinely measure it. Emerging consensus suggests that, when used selectively and thoughtfully, hsCRP may provide actionable information that reshapes preventive cardiovascular care (Hernandez Ortega et al., 2025).
Clinical pearls
1. The "Fire vs. Fuel" Concept
Scientific Insight: While LDL cholesterol acts as the "fuel" (the material that builds up in the artery wall), hsCRP represents the "fire" (the inflammatory process that makes that material unstable).
Takeaway: You can have a low amount of fuel (cholesterol), but if there is a spark of inflammation (high hsCRP), you are still at risk of a "fire" or heart attack. Both numbers matter.
2. The 10.0 mg/L "Reset" Rule
Scientific Insight: In cardiovascular risk stratification, an hsCRP value >10.0 mg/L is generally considered clinically "uninterpretable" for heart disease. It usually indicates an acute infection, injury, or flare-up of a chronic condition.
Takeaway: If your number is extremely high (over 10), don't panic about your heart immediately. You likely have a cold, a minor injury, or a recent infection. Wait two weeks and test again when you are feeling 100% healthy.
3. The "Statin" Synergist
Scientific Insight: Research (such as the JUPITER trial and recent 2025 updates) shows that statins don't just lower cholesterol; they have pleiotropic effects, meaning they directly lower hsCRP levels regardless of LDL changes.
Takeaway: If your doctor prescribes a statin despite "decent" cholesterol, it might be because your hsCRP is high. The medicine is acting as a "fire extinguisher" for the inflammation in your arteries.
4. Stability Over Quantity
Scientific Insight: As highlighted in the Fröbert et al. (2025) study, hsCRP is a marker of plaque vulnerability. A small, inflamed plaque is more likely to rupture and cause a heart attack than a large, stable, calcified one.
Takeaway: It’s not just about how much "gunk" is in your pipes; it's about how stable that gunk is. Low hsCRP is a sign that your arterial walls are stable and less likely to cause a sudden emergency.
5. The "Golden Window" for Autoimmune Patients
Scientific Insight: For patients with RA or Lupus, traditional risk calculators (like the ASCVD score) often underestimate risk. In these populations, hsCRP should be viewed as a risk enhancer that can justify earlier, more aggressive preventative therapy.
Takeaway: If you have an autoimmune condition, your "normal" risk isn't actually normal. Checking hsCRP helps your doctor see the invisible stress your condition is putting on your heart, allowing you to protect yourself sooner.
6. Lifestyle is a "Biological Modifier"
Scientific Insight: Unlike genetic risk factors, hsCRP is highly sensitive to lifestyle interventions. Aerobic exercise and the Mediterranean diet act as "biologic modifiers" that downregulate pro-inflammatory cytokines like IL-6, which in turn lowers hsCRP.
Takeaway: You are in the driver's seat. Weight loss and exercise aren't just "good ideas"—they are direct medical treatments that physically cool down the inflammation in your blood vessels.
What is High-Sensitivity C-Reactive Protein (hsCRP)?
High-sensitivity C-reactive protein is a marker of inflammation in your body, specifically measured using advanced laboratory techniques that can detect even tiny amounts of this protein. When your body experiences inflammation—whether from infection, injury, or chronic disease—your liver produces C-reactive protein (CRP) as an inflammatory response.
But here's the crucial part: chronic inflammation isn't always obvious. Unlike an acute infection that causes fever and discomfort, the type of inflammation linked to cardiovascular disease risk happens silently in your arteries. This is why hsCRP testing has gained significant attention in recent years as a potential early warning system for heart disease.
The difference between standard CRP and hsCRP lies in sensitivity. While traditional CRP tests are useful for detecting acute inflammation, hsCRP tests can measure inflammation at much lower levels, making them particularly valuable for assessing cardiovascular risk in apparently healthy individuals.
Study 1: Consensus on hsCRP Measurement
The Mehta et al. (2025) addressed one of the most pressing questions in modern cardiology: should we measure hsCRP in patients with atherosclerotic cardiovascular disease (ASCVD)?
This comprehensive review in US Cardiology examined whether adding hsCRP measurement to standard risk assessment tools actually improves our ability to predict heart attacks and strokes. The researchers found that while hsCRP does have merit as an additional risk marker, the question isn't simply "yes or no"—it's more nuanced.
The research indicates that hsCRP is most valuable in specific clinical scenarios:
For individuals with intermediate cardiovascular risk: Those whose traditional risk factors (cholesterol, blood pressure, diabetes status) don't clearly indicate high or low risk benefit most from hsCRP testing
For risk stratification: When doctors need to decide whether someone should start preventive medications like statins, hsCRP levels can provide additional clarity
For motivation: Sometimes seeing an elevated hsCRP result motivates patients to make lifestyle changes
Think of hsCRP as a detective's magnifying glass—it helps identify inflammation markers that standard tests might miss. For middle-risk patients, this additional information can be truly valuable.
Study 2: - hsCRP as a Risk Assessment Tool
Hernandez Ortega et al. (2025) published their findings in Cardiology Magazine from the American College of Cardiology, focusing specifically on hsCRP as a promising risk assessment tool. Their work highlighted emerging evidence that hsCRP measurement may help identify patients at risk for cardiovascular events who might otherwise be considered low-risk by traditional metrics.
The researchers emphasized that hsCRP levels correlate with the presence and severity of atherosclerotic plaque in arteries. This is significant because it suggests that elevated hsCRP might indicate active inflammation within artery walls—precisely where heart attacks begin.
Key Insights for Patients
Normal hsCRP level: Less than 1.0 mg/L indicates low risk
An intermediate hsCRP level: 1.0 to 3.0 mg/L suggests intermediate risk
Elevated hsCRP level: Greater than 3.0 mg/L indicates higher cardiovascular risk
The Hernandez Ortega study suggests that hsCRP measurement should be considered a "promising" tool in modern cardiology practice, particularly for patients where traditional risk assessment leaves uncertainty.
Study 3: hsCRP and Autoimmune Diseases
Shende et al. (2026) conducted a groundbreaking cross-sectional study published in the Journal of Clinical and Diagnostic Research, examining the correlation between hsCRP and fasting lipid profiles in patients with autoimmune connective tissue disorders.
This research is particularly important because patients with conditions like rheumatoid arthritis and lupus face dramatically elevated cardiovascular disease risk—often 2-3 times higher than the general population.
The study demonstrated a significant positive correlation between elevated hsCRP levels and abnormal lipid profiles in patients with autoimmune diseases. This finding suggests that:
Inflammation and lipid abnormalities work together to increase cardiovascular risk in autoimmune patients
hsCRP testing could help identify which autoimmune patients need more aggressive cardiovascular risk reduction
The combination of hsCRP and traditional lipid testing provides a more complete picture of cardiovascular health in this high-risk population
For patients with conditions like rheumatoid arthritis, systemic lupus erythematosus, or Sjögren's syndrome, monitoring hsCRP levels becomes even more critical because inflammation is a hallmark of both the autoimmune condition and cardiovascular disease progression.
Study 4: Fröbert et al. (2025) - hsCRP and Vulnerable Plaque Detection
Fröbert et al. (2025) published remarkable findings in JACC: Cardiovascular Interventions from the PROSPECT II trial, one of the most rigorous cardiovascular studies conducted. Their research examined the relationship between hsCRP and high-risk vulnerable plaque after non-ST elevation myocardial infarction (NSTEMI).
The PROSPECT II trial used advanced intravascular ultrasound (IVUS) imaging to directly visualize plaque characteristics in patients who had already suffered heart attacks. This allowed researchers to correlate hsCRP levels with the actual structure and composition of plaques.
Key Findings
Higher hsCRP levels were associated with more vulnerable plaque characteristics—meaning plaques more likely to rupture and cause heart attacks
hsCRP appears to reflect the stability of atherosclerotic lesions, not just the amount of plaque
Patients with both elevated hsCRP and vulnerable plaque features have the worst prognosis
This research validates the concept that hsCRP isn't simply measuring inflammation—it's identifying plaques at risk of rupture. For patients recovering from heart attacks, an elevated hsCRP signals the need for more intensive cardiovascular risk management, including aggressive medication therapy and lifestyle modification.
Study 5: Long-Term Cardiovascular Outcomes
Hartley et al. (2025) published findings in eBioMedicine that represent some of the most compelling evidence for hsCRP's predictive value. Their study tracked the relationship between baseline hsCRP and incident cardiovascular events over an impressive 20-year period.
What 20 Years of Data Revealed
Elevated baseline hsCRP levels were significantly associated with increased risk of cardiovascular events over 20 years
hsCRP's predictive power persisted even after accounting for traditional risk factors like blood pressure, cholesterol, and smoking status
All-cause mortality was higher in individuals with elevated hsCRP, suggesting the importance of inflammation as a broad health indicator
Unlike shorter studies that might show temporary associations, the Hartley et al. research provides evidence that hsCRP measurement offers genuine long-term prognostic value. This means that a single blood test measuring hsCRP can provide information about your cardiovascular risk over the next two decades.
Key Studies on hsCRP in Cardiovascular Disease (2025–2026)
Mehta et al. (2025)
Study focus: Rationale for hsCRP measurement in ASCVD
Key finding: hsCRP adds meaningful value in intermediate-risk patients
Clinical application: Improves risk stratification and guides preventive therapy decisions
Hernandez Ortega et al. (2025)
Study focus: hsCRP as a cardiovascular risk assessment tool
Key finding: Identifies individuals at increased cardiovascular risk who may be missed by traditional metrics
Clinical application: Supports preventive cardiology and early intervention
Shende et al. (2026)
Study focus: Role of hsCRP in autoimmune connective tissue diseases
Key finding: Significant positive correlation between hsCRP and adverse lipid profiles
Clinical application: Enhances cardiovascular screening in autoimmune patients
Fröbert et al. (2025)
Study focus: Relationship between hsCRP and plaque vulnerability after NSTEMI
Key finding: Elevated hsCRP correlates with unstable, rupture-prone plaques
Clinical application: Guides post-myocardial infarction risk management
Hartley et al. (2025)
Study focus: Long-term cardiovascular outcomes
Key finding: Baseline hsCRP predicts cardiovascular events and mortality over 20 years
Clinical application: Useful for lifetime cardiovascular risk assessment
Who Should Get Their hsCRP Tested?
Based on the research evidence, hsCRP testing is most beneficial for:
Intermediate-Risk Patients
If your traditional cardiovascular risk factors don't clearly indicate high or low risk, hsCRP measurement can help your doctor make better decisions about preventive therapy.
Patients with Autoimmune Diseases
If you have rheumatoid arthritis, lupus, or other inflammatory autoimmune conditions, your hsCRP level provides important insight into your cardiovascular risk—especially when combined with lipid testing.
Heart Attack Survivors
If you've had an NSTEMI or other acute cardiovascular event, hsCRP measurement helps identify whether your plaque is becoming more stable or remains dangerous.
People with Family History
If close relatives experienced early heart disease or stroke, hsCRP testing can help determine whether you've inherited cardiovascular risk factors and need more aggressive prevention
.
Those Considering Preventive Medications
If you're discussing whether to start medications like statins for primary prevention (before having a heart attack), an elevated hsCRP provides additional justification for treatment.
Understanding hsCRP Results: What Do Your Numbers Mean?
hsCRP is measured in mg/L:
< 1.0 mg/L: Low cardiovascular risk
1.0 to 3.0 mg/L: Intermediate cardiovascular risk
> 3.0 mg/L: High cardiovascular risk
Important Note: A single hsCRP measurement tells you one piece of your health puzzle. It should never replace comprehensive cardiovascular assessment that includes blood pressure, cholesterol levels, diabetes screening, and lifestyle factors.
Beyond the Blood Test: What Lowers hsCRP?
The beauty of hsCRP as a health marker is that it's modifiable. Here are evidence-based strategies to reduce inflammation and lower hsCRP levels:
Regular Physical Activity
Exercise is one of the most powerful inflammation fighters. Aim for 150 minutes of moderate-intensity aerobic activity weekly to reduce hsCRP.
Heart-Healthy Diet
Mediterranean-style diets rich in omega-3 fatty acids, fruits, vegetables, and whole grains consistently lower hsCRP.
Weight Management
Obesity drives inflammation. Even modest weight loss—5-10% of body weight—can significantly reduce hsCRP levels.
Smoking Cessation
Smoking increases inflammation and hsCRP. Quitting provides rapid benefits to your cardiovascular system.
Stress Management
Chronic stress elevates hsCRP. Practices like meditation, yoga, and mindfulness reduce inflammation.
Quality Sleep
Poor sleep disrupts inflammatory pathways. Aim for 7-9 hours nightly to support healthy hsCRP levels.
Managing Infections
Treating chronic infections and maintaining dental health prevent elevation of hsCRP.
The Controversy: Does hsCRP Deserve a Seat at the Table?
Not all cardiologists enthusiastically endorse routine hsCRP testing. Here's why some remain skeptical:
Arguments Against Routine hsCRP Testing
Elevated hsCRP might simply reflect other underlying health problems rather than unique cardiovascular risk
hsCRP can be elevated by infections, recent surgery, or other acute conditions, potentially leading to unnecessary testing
Adding hsCRP measurement to standard risk assessment might not change treatment decisions for most patients
Cost considerations: Is routine testing financially justified for widespread use?
Arguments Supporting hsCRP Testing
Research (especially Hartley et al., 2025) demonstrates that hsCRP provides independent, long-term predictive value
For intermediate-risk patients, hsCRP helps identify those who need preventive medication
The test is inexpensive, safe, and modifiable through lifestyle changes
For autoimmune patients and heart attack survivors, hsCRP offers valuable risk information
FAQs About hsCRP and Cardiovascular Health
Q: Can I have a normal cholesterol level but high hsCRP? A: Yes, absolutely. hsCRP measures inflammation, not cholesterol. Some people have normal lipids but significant arterial inflammation—which is why hsCRP provides complementary information.
Q: How often should I get hsCRP tested? A: This depends on your individual situation. Ask your cardiologist about appropriate testing intervals based on your risk profile.
Q: Can medications lower hsCRP? A: Yes. Statins, certain blood pressure medications, and anti-inflammatory medications can reduce hsCRP levels.
Q: Is hsCRP testing covered by insurance? A: Coverage varies by insurance plan and clinical indication. Check with your insurance provider about coverage details.
Q: Can hsCRP be elevated from a cold or minor infection? A: Yes. hsCRP responds to any inflammatory stimulus. It's best to test when you're feeling well and free from acute illness.
Q: What's the difference between CRP and hsCRP? A: hsCRP (high-sensitivity) can measure lower levels of inflammation than standard CRP testing, making it more suitable for cardiovascular risk assessment.
Q: If my hsCRP is elevated, will I definitely have a heart attack? A: No. Elevated hsCRP indicates increased risk, but many people with high hsCRP never experience heart disease. Risk factors work together, not in isolation.
Key Takeaways: What You Need to Know About hsCRP
hsCRP is a marker of inflammation that helps identify cardiovascular disease risk beyond traditional factors
Five major 2025-2026 studies confirm that hsCRP measurement provides valuable prognostic information, particularly for:
Intermediate-risk patients
Those with autoimmune diseases
Heart attack survivors
Long-term cardiovascular risk assessment
Elevated hsCRP is associated with vulnerable plaque characteristics and predicts long-term cardiovascular events
hsCRP levels are modifiable through exercise, diet, weight management, stress reduction, and sleep improvement
hsCRP testing is most useful as part of comprehensive cardiovascular assessment, not as a standalone screening tool
Not all patients need hsCRP testing, but it's particularly valuable in specific clinical scenarios identified by recent research
Next Steps: Should You Ask Your Doctor About hsCRP Testing?
If any of these descriptions apply to you, consider discussing hsCRP testing with your healthcare provider:
You have intermediate cardiovascular risk and your doctor is uncertain about starting preventive medications
You have an autoimmune disease and want comprehensive cardiovascular risk assessment
You've experienced a heart attack or other acute cardiovascular event
You have a strong family history of early heart disease
You want to optimize your heart health and understand all relevant risk markers
Remember, hsCRP is one piece of a much larger puzzle. Your comprehensive cardiovascular health assessment should include blood pressure, cholesterol levels, glucose control, physical fitness, stress levels, and lifestyle factors.
Author’s Note
Cardiovascular disease remains the leading cause of morbidity and mortality worldwide, despite decades of progress in lipid management, blood pressure control, and lifestyle modification. One of the central motivations behind this article was to highlight a growing shift in cardiovascular science—from a purely lipid-centric model toward a more integrated understanding that recognizes chronic inflammation as a key driver of atherosclerosis and plaque instability.
High-sensitivity C-reactive protein (hsCRP) is not a new biomarker, but recent high-quality studies from 2025–2026 have clarified where it adds value and where it does not. This article was written to bridge the gap between emerging evidence and real-world clinical decision-making, particularly for patients who fall into “gray zones” of risk where traditional calculators may underestimate danger. Special attention was given to populations often overlooked in preventive cardiology, including individuals with autoimmune inflammatory diseases and patients recovering from acute coronary syndromes.
The goal was not to promote routine hsCRP testing for everyone, but to present a balanced, evidence-based perspective on its selective use as a complementary tool for risk stratification. Wherever possible, findings were grounded in peer-reviewed research, long-term outcome data, and imaging-based studies to avoid oversimplification or biomarker hype.
Ultimately, hsCRP should be viewed not as a standalone diagnostic test, but as part of a broader, patient-centered approach to cardiovascular prevention—one that emphasizes modifiable inflammation through lifestyle, medical therapy, and long-term risk awareness. It is my hope that this article helps clinicians make more informed decisions and empowers readers to engage in meaningful conversations with their healthcare providers about cardiovascular risk and prevention.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Individual circumstances vary, and treatment decisions should always be made in consultation with qualified healthcare professionals.
Related Articles
Cardiovascular Inflammaging: Understanding How Chronic Inflammation Ages Your Heart | DR T S DIDWAL
Your Body Fat Is an Endocrine Organ—And Its Hormones Shape Your Heart Health | DR T S DIDWAL
hsCRP Explained: What Inflammation Means for Your Heart | DR T S DIDWAL
What’s New in the 2025 Blood Pressure Guidelines? A Complete Scientific Breakdown | DR T S DIDWAL
Low-Fat vs. Low-Carb: Which Diet is Best for Weight Loss? | DR T S DIDWAL
References
Fröbert, O., Stone, G. W., Larsen, A. I., Zhou, Z., Kotinkaduwa, L. N., Engstrøm, T., Kjøller-Hansen, L., Maeng, M., Matsumura, M., Ben-Yehuda, O., Bøtker, H. E., Persson, J., Wiseth, R., Jensen, L. O., Nordrehaug, J. E., Trovik, T., Jensen, U., Bleie, Ø., James, S. K., … Maehara, A. (2025). Relationships of hsCRP to high-risk vulnerable plaque after NSTEMI: Insights from the PROSPECT II trial. JACC: Cardiovascular Interventions, 18(10), 1217–1228. https://doi.org/10.1016/j.jcin.2025.01.440
Hartley, A., Rostamian, S., Kaura, A., Chrysostomou, P., Welsh, P., Ariti, C., Sattar, N., Sever, P., & Khamis, R. (2025). The relationship of baseline high-sensitivity C-reactive protein with incident cardiovascular events and all-cause mortality over 20 years. eBioMedicine, 117, 105786. https://doi.org/10.1016/j.ebiom.2025.105786
Hernandez Ortega, D., Faridi, K., & Dastmalchi, L. (2025, December 1). Prioritizing health | hsCRP: A promising risk assessment tool. Cardiology Magazine, American College of Cardiology. https://www.acc.org/latest-in-cardiology/articles/2025/12/01/01/prioritizing-health-hscrp
Mehta, A., Blumenthal, R. S., Gluckman, T. J., Feldman, D. I., & Kohli, P. (2025). High-sensitivity C-reactive protein in atherosclerotic cardiovascular disease: To measure or not to measure? US Cardiology, 19, e06.
Shende, P., Kore, T. A., Lapsiwala, V. H., & Mangal, S. (2026). Correlation of high-sensitivity C-reactive protein and fasting lipid profile for assessing cardiovascular risk factors in patients with autoimmune connective tissue disorders: A cross-sectional study. Journal of Clinical and Diagnostic Research, 20(1), OC05–OC09. https://doi.org/10.7860/JCDR/2026/79872.22204