Dietary Protein and Glycemic Control: Evidence from the Latest Diabetes Research
Are you eating enough protein to manage your diabetes? Learn the ideal daily intake, the best protein sources for insulin sensitivity, and how to protect your kidneys while staying ful
DIABETES
Dr. T.S. Didwal, M.D.(Internal Medicine)
1/2/202615 min read
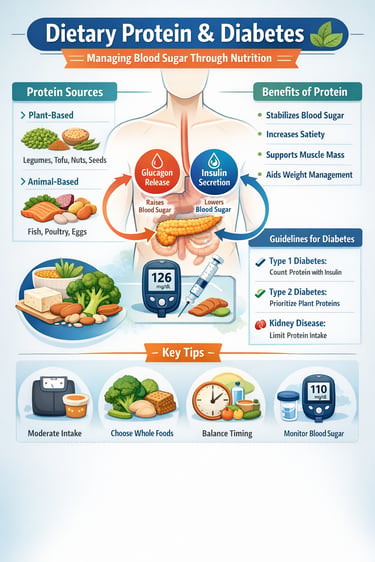
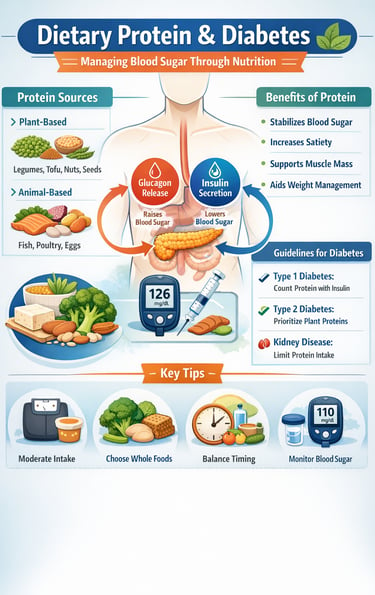
For millions of people living with type 1 diabetes and type 2 diabetes, food choices are not just about calories—they directly influence blood glucose control, insulin requirements, and long-term cardiometabolic health. Among all macronutrients, dietary protein remains one of the most misunderstood components of the diabetic diet. Is protein truly “blood-sugar neutral,” or does it subtly alter insulin and glucagon dynamics? And does the source of protein—animal-based versus plant-based—really matter?
Emerging research from 2023–2025 reveals that protein plays a far more active role in glucose metabolism than previously believed. Studies now show that protein ingestion can influence post-meal glycemic responses, stimulate glucagon secretion, and modify insulin needs, particularly in individuals with type 1 diabetes (Dao et al., 2025; Nagy et al., 2025). At the same time, large cohort studies and meta-analyses indicate that protein quality and source strongly affect insulin sensitivity, type 2 diabetes risk, and cardiovascular outcomes—with plant-based proteins and legumes consistently associated with better metabolic profiles (Xu et al., 2025; Namazi et al., 2025).
For people with diabetes and chronic kidney disease, the story becomes even more nuanced, as carefully tailored protein intake may slow disease progression while improving glycemic stability (Liu et al., 2025). Understanding how protein works—beyond simple grams per day—is now essential for truly personalized diabetes care.
In this comprehensive guide, we'll walk through what the latest evidence tells us about protein and diabetes, explore cutting-edge research from 2023-2025, and help you understand how to make informed nutritional choices for your health.
Clinical pearls
1. Protein Isn't a "Free" Food for Type 1s
For years, education focused solely on carbs. However, protein triggers glucagon secretion, which prompts the liver to release stored glucose. If you have Type 1 diabetes, a high-protein meal without carbohydrates may still require a delayed or "split" insulin bolus to prevent a late-climb spike 3 to 5 hours later.
2. The "Legume Advantage" for Heart Health
While animal proteins provide complete amino acids, plant proteins (like lentils and chickpeas) come bundled with viscous fiber. This fiber slows down gastric emptying and creates a "halo effect" that improves insulin sensitivity and lowers LDL cholesterol. For Type 2 management, replacing just one serving of red meat with legumes can significantly reduce systemic inflammation.
3. "Protein-First" Eating Patterns
The order in which you eat matters. Recent studies suggest that consuming protein and vegetables before carbohydrates in a meal can significantly dampen the post-prandial (after-meal) glucose spike. This is because the protein stimulates GLP-1 (a gut hormone) even before the sugar hits your system, preparing your body to handle the glucose more efficiently.
4. The Kidney "Grit" Factor
In the early stages of diabetic kidney disease, the kidneys are in a state of hyperfiltration—essentially working in overdrive. High-protein diets act like "gritty" fuel for these filters. Reducing intake to the recommended 0.6 to 0.8 g/kg of body weight acts like a pressure-release valve, preserving kidney function for years longer than a standard high-protein diet would.
5. BCAAs: The Double-Edged Sword
Branched-chain amino acids (BCAAs), like those found in whey protein and red meat, are excellent for muscle synthesis. However, in a state of high caloric intake and low activity, high levels of BCAAs can actually interfere with insulin signaling. The pearl? If you’re using protein to build muscle, ensure you’re actually doing the resistance training to utilize those amino acids; otherwise, they may contribute to insulin resistance.
Dietary Protein and Diabetes: A Comprehensive Evidence-Based Guide to Managing Blood Sugar Through Nutrition
Why Protein Matters for Blood Sugar Control
Before diving into the research, let's establish why protein intake matters so much for glucose management. Unlike carbohydrates, which rapidly enter the bloodstream and spike blood sugar, protein has a more complex relationship with blood glucose levels.
Protein digestion triggers the release of glucagon and affects insulin secretion differently than carbs do (Nagy et al., 2025). This is why understanding protein's glycemic impact is crucial for anyone managing diabetes. The emerging evidence suggests that not all protein works the same way in the body, and timing matters significantly.
The Rising Concern About Diabetes and Diet
The World Health Organization reports that over 400 million people globally live with diabetes. In India alone, diabetes affects more than 77 million people, making nutritional management absolutely essential. This is precisely why recent research on dietary protein and cardiometabolic risk factors has become so important.
Breaking Down the Latest Research: What Studies Show
Study 1: Protein Ingestion and Type 1 Diabetes (Dao et al., 2025)
Study Overview
Dao and colleagues conducted a groundbreaking study examining the glycemic impact of protein ingestion in people with type 1 diabetes. Published in Diabetes Care in 2025, this research directly addresses a gap in diabetes management—how protein affects glucose dynamics in insulin-dependent individuals.
Key Findings
The research demonstrated that protein ingestion has measurable effects on insulin requirements and blood glucose patterns in people with type 1 diabetes (Dao et al., 2025). Unlike popular belief that protein has minimal impact on blood sugar, this study revealed that protein timing and protein quantity significantly influence how the body responds to insulin.
One critical discovery: protein-induced glucagon secretion helps prevent hypoglycemia in some situations but can complicate glucose control in others. This means that people with type 1 diabetes need to account for protein intake when calculating insulin doses—something many diabetes education programs haven't traditionally emphasized.
Key Takeaways for Patients
Protein ingestion is not "free" from a blood sugar perspective
Protein timing matters and should coordinate with insulin administration
Individual responses to dietary protein vary significantly
Glucagon responses to protein intake may prevent low blood sugar episodes
Clinical Relevance
For type 1 diabetes management, this study suggests that current carbohydrate counting approaches may need updating to include protein intake calculations. This is especially important for people using insulin pumps or continuous glucose monitors who can track real-time glucose responses.
Study 2: Registry-Based Cohort and Meta-Analysis (Xu et al., 2025)
Study Overview
Xu and colleagues combined data from a large registry-based cohort study with a comprehensive meta-analysis of prospective cohort studies to examine the association between dietary protein and type 2 diabetes risk. Published in Nutritional Diabetes, this research synthesizes evidence from thousands of participants across multiple studies.
Key Findings
The evidence reveals a complex relationship between total protein intake and type 2 diabetes development. The meta-analysis found that moderate protein consumption—when it replaces refined carbohydrates—is associated with lower diabetes risk (Xu et al., 2025). However, extremely high protein intake, particularly from processed animal sources, may not provide additional benefits and could increase risk for certain subgroups.
Importantly, the study identified that the source of protein matters significantly. Participants who replaced refined grains with legume-based protein showed better glucose control outcomes compared to those who increased red meat consumption.
Key Takeaways for Patients
Moderate protein intake (around 1.0-1.2g per kilogram of body weight) appears optimal for diabetes prevention
Plant-based proteins offer additional protective effects beyond protein alone
Protein quality and source are as important as quantity
Replacing refined carbohydrates with high-quality protein reduces type 2 diabetes risk
Clinical Relevance
This evidence strongly supports dietary pattern approaches emphasizing whole food proteins, particularly plant-based options, for those at risk of type 2 diabetes. The findings align with major diabetes organizations' recommendations for prioritizing protein quality over simply increasing protein quantity.
Study 3: Protein, Amino Acids, and Type 2 Diabetes (Mensink, 2024)
Study Overview
Mensink's 2024 review in Frontiers in Nutrition provides a comprehensive examination of the mechanisms linking dietary protein, amino acids, and type 2 diabetes mellitus. Rather than presenting original research, this review synthesizes current understanding of how protein metabolism affects insulin sensitivity and glucose homeostasis.
Key Findings
The review highlights that specific amino acids—particularly branched-chain amino acids (BCAAs)—have complex effects on insulin secretion and glucose metabolism (Mensink, 2024). While amino acids trigger insulin release, they also serve as building blocks for muscle tissue, which is crucial for glucose uptake and overall metabolic health.
The research identifies a critical distinction: fast-digesting proteins (like whey) produce rapid insulin spikes, while slow-digesting proteins (like casein) create more gradual responses. For diabetes management, the timing and speed of protein digestion can influence glycemic control.
Key Takeaways for Patients
All amino acids don't affect blood sugar equally
Muscle mass is essential for glucose handling; protein intake supports muscle maintenance
Protein timing—spreading intake throughout the day—may be better than concentrated amounts
Food processing affects how quickly protein digests and influences glucose responses
Clinical Relevance
This review emphasizes that protein management in diabetes isn't just about quantity but understanding the biochemistry of how different protein sources and eating patterns influence metabolic pathways. Healthcare providers should help patients select protein sources that provide both amino acid diversity and metabolic benefits.
Study 4: Animal vs. Plant Protein and Cardiometabolic Risk (Namazi et al., 2025)
Study Overview
Namazi and colleagues investigated a crucial question for people with existing type 2 diabetes: does it matter whether dietary protein comes from animal sources or plant sources? Using iso-energetic substitution models (replacing one food with equal calories of another), this 2025 study in the Journal of Diabetes and Metabolic Disorders provides precise evidence about protein source quality.
Key Findings
The research revealed significant differences in cardiometabolic outcomes depending on protein source (Namazi et al., 2025). When people with type 2 diabetes replaced animal protein—particularly processed red meat—with plant-based protein, they experienced improved insulin sensitivity, lower triglyceride levels, reduced blood pressure, improved inflammatory markers, and better cholesterol profiles.
Notably, not all animal protein was equal. Fish and poultry, especially when prepared without heavy processing, showed favorable outcomes compared to red meat. The study also found that legume-based proteins (beans, lentils, chickpeas) provided superior cardiometabolic benefits compared to isolated plant proteins.
Key Takeaways for Patients
Protein source is as important as protein amount for managing type 2 diabetes
Plant-based proteins offer superior cardiovascular benefits
Processed animal proteins should be minimized
Legumes are particularly beneficial for people with diabetes
Whole food sources matter more than processed options
Clinical Relevance
This research directly addresses a gap in diabetes management—the recognition that people with type 2 diabetes often have concurrent cardiovascular risk factors. By choosing plant-based proteins and whole animal protein sources, patients can simultaneously manage blood glucose and reduce heart disease risk.
Study 5: Long-Term Protein Restriction and Diabetes with Kidney Disease (Liu et al., 2025)
Study Overview
Liu and colleagues conducted a crucial 10-year retrospective cohort study examining people with both type 2 diabetes and chronic kidney disease—a common and serious complication. Published in BMC Nutrition, this research answers an important question: should people with diabetic nephropathy restrict dietary protein?
Key Findings
The study demonstrates that long-term dietary protein restriction (approximately 0.6-0.8g per kilogram of body weight daily) significantly benefited people with diabetes and kidney disease (Liu et al., 2025). Benefits included slower kidney disease progression, improved renal function indicators, better blood glucose control, reduced proteinuria (protein in urine), and lower blood pressure.
Importantly, the study found that protein restriction didn't compromise nutritional status when nutritionally adequate plant-based proteins replaced higher quantities of animal proteins. This suggests that protein quality matters more than absolute quantity for this population.
Key Takeaways for Patients
People with diabetes and kidney disease benefit from moderate protein restriction
Plant-based proteins are particularly advantageous for this population
Protein restriction should be individualized based on kidney function stage
Nutritional monitoring is essential during protein restriction
Blood glucose control often improves with appropriate protein management
Clinical Relevance
This research is critical because it provides evidence-based guidance for managing diabetic kidney disease, which affects approximately 30-40% of people with diabetes. Rather than applying generic protein recommendations, individuals with chronic kidney disease need tailored approaches that balance protein needs with kidney function preservation.
Study 6: Expert Opinion on Protein in Indian Diabetes Management (Mohan et al., 2023)
Study Overview
Mohan and colleagues assembled a panel of leading diabetes experts in India to synthesize current knowledge about dietary protein in type 2 diabetes management, particularly considering cultural, economic, and epidemiological factors specific to India. Published in the Journal of the Association of Physicians of India, this expert consensus document addresses unique challenges in diabetes management across diverse populations.
Key Findings
The expert panel emphasized that while protein intake is important, the cultural context and food availability dramatically affect realistic recommendations (Mohan et al., 2023). Key insights include recognition that traditional legume-based diets in India provide excellent protein sources for diabetes management, while plant-based proteins from lentils, beans, and chickpeas align with both cultural preferences and metabolic benefits.
The consensus highlighted that protein intake should account for body composition, physical activity, and renal function, and that individualization is more important than one-size-fits-all guidelines. The panel also cautioned that processed plant-based alternatives may not offer the same benefits as whole food sources.
Key Takeaways for Patients
Recommendations must fit your cultural food context and preferences
Traditional whole food proteins in your diet may already be optimal
Cost-effectiveness matters; you don't need expensive protein supplements
Protein recommendations should be personalized, not standardized
Family and community support enhances success with dietary changes
Clinical Relevance
This expert consensus reminds us that diabetes management isn't about following universal rules but adapting evidence-based principles to individual circumstances. Healthcare providers should work with patients to identify protein sources available, affordable, and acceptable within their specific communities and cultures.
Key Takeaways: What All This Research Means for You
If You Have Type 1 Diabetes
Account for protein intake when calculating insulin doses
Spread protein intake throughout the day
Monitor how different protein sources affect your blood glucose
Work with your diabetes educator to update meal plans to include protein counting
If You Have Type 2 Diabetes
Aim for moderate protein intake (about 1.0-1.2g per kilogram of body weight)
Prioritize plant-based proteins, especially legumes
Replace refined carbohydrates with high-quality protein
Choose whole food sources over processed options
Consider your cardiovascular risk when selecting protein sources
If You Have Diabetes and Kidney Disease
Work with a renal dietitian to determine your protein target
Generally, moderate protein restriction (0.6-0.8g per kilogram) is beneficial
Choose plant-based proteins preferentially
Monitor kidney function and adjust based on lab results
Never self-restrict protein without professional guidance
Universal Recommendations
Protein quality matters more than protein quantity
Whole food sources provide superior benefits compared to processed alternatives
Timing and distribution of protein intake affects blood glucose control
Individual variation is significant; what works for one person may differ for another
Regular monitoring and adjustments are essential
FAQs: Your Protein and Diabetes Questions Answered
Q: How much protein should I eat daily if I have diabetes?
A: The research suggests 1.0-1.2 grams per kilogram of body weight for most people with type 2 diabetes. However, if you have kidney disease, this drops to 0.6-0.8 grams per kilogram. For type 1 diabetes, work with your diabetes educator to incorporate protein counting into your meal planning. Your individual needs depend on factors like body composition, activity level, kidney function, and blood glucose control.
Q: Is plant-based protein better than animal protein for diabetes?
A: According to the research, plant-based proteins—especially legumes—offer superior cardiometabolic benefits for people with diabetes. However, quality animal proteins like fish and poultry are also acceptable. What matters most is choosing whole food sources and minimizing processed meats. The key advantage of plant-based proteins is that they typically come with fiber, minerals, and other beneficial compounds that improve overall metabolic health.
Q: Does protein timing matter for diabetes control?
A: Yes, according to recent research. Spreading protein intake throughout the day appears better than concentrating it in one meal. For type 1 diabetes, protein timing should coordinate with insulin administration. For type 2 diabetes, spacing protein-containing meals helps maintain stable blood glucose levels.
Q: Can protein help prevent low blood sugar (hypoglycemia)?
A: Research suggests that protein ingestion triggers glucagon release, which can help prevent hypoglycemia. However, this effect is individual and depends on other factors like insulin timing and carbohydrate intake. If you experience frequent low blood sugar, discuss protein strategies with your healthcare provider rather than self-adjusting.
Q: Should I take protein supplements or powders?
A: The research consistently shows that whole food protein sources provide superior benefits compared to processed supplements. Whole foods provide not just protein but also fiber, minerals, vitamins, and other beneficial compounds. Unless you have specific nutritional gaps, focus on whole foods first.
Q: How does protein affect insulin resistance?
A: Specific amino acids, particularly branched-chain amino acids, have complex effects on insulin sensitivity. Generally, adequate protein intake combined with muscle-building activity improves insulin sensitivity. However, extremely high protein intake from certain sources may worsen insulin resistance in some people. This is why protein quality and source matter significantly.
Q: Is high-protein diet dangerous for my kidneys?
A: For people without kidney disease, moderate protein intake doesn't harm kidney function. However, if you have chronic kidney disease or diabetes with kidney complications, high protein intake can accelerate kidney disease progression. This is why individualized assessment is essential—don't follow high-protein trends without checking your kidney function first.
Q: Can protein help with weight loss in diabetes?
A: Yes, protein intake supports weight management through increased satiety (feeling full) and preserved muscle mass during weight loss. Research suggests that high-quality protein helps maintain metabolic rate while reducing calorie intake, making it easier to achieve weight loss goals relevant to diabetes management.
Q: How should I adjust protein intake if I'm exercising?
A: Physical activity increases protein needs for muscle recovery and building. People with diabetes who exercise regularly may benefit from protein intake in the 1.2-1.6 grams per kilogram range. Time protein intake within a few hours after exercise for optimal muscle protein synthesis. Always discuss exercise adjustments with your healthcare team to coordinate with medication changes.
Practical Protein Sources for Diabetes Management
Plant-Based Proteins (Recommended Priority)
Legumes: lentils, chickpeas, black beans, kidney beans
Whole grains: quinoa, amaranth, farro
Nuts and seeds: almonds, walnuts, flaxseeds, chia seeds
Soy products: tofu, tempeh, edamame
Vegetables: broccoli, spinach, peas
Quality Animal Proteins (Secondary Priority)
Fish: salmon, sardines, mackerel (omega-3 rich)
Poultry: chicken and turkey (skinless)
Eggs: whole eggs including nutrient-rich yolks
Dairy: Greek yogurt, cottage cheese, cheese (in moderation)
Foods to Minimize
Processed meats: bacon, sausage, deli meats
High-fat animal products: fatty cuts of meat, full-fat dairy
Ultra-processed protein products: may contain added sugars and harmful additives
The Bottom Line: Creating Your Protein Strategy
The latest research paints a clear picture: protein management is a cornerstone of effective diabetes control. However, it's not about following rigid rules but understanding principles and adapting them to your unique circumstances.
Whether you have type 1 diabetes, type 2 diabetes, or diabetes with complications, the evidence consistently points to the importance of protein quality, appropriate quantity, strategic timing, and individual customization.
The studies we've examined—from examining protein's glycemic impact in type 1 diabetes to exploring plant-based vs. animal protein effects on cardiometabolic health to investigating protein restriction benefits for diabetic kidney disease—all contribute to a more nuanced understanding of how nutrition shapes diabetes outcomes.
Take Action Today
Ready to optimize your diabetes management through better protein choices?
Schedule a consultation with a registered dietitian who specializes in diabetes. They can personalize protein recommendations based on your specific situation, kidney function, activity level, and preferences.
Track your current protein intake for three days to establish a baseline. Are you getting enough? Too much? Are you choosing quality sources?
Identify three new plant-based proteins to incorporate into your weekly meals. Start with options aligned with your cultural background and food preferences.
If you have type 1 diabetes, work with your diabetes educator to update your insulin dosing to account for protein intake using the evidence from the latest research.
Monitor your response to dietary protein changes. Use your blood glucose meter or continuous glucose monitor to see how different protein sources and timing affect your blood sugar levels.
Share this information with your healthcare team. Bring these research findings to your next appointment and discuss how they apply to your individual management plan.
Your diabetes management journey is unique, but it's grounded in solid science. By making informed decisions about dietary protein, you're taking a powerful step toward better blood glucose control, improved overall health, and enhanced quality of life.
Author’s Note
This article is intended for educational purposes and reflects the current scientific understanding of dietary protein and diabetes management based on peer-reviewed research published between 2023 and 2025. Nutrition in diabetes is highly individualized; factors such as type of diabetes, kidney function, body composition, medications, physical activity, and cultural dietary patterns significantly influence optimal protein intake. While the evidence discussed here can guide informed decision-making, it should not replace personalized medical or dietary advice. Readers are encouraged to consult their treating physician or a registered dietitian before making significant dietary changes, particularly if they have chronic kidney disease, are on insulin, or have multiple comorbidities. The goal of this article is to empower patients and clinicians alike with clarity, context, and scientifically grounded insight—without oversimplification or fear-based nutrition messaging.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Individual circumstances vary, and treatment decisions should always be made in consultation with qualified healthcare professionals.
Related Articles
Is a Functional Cure for Diabetes Within Reach? The Science of Beta-Cell Restoration | DR T S DIDWAL
SGLT2 Inhibitors Beyond Diabetes: Are We Prescribing Them Too Late? | DR T S DIDWAL
Can Fish Consumption Help Reverse Metabolic Syndrome? What Latest Research Shows | DR T S DIDWAL
The Metabolic Triad: Why Diabetes, Obesity & CVD Are One Epidemic | DR T S DIDWAL
What’s New in the 2025 Blood Pressure Guidelines? A Complete Scientific Breakdown | DR T S DIDWAL
Manage Diabetes Naturally: How Beta-Glucans Control Blood Sugar | DR T S DIDWAL
Exercise as Metabolic Medicine: Latest Research on Glucose and Heart Health| DR T S DIDWAL
References
Dao, G. M., Kowalski, G. M., Bruce, C. R., O'Neal, D. N., Smart, C. E., Zaharieva, D. P., Hennessy, D. T., Zhao, S., & Morrison, D. J. (2025). The glycemic impact of protein ingestion in people with type 1 diabetes. Diabetes Care, 48(4), 509–518. https://doi.org/10.2337/dci24-0096
Liu, D., Li, Q., Jia, R., He, W., Zhao, X., Pan, M., Chen, X., Wang, Y., Zhu, Y., Hou, H., Xie, J., & Wang, W. (2025). Type 2 diabetes mellitus with chronic kidney disease benefits from long-term restriction of dietary protein intake: A 10-year retrospective cohort study. BMC Nutrition, 11(1), 131. https://doi.org/10.1186/s40795-025-01119-w
Mensink, M. (2024). Dietary protein, amino acids and type 2 diabetes mellitus: A short review. Frontiers in Nutrition, 11, 1445981. https://doi.org/10.3389/fnut.2024.1445981
Mohan, V., Misra, A., Bhansali, A., Singh, A. K., Makkar, B., Krishnan, D., Chadha, M., Shah, P., Samaddar, R., Saraogi, R. K., Tiwaskar, M., Saboo, B., Baruah, M. P., Chowdhury, S., Jaggi, S., & Shivaswamy, V. (2023). Role and significance of dietary protein in the management of type 2 diabetes and its complications in India: An expert opinion. Journal of the Association of Physicians of India, 71(12), 36–46. https://doi.org/10.59556/japi.71.0339
Nagy, S., Turner, L. V., & Riddell, M. C. (2025). Effects of protein intake on glucagon, insulin, and glucose dynamics: Implications for diabetes. Frontiers in Clinical Diabetes and Healthcare, 6. https://doi.org/10.3389/fcdhc.2025.1712506
Namazi, N., Anjom-Shoae, J., Darbandi, M., et al. (2025). Dietary intake of total, animal, and vegetable protein and cardiometabolic risk factors in patients with type 2 diabetes: Using iso-energetic substitution models. Journal of Diabetes and Metabolic Disorders, 24, 60. https://doi.org/10.1007/s40200-025-01571-2
Xu, M., Zheng, J., Ying, T., et al. (2025). Dietary protein and risk of type 2 diabetes: Findings from a registry-based cohort study and a meta-analysis of prospective cohort studies. Nutritional Diabetes, 15, 25. https://doi.org/10.1038/s41387-025-00380-z