Can Fish Consumption Help Reverse Metabolic Syndrome? What Latest Research Shows
Marine omega-3 fatty acids reduce liver fat and improve insulin sensitivity. This 2025 evidence review explores MASLD, the “SMASH” fish strategy, and the metabolic importance of fatty acid source.
NUTRITION
Dr. T.S. Didwal, M.D.(Internal Medicine)
1/3/202610 min read
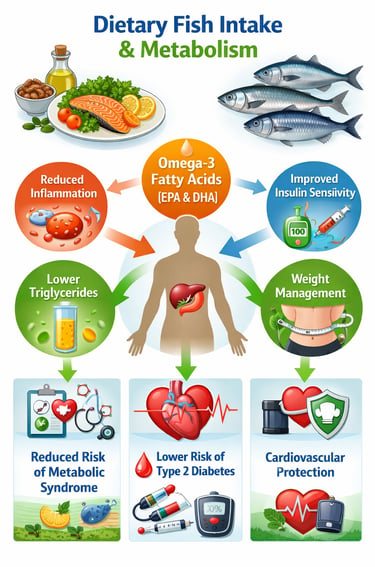
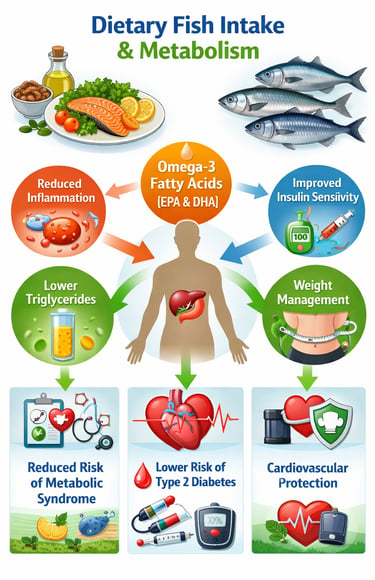
Growing scientific evidence confirms that dietary fish intake and omega-3 fatty acids (EPA and DHA) play a crucial role in maintaining metabolic health. Metabolic syndrome—a cluster of conditions including insulin resistance, abdominal obesity, dyslipidemia, hypertension, and fatty liver disease (MASLD)—is now recognized as largely modifiable through diet. Among dietary interventions, regular fish consumption stands out for its consistent benefits across populations.
Recent cohort studies and meta-analyses show that higher intake of marine n-3 polyunsaturated fatty acids is associated with reduced triglycerides, improved insulin sensitivity, lower systemic inflammation, and decreased liver fat accumulation (Tatoli et al., 2025; Tang et al., 2025). These effects are mediated through multiple mechanisms, including suppression of inflammatory pathways, enhancement of insulin signaling, and favorable changes in lipid metabolism. Umbrella reviews further confirm that fish consumption is linked to lower risk of type 2 diabetes, cardiovascular disease, and metabolic syndrome across diverse populations (Zhao et al., 2023).
Importantly, whole fish provides benefits beyond supplements by delivering high-quality protein, micronutrients, and bioactive compounds that work synergistically with omega-3s (Ofori et al., 2024). Emerging research also highlights nutrigenetic variability, suggesting that individual responses to omega-3 intake may differ based on genetic background (Arunagiri et al., 2025).
Overall, consuming 2–3 servings of omega-3-rich fish per week as part of a Mediterranean-style diet represents a safe, evidence-based strategy to improve metabolic health and reduce long-term cardiometabolic risk.
Clinical pearls
1. The "DHA-EPA" vs. "ALA" Efficiency Gap
Many people believe flaxseeds or walnuts provide all the Omega-3s they need. Scientifically, those contain ALA, which your body must convert into EPA and DHA to protect your heart and liver. The "pearl" here is that humans are remarkably poor converters—often less than 5% becomes usable. To truly reduce liver fat as seen in the NUTRIHEP study, you need the direct "pre-formed" sources found in fatty fish or algae oil.
2. Omega-3s are "Membrane Softeners"
Think of your cell membranes like the "skin" of your cells. When you eat saturated fats, these membranes become rigid. When you consume marine Omega-3s, they incorporate into the cell wall, making it more fluid and flexible. This physical change allows insulin receptors to sit more effectively on the cell surface, which is exactly how fish consumption improves insulin sensitivity and lowers blood sugar.
3. The "SMASH" Fish Strategy
While the 2025 research emphasizes frequency (2-3 times a week), the type of fish is the secret to avoiding toxins. Use the SMASH acronym: Sardines, Mackerel, Anchovies, Salmon, and Herring. These fish are lower on the food chain, meaning they provide the highest concentration of metabolic-saving Omega-3s with the lowest accumulation of mercury.
4. Turning Off the "Fat-Making" Switch in the Liver
Regarding the newly named MASLD (fatty liver), Omega-3s act as biological "gene switches." They suppress a protein called SREBP-1c, which is the primary "on-switch" for the liver to create new fat. Simultaneously, they activate the "burn-switch" (PPAR-alpha). Essentially, eating fatty fish tells your liver to stop storing fat and start using it for fuel.
5. Temperature Matters: Don't Kill the Nutrient
Omega-3 fatty acids are chemically "fragile" because of their double bonds. High-heat deep frying doesn't just add calories; it causes lipid peroxidation, which can turn a healthy fat into a pro-inflammatory one. To preserve the metabolic benefits documented in the Zhao et al. (2023) review, stick to poaching, steaming, or low-temperature baking (under 180°C).
Omega-3 Fatty Acids and Fish Consumption: Your Complete Guide to Better Metabolic Health
If you're concerned about metabolic syndrome, fatty liver disease, or simply want to optimize your health through nutrition, understanding the role of marine n-3 polyunsaturated fatty acids could be transformative. This comprehensive guide synthesizes cutting-edge research to help you make informed dietary decisions.
What Is Metabolic Syndrome and Why Should You Care?
Metabolic syndrome represents a cluster of conditions that occur together, increasing your risk of heart disease, stroke, and type 2 diabetes. These conditions include elevated blood pressure, high blood sugar, excess body fat (especially around the waist), and abnormal cholesterol or triglyceride levels.
More recently, researchers have identified a related condition called metabolic dysfunction-associated steatotic liver disease (MASLD), formerly known as non-alcoholic fatty liver disease. This condition involves excess fat accumulation in liver cells and is increasingly common in modern populations.
The good news? Dietary interventions—particularly increasing fish consumption and omega-3 intake—show remarkable promise in preventing and managing these conditions.
Study 1: Mediterranean Diet and Fish Omega-3s for Liver Health
The Research
Tatoli et al. (2025) conducted research on the NUTRIHEP cohort, examining how dietary omega-3 fatty acids from fish influence the risk of metabolic dysfunction-associated steatotic liver disease in a Mediterranean population. This study represents one of the most current investigations into how fish consumption protects liver health.
Key Takeaways
Mediterranean populations, traditionally consuming higher amounts of fish and seafood, demonstrate lower rates of MASLD
Fish-derived omega-3s demonstrate specific protective mechanisms against liver fat accumulation
The relationship between marine omega-3 polyunsaturated fatty acids and liver health is dose-dependent—more beneficial intake correlates with better outcomes
Dietary patterns rich in fish align with cardiovascular and metabolic benefits simultaneously
What This Means for You
If you're at risk for liver disease or metabolic dysfunction, following a Mediterranean-style eating pattern emphasizing fish consumption offers evidence-based protection. This isn't just theoretical—real population data supports these benefits.
Study 2: China's Metabolic Burden and Low Marine N-3 Intake
The Research
Tang et al. (2025) published groundbreaking research demonstrating that low dietary intake of marine n-3 fatty acids and seafood significantly contributes to metabolic syndrome burden in China. This large-scale investigation reveals how inadequate omega-3 consumption directly correlates with metabolic disease prevalence.
Key Takeaways
Populations consuming insufficient seafood and marine omega-3 sources show substantially higher metabolic syndrome rates
Dietary deficiencies in n-3 fatty acids represent a modifiable risk factor for metabolic disease across diverse populations
Fish consumption patterns could reduce metabolic disease burden at population levels
Even modest increases in omega-3 intake from seafood may yield significant public health benefits
What This Means for You
This research reveals that metabolic syndrome isn't inevitable—it's partly a function of dietary choices. If your current diet lacks fish and seafood, increasing consumption could meaningfully improve your metabolic health markers.
Study 3: Nutrigenetics and Dietary Contributors to Metabolic Health
The Research
Arunagiri et al. (2025) published an editorial in Frontiers in Endocrinology examining dietary and nutrigenetic contributors to metabolic syndrome. This perspective piece emphasizes how genetic variations interact with dietary components, including omega-3 fatty acids, to influence metabolic outcomes.
Key Takeaways
Nutrigenetics—how genes interact with dietary nutrients—plays a significant role in metabolic disease susceptibility
Personalized nutrition approaches considering both diet and genetic factors may optimize metabolic health outcomes
Omega-3 fatty acids represent key nutrients in nutrigenetic-informed dietary strategies
One-size-fits-all dietary recommendations may miss opportunities for personalized interventions
What This Means for You
While fish consumption benefits most people, understanding your genetic predisposition to metabolic disorders could help tailor your approach. Consulting with a nutritionist familiar with nutrigenomics might reveal whether higher or moderate omega-3 intake serves your particular health needs best.
Study 4: Fish Consumption and Multiple Health Outcomes Meta-Analysis
The Research
Zhao et al. (2023) conducted an umbrella review of meta-analyses examining fish consumption in multiple health outcomes. This comprehensive synthesis analyzed numerous observational and clinical studies, providing powerful evidence about fish's protective effects.
Key Takeaways
Fish consumption demonstrates protective associations across multiple health domains—not just metabolic health
Seafood nutrients, particularly omega-3 polyunsaturated fatty acids, show consistent benefits in research
The evidence base supporting fish intake recommendations comes from thousands of individual studies
Consistent associations across diverse populations strengthen confidence in fish's health benefits
What This Means for You
When multiple high-quality reviews reach similar conclusions about fish consumption, the evidence becomes particularly compelling. This research confirms that eating fish more regularly addresses numerous health concerns simultaneously.
Study 5: Fish Consumption's Preventive Role in Metabolic Syndrome
The Research
Tørris et al. (2014) conducted a systematic review examining fish consumption's preventive role in metabolic syndrome development and prevalence. Although published in 2014, this research remains foundational for understanding fish's metabolic benefits.
Key Takeaways
Regular fish consumption shows a protective association with lower metabolic syndrome prevalence
Omega-3 rich fish varieties provide superior metabolic benefits compared to fish with lower omega-3 content
Frequency of fish consumption matters—consistent intake produces better outcomes than occasional consumption
Fish proteins and micronutrients complement omega-3 benefits for metabolic health
What This Means for You
Consistency matters. Eating fish occasionally provides less benefit than regular weekly consumption. Aiming for multiple fish servings weekly leverages the metabolic protective effects these studies document.
Study 6: Dietary Fat Intake and Metabolic Health—A Comprehensive Analysis
The Research
Ofori et al. (2024), particularly omega-3 polyunsaturated fatty acids, ) provided an in-depth analysis of dietary fat intake on metabolic health, synthesizing epidemiological, clinical, and animal studies. This comprehensive review clarifies how different fat types—particularly omega-3 polyunsaturated fatty acids—influence metabolic outcomes.
Key Takeaways
Not all dietary fats affect metabolic health equally; omega-3s show particularly beneficial effects
Animal models confirm mechanisms by which marine omega-3 fatty acids improve insulin sensitivity and reduce inflammation
Clinical evidence supports that omega-3 supplementation and fish consumption reduce metabolic disease markers
Replacing saturated fats with omega-3 sources offers metabolic advantages beyond simple calorie reduction
What This Means for You
The type of fat you consume matters profoundly. Prioritizing fish-based omega-3s over other fat sources can meaningfully improve your metabolic health markers.
The Science Behind Omega-3 Benefits: How Fish Protects Metabolic Health
Anti-Inflammatory Effects
Omega-3 polyunsaturated fatty acids reduce systemic inflammation—a key driver of metabolic dysfunction. Chronic inflammation contributes to insulin resistance, fatty liver disease, and metabolic syndrome development.
Improved Insulin Sensitivity
Research demonstrates that marine n-3 fatty acids enhance how your cells respond to insulin, reducing blood sugar and supporting better metabolic control.
Triglyceride Reduction
Fish consumption consistently lowers triglycerides, a critical metabolic syndrome component that increases cardiovascular risk.
Liver Fat Reduction
As the NUTRIHEP study emphasized, fish-derived omega-3s specifically target hepatic fat accumulation, protecting against metabolic dysfunction-associated steatotic liver disease.
Healthy Lipid Profiles
Omega-3 rich fish improve cholesterol ratios, increasing beneficial HDL and reducing harmful LDL particles.
Practical Guidance: How Much Fish Should You Eat?
General Recommendations
Most research supports 2-3 servings of fish weekly, with each serving containing 3.5 ounces (100 grams) of cooked fish.
Best Fish Choices for Omega-3 Content
High omega-3 fish include:
Salmon (wild-caught preferred)
Sardines
Mackerel
Herring
Anchovies
Trout
Moderate omega-3 fish include:
Tuna (fresh, not canned in oil)
Sea bass
Halibut
Preparation Matters
Baking, grilling, or steaming preserves omega-3 content. Avoid deep frying, which can damage these delicate nutrients and introduce unhealthy trans fats.
Mercury Considerations
While fish benefits are substantial, be aware of mercury content. Vary your fish choices and limit high-mercury varieties (shark, swordfish, king mackerel) to occasional consumption.
Frequently Asked Questions
Q: Can I get sufficient omega-3s from plant sources alone?
A: While some plant foods contain alpha-linolenic acid (ALA), your body converts only 5-10% to the active forms—EPA and DHA—found in fish. Marine omega-3 sources provide these forms directly, making fish significantly more efficient for meeting omega-3 needs.
Q: What if I'm vegetarian or allergic to fish?
A: Algae supplements contain EPA and DHA (the active omega-3 forms) without fish. Additionally, walnuts, flaxseeds, and chia seeds provide ALA, though conversion remains limited. Consult a healthcare provider about supplementation.
Q: How long does it take to see metabolic improvements from eating more fish?
A: Research shows measurable improvements in metabolic markers within 4-8 weeks of consistent increased fish consumption. Full benefits may take 3-6 months.
Q: Is fish oil supplementation as effective as eating whole fish?
A: While fish oil supplements contain omega-3s, whole fish provides additional nutrients—proteins, vitamins, minerals—that work synergistically. When possible, prioritize whole fish; supplements complement but don't completely replace whole foods.
Q: Can I reverse metabolic syndrome through fish consumption alone?
A: Fish consumption represents one powerful component of metabolic health recovery. Combined with regular physical activity, stress management, adequate sleep, and overall healthy eating patterns, fish significantly contributes to reversal of metabolic dysfunction.
Q: Are there fish I should avoid due to contamination concerns?
A: Focus on sustainably sourced, wild-caught (or responsibly farmed) fish from reputable sources. Avoid fish from heavily polluted waters. Most common supermarket fish meet safety standards.
Call to Action: Start Your Metabolic Health Transformation Today
The research is clear: fish consumption and omega-3 fatty acids offer a scientifically validated pathway to better metabolic health. You don't need complicated interventions or expensive supplements—simply incorporating more fish into your weekly diet can meaningfully improve your health outcomes.
Your Next Steps:
Assess your current fish intake. Are you reaching 2-3 weekly servings? If not, identify barriers to increased consumption.
Choose your favorite high-omega-3 fish. Salmon, sardines, and mackerel offer excellent options. Find preparation methods you enjoy.
Plan a weekly fish-based meal. Start with one additional fish meal weekly and gradually increase frequency.
Monitor your health markers. Work with your healthcare provider to track metabolic improvements—blood sugar, triglycerides, blood pressure, liver enzymes.
Consider professional guidance. A registered dietitian familiar with nutrigenomics can help personalize recommendations based on your unique needs and genetic predispositions.
Author’s Note
This article is intended to provide a clear, evidence-based overview of the evolving role of dietary fish intake and marine omega-3 fatty acids in metabolic health, particularly in the context of metabolic syndrome and metabolic dysfunction–associated steatotic liver disease (MASLD). The interpretations presented here are derived from peer-reviewed human studies, systematic reviews, and mechanistic research published up to 2025, with an emphasis on clinical relevance rather than nutritional dogma.
Nutrition science is inherently complex and individualized. While the data supporting the metabolic benefits of omega-3 fatty acids—especially from whole fish sources—are increasingly robust, responses vary depending on genetics, baseline metabolic status, dietary patterns, and coexisting conditions such as diabetes or cardiovascular disease. For this reason, the findings discussed should be viewed as guiding principles rather than universal prescriptions.
This article does not advocate high-dose supplementation or extreme dietary approaches. Instead, it highlights the importance of fatty acid quality, food source, and dietary context, which are often overlooked in simplified nutrition messaging. Readers are encouraged to interpret these findings in consultation with qualified healthcare professionals, particularly when managing chronic metabolic or liver-related conditions.
The goal of this work is to bridge scientific rigor with practical understanding—empowering clinicians, researchers, and informed readers to make nutrition decisions grounded in physiology, evidence, and long-term metabolic health.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Individual circumstances vary, and treatment decisions should always be made in consultation with qualified healthcare professionals.
Related Articles
What’s New in the 2025 Blood Pressure Guidelines? A Complete Scientific Breakdown | DR T S DIDWAL
Low-Fat vs. Low-Carb: Which Diet is Best for Weight Loss? | DR T S DIDWAL
5 Steps to Reverse Metabolic Syndrome: Diet, Habit, & Lifestyle Plan | DR T S DIDWAL
The Role of Cholesterol in Health and Disease: Beyond the "Bad" Label | DR T S DIDWAL
Lowering Cholesterol with Food: 4 Phases of Dietary Dyslipidemia Treatment | DR T S DIDWAL
High Triglyceride Levels: 5 New Facts to Help You Lower Your Risk | DR T S DIDWAL
The Best Dietary Fat Balance for Insulin Sensitivity, Inflammation, and Longevity | DR T S DIDWAL
Feed Your Gut, Fuel Your Health: Diet, Microbiota, and Systemic Health | DR T S DIDWAL
References
Arunagiri, A., Alam, M., Dror, E., & Kebede, M. A. (2025). Editorial: Dietary and nutrigenetic contributors to metabolic syndrome. Frontiers in endocrinology, 16, 1632753. https://doi.org/10.3389/fendo.2025.1632753
Ofori, S. A., Dwomoh, J., Owusu, P., Kwakye, D. O., Osei Kyeremeh, O., Frimpong, D. K., & Aggrey, M. L. (2024). Dietary fat intake on metabolic health: An in-depth analysis of epidemiological, clinical, and animal studies. American Journal of Biomedical and Life Sciences, 12(4), 68–77. https://doi.org/10.11648/j.ajbls.20241204.12
Tatoli, R., Caterina, B., Donghia, R., Pesole, P. L., Fontana, L., & Giannelli, G. (2025). Dietary omega-3 fatty acids from fish and risk of metabolic dysfunction-associated steatotic liver disease in a Mediterranean population: Findings from the NUTRIHEP cohort. Nutrients, 17(21), 3372. https://doi.org/10.3390/nu17213372
Tang, X., Zhuang, P., Wu, S., Liu, X., Lu, X., Wu, Y., Yan, Z., Li, Y., Zhang, Y., & Jiao, J. (2025). Low dietary intake of marine n-3 fatty acids and seafood significantly contributes to metabolic syndrome burden in China. Nutrition Research (New York, N.Y.), 140, 1–10. https://doi.org/10.1016/j.nutres.2025.04.013
Tørris, C., Molin, M., & Cvancarova Småstuen, M. (2014). Fish consumption and its possible preventive role on the development and prevalence of metabolic syndrome—a systematic review. Diabetology & Metabolic Syndrome, 6(1), 112. https://doi.org/10.1186/1758-5996-6-112
Zhao, H., Wang, M., Peng, X., Zhong, L., Liu, X., Shi, Y., Li, Y., Chen, Y., & Tang, S. (2023). Fish consumption in multiple health outcomes: An umbrella review of meta-analyses of observational and clinical studies. Annals of Translational Medicine, 11(3), 152. https://doi.org/10.21037/atm-22-6515