Diabetes and Thyroid Dysfunction: Clinical Insights Into Their Shared Pathway of Insulin Resistance
Struggling with diabetes management? Discover the hidden connection between insulin resistance and thyroid dysfunction. Learn why treating your thyroid is essential for blood sugar control, weight loss, and metabolic health based on 2025 research.
DIABETES
Dr. T.S. Didwal, M.D.(Internal Medicine)
1/17/202613 min read
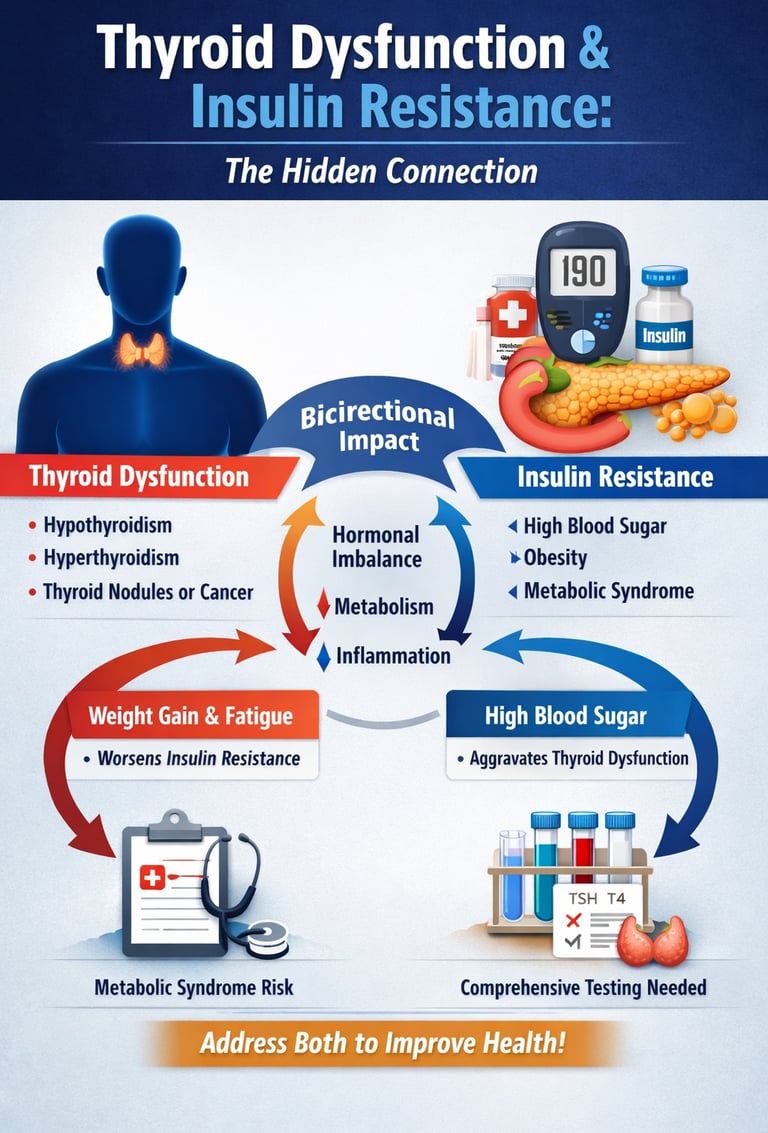
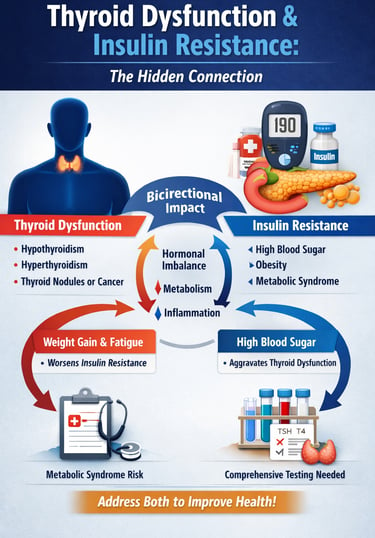
Why do millions of people continue to struggle with stubborn weight gain, chronic fatigue, and uncontrolled blood sugar—even when they follow diet and exercise plans faithfully? Emerging research suggests the answer may lie in a powerful but often overlooked interaction between two major hormonal systems: the thyroid gland and insulin signaling pathways.
Over the past decade, scientists have discovered that thyroid dysfunction and insulin resistance are not separate issues at all—they are deeply interconnected metabolic disorders that amplify each other in a vicious cycle (Razvi, 2026). What’s even more alarming is that this relationship often goes undetected for years. Many patients are treated for diabetes without their thyroid ever being checked, or diagnosed with hypothyroidism while the underlying insulin resistance silently worsens in the background.
Recent studies show that individuals with thyroid disease are significantly more likely to develop insulin resistance and metabolic syndrome—even when body weight is controlled for (Krishnamurthy et al., 2025). Meanwhile, insulin resistance can impair thyroid hormone activity at the tissue level, making conventional treatment less effective (Safari et al., 2024).
In other words: if you’re treating only one condition, you may be unintentionally allowing the other to sabotage your progress. Understanding this hidden connection could be the key to unlocking better energy, weight control, and metabolic health.
In this comprehensive guide, we'll explore the latest 2025 research on how these conditions interact, what it means for your health, and what you can do about it.
Clinical pearls—critical intersection of thyroid health and metabolic function.
1. The "T4 to T3" Conversion Bottleneck
Think of T4 as a "storage" hormone and T3 as the "active" fuel your cells actually use. Insulin resistance often acts like a roadblock in the liver, preventing the conversion of T4 into the active T3. Even if your TSH (screening) looks normal, your body may be in a state of "cellular hypothyroidism" because the active fuel isn't reaching its destination. This is why many patients feel symptomatic despite having "normal" lab results.
2. The Abdominal Fat Feed-Forward Loop
Insulin resistance promotes the accumulation of visceral (abdominal) fat. This specific type of fat is metabolically active and secretes inflammatory cytokines. These inflammatory signals can directly interfere with thyroid hormone receptors, making your thyroid hormones less effective. In short: metabolic inflammation makes your cells "deaf" to the thyroid’s signals, leading to further weight gain and fatigue.
3. TSH is a Leading Indicator for Heart Health
Your TSH level isn't just a thyroid marker; it's a metabolic weather vane. Research shows that as TSH rises—even within the "high-normal" range—levels of LDL cholesterol and triglycerides often rise with it. If you are struggling with high cholesterol that doesn't respond to diet, the root cause may be a sluggish thyroid failing to signal the liver to clear fats from the blood.
4. Muscle: The Engine Room for Both Systems
Skeletal muscle is the primary site for both glucose disposal (managed by insulin) and heat production (managed by thyroid hormone). When thyroid levels are low, muscle mass can become less metabolically efficient. Engaging in resistance training doesn't just "burn calories"; it physically increases the number of thyroid hormone receptors and insulin receptors in the body, essentially "upgrading" your metabolic hardware.
5. The "Hypo-G" Seesaw
Thyroid dysfunction can make blood sugar management feel like a rollercoaster. Hypothyroidism slows the rate at which glucose is absorbed from the gut and cleared from the blood, which can lead to unpredictable "lows" (hypoglycemia) followed by sustained "highs." If your glucose readings are erratic despite a consistent diet, stabilizing your thyroid levels is often the "anchor" needed to steady your blood sugar.
Thyroid Dysfunction and Insulin Resistance: Understanding the Hidden Connection Between Two Silent Epidemics
Why Thyroid and Metabolic Health Matter
According to Razvi's 2026 analysis in Nature Reviews Endocrinology, diabetes mellitus and thyroid disease represent a genuine public health burden that demands immediate attention. These aren't isolated problems—they're interconnected metabolic disasters that amplify each other's effects.
Thyroid disease affects approximately 200 million people worldwide, while diabetes impacts over 400 million individuals. What's alarming is the overlap: people with thyroid dysfunction have significantly higher rates of insulin resistance and poor metabolic control, and vice versa.
But why does this matter to you? Because untreated thyroid dysfunction can sabotage your efforts to manage blood sugar levels, making diabetes prevention and weight management feel impossible.
Study 1: Insulin Resistance in Thyroid Nodules and Differentiated Thyroid Cancer
Iuliano et al. (2025) conducted a comprehensive examination of insulin resistance and metabolic dysfunction in patients with thyroid nodules and differentiated thyroid cancer. Published in Current Opinion in Oncology, this research bridges two seemingly separate fields: oncology and metabolic medicine.
The significance of this study lies in its novel perspective: metabolic abnormalities aren't just complications of thyroid cancer—they may actually be driving factors in disease development and progression.
Key Takeaways
Insulin resistance is present in a substantial proportion of thyroid cancer patients
Metabolic dysfunction appears to influence thyroid cancer biology and outcomes
Thyroid nodules are frequently accompanied by glucose metabolism abnormalities
The relationship suggests potential therapeutic opportunities through metabolic intervention
Obesity and insulin resistance may increase cancer risk and complicate treatment
For patients with thyroid disease, this research underscores the importance of screening for metabolic syndrome and insulin resistance. If you have thyroid cancer or thyroid nodules, discussing your metabolic health status with your healthcare provider becomes critically important.
Study 2: Association Between Thyroid Dysfunction and Insulin Resistance—A Cohort Study
Krishnamurthy et al. (2025) published a robust retrospective cohort study in BMJ Open examining the association between thyroid dysfunction and insulin resistance. This large-scale analysis provides compelling evidence that these conditions are tightly linked.
Rather than relying on small samples, the researchers analyzed substantial patient populations over extended periods, allowing them to identify patterns and causality that smaller studies might miss.
Key Takeaways
Thyroid dysfunction (both hypothyroidism and hyperthyroidism) correlates with elevated insulin resistance levels
The association persists even after controlling for obesity and body mass index (BMI)
TSH levels (thyroid-stimulating hormone) may serve as predictors of metabolic dysfunction
Early detection of thyroid abnormalities could facilitate early diabetes prevention
The relationship appears bidirectional—each condition can worsen the other
If you've been diagnosed with thyroid disease, you're at an elevated risk for metabolic dysfunction. Conversely, if you have prediabetes or type 2 diabetes, screening for thyroid disorders becomes a priority. This isn't redundant testing—it's comprehensive metabolic management.
Study 3: Thyroid Function and Insulin Resistance Using METS-IR Index
Safari et al. (2024) leveraged data from the National Health and Nutrition Examination Survey (NHANES) spanning 2007–2012 to investigate the association between thyroid function and insulin resistance using the Metabolic Score for Insulin Resistance (METS-IR). This sophisticated metric provides a more nuanced assessment than traditional measures like HOMA-IR.
The use of METS-IR is particularly valuable because it incorporates metabolic syndrome parameters beyond simple insulin-glucose ratios, offering a comprehensive picture of metabolic health.
Key Takeaways
Thyroid function parameters strongly predict insulin resistance as measured by METS-IR
Free T4 levels (thyroid hormone) show inverse associations with insulin resistance
TSH elevation correlates with higher insulin resistance scores
The association holds across diverse demographic groups
Thyroid optimization may improve metabolic markers even without medication
This research validates using sophisticated assessment tools like METS-IR rather than outdated measures. If your doctor is only checking fasting glucose and insulin levels, ask about metabolic syndrome screening and comprehensive thyroid panels. A full picture requires a comprehensive evaluation.
Study 4: Thyroid Disorders in Diabetic and Hypertensive Patients in India
Sharma et al. (2025) conducted a systematic review and meta-analysis examining the prevalence of thyroid disorders in patients with diabetes and hypertension in India. This research is particularly important because it highlights how the thyroid-metabolic connection manifests in diverse populations.
India's growing burden of metabolic disease makes this analysis especially relevant. The findings help establish whether the thyroid-insulin resistance association is universal or population-specific.
Key Takeaways
Thyroid disorders are significantly more prevalent in diabetic and hypertensive populations compared to the general population
Hypothyroidism is the most common thyroid dysfunction observed in metabolic disease patients
The prevalence varies by geographic region and population characteristics
Comorbid thyroid disease complicates management of diabetes and hypertension
Early thyroid screening in metabolic disease populations is justified and cost-effective
Autoimmune thyroiditis frequently accompanies metabolic disorders
This study demonstrates that the thyroid-metabolic connection transcends geography and ethnicity. Whether you're in India, North America, or Europe, if you have diabetes or hypertension, your thyroid health deserves attention.
Study 5: Impact of Thyroid Disorders on Type 2 Diabetes Mellitus
Suganya et al. (2025) conducted a cross-sectional study exploring the impact of thyroid disorders on type 2 diabetes mellitus patients, published in the Romanian Medical Journal. This research directly examines how thyroid dysfunction influences diabetes outcomes and glycemic control.
The cross-sectional design allows researchers to identify associations and prevalence rates, establishing the magnitude of the problem in real-world settings.
Key Takeaways
Thyroid disorders significantly impact glycemic control in type 2 diabetes patients
Patients with concurrent thyroid dysfunction experience:
Higher HbA1c levels (average blood sugar over three months)
Greater difficulty achieving blood sugar targets
More frequent hypoglycemic episodes or inconsistent glucose patterns
Increased metabolic complications
TSH levels correlate with diabetes severity and medication requirements
Thyroid treatment optimization can improve metabolic outcomes
Comorbid thyroid disease increases healthcare costs and complexity
If you have type 2 diabetes, this research suggests that treating underlying thyroid dysfunction isn't optional—it's essential for achieving your blood sugar targets. Your diabetes management plan may be hindered by an untreated thyroid condition.
The Mechanism: How Does the Thyroid Affect Insulin Resistance?
You might be wondering: what's the actual mechanism connecting these two systems? The answer involves several interconnected pathways:
1. Metabolic Rate and Energy Expenditure Thyroid hormones directly regulate your body's metabolic rate. When thyroid function is impaired:
Your calorie burning decreases
Weight gain becomes easier
Insulin sensitivity declines
Metabolic syndrome risk increases
2. Mitochondrial Function Thyroid hormones are essential for healthy mitochondrial function—the cellular "power plants" that burn glucose for energy. Impaired thyroid function leads to:
Reduced cellular energy production
Decreased glucose utilization
Accumulation of abdominal fat
Worsening of insulin resistance
3. Inflammation and Autoimmunity Many thyroid disorders involve autoimmune inflammation, which directly contributes to:
Chronic low-grade inflammation
Impaired insulin signaling
Metabolic endotoxemia (gut-derived inflammatory signals)
Accelerated insulin resistance development
4. Gut Microbiome Alterations Thyroid dysfunction alters the gut microbiome composition, which:
Increases intestinal permeability ("leaky gut")
Promotes metabolic endotoxemia
Worsens insulin sensitivity
Complicates weight management
The Bidirectional Relationship
It's crucial to understand that this relationship flows in both directions:
Thyroid dysfunction → causes insulin resistance
Insulin resistance → worsens thyroid disease and reduces medication effectiveness
This bidirectional nature means that treating one condition without addressing the other leaves patients at a disadvantage.
Who's at Risk? Understanding Your Vulnerability
High-Risk Groups
1. Women Over 50 Postmenopausal women experience higher rates of both thyroid dysfunction and insulin resistance due to:
Declining estrogen levels
Changes in body composition
Increased metabolic syndrome prevalence
2. People with Type 2 Diabetes If you have diabetes, your risk of thyroid disease is 2-3 times higher than the general population.
3. Individuals with Obesity Obesity is both a risk factor for and consequence of the thyroid-insulin connection.
4. Those with Family History Both thyroid disease and insulin resistance run in families, suggesting genetic predisposition.
5. People with Autoimmune Conditions Having one autoimmune disease increases risk for others, including autoimmune thyroid disease.
6. Certain Ethnic Groups Research by Sharma et al. (2025) suggests some populations have higher prevalence, though universal screening is warranted.
Red Flags: When to Get Checked
Thyroid Dysfunction Symptoms
Unexplained weight gain despite diet efforts?
Persistent fatigue and low energy?
Hair loss or brittle hair?
Cold intolerance and low body temperature?
Brain fog or memory problems?
Depression or mood changes?
Dry skin and sluggish digestion?
Insulin Resistance Warning Signs
Difficulty losing weight, especially around the abdomen
Constant sugar cravings
Afternoon energy crashes
Dark skin patches (acanthosis nigricans)
High blood pressure
Elevated triglycerides
Polycystic ovary syndrome (PCOS) in women
If you experience multiple signs from both categories, discussing comprehensive metabolic screening with your healthcare provider becomes urgent.
Diagnostic Approaches: What Your Doctor Should Check
Essential Thyroid Tests
TSH (thyroid-stimulating hormone)
Free T4 and Free T3
Thyroid peroxidase (TPO) antibodies
Thyroglobulin antibodies
Insulin Resistance Assessments
HOMA-IR (Homeostatic Model Assessment for Insulin Resistance)
METS-IR (Metabolic Score for Insulin Resistance)—the more sophisticated measure
HbA1c (average blood sugar)
Lipid panel (triglycerides, cholesterol)
Metabolic syndrome screening
Why Both Matter
The research presented above emphasizes that checking only one system is insufficient. Comprehensive health management requires evaluating both thyroid function and metabolic status simultaneously.
Gender Gap
Women are diagnosed with thyroid disorders at a rate of 1 in 8, significantly higher than men. In the context of diabetes, this makes thyroid screening a mandatory "Level 1" priority for female patients.
Treatment Strategies: Integrated Approaches
Medical Management
For Thyroid Dysfunction:
Levothyroxine (synthetic T4) remains first-line therapy
Dose optimization based on TSH and symptom response
Some patients benefit from combination therapy with T3
Regular monitoring and adjustment
For Insulin Resistance:
Metformin addresses both glucose metabolism and insulin sensitivity
GLP-1 receptor agonists for prediabetes and diabetes
SGLT2 inhibitors for cardiovascular protection
Other agents based on individual risk factors
Lifestyle Interventions
Nutrition Strategies:
An anti-inflammatory diet reducing processed foods
Adequate protein (25-30% of calories) to support metabolic function
Complex carbohydrates over refined sugars
Sufficient selenium and zinc for thyroid function
Adequate omega-3 fatty acids for anti-inflammatory effects
Physical Activity:
Resistance training improves insulin sensitivity and metabolic rate
Aerobic exercise supports metabolic health
Consistency matters more than intensity
Aim for 150 minutes of moderate activity weekly
Stress Management:
Chronic stress worsens both thyroid dysfunction and insulin resistance
Cortisol elevation directly impairs metabolic function
Meditation, yoga, and sleep optimization are evidence-based
Sleep Optimization:
Poor sleep quality and sleep deprivation worsen insulin resistance
Target 7-9 hours nightly
Maintain consistent sleep schedules
FAQs: Your Questions Answered
Q1: Can thyroid disease cause weight gain even with a healthy diet?
A: Absolutely. Thyroid hormones directly regulate metabolic rate. Untreated hypothyroidism can reduce calorie burning by 30-40%, making weight gain inevitable regardless of diet. This is biology, not willpower failure.
Q2: Do I need thyroid screening if I have diabetes?
A: Yes. The research strongly supports universal thyroid screening in diabetic populations. Early detection allows for intervention before metabolic complications worsen.
Q3: Can treating thyroid disease improve blood sugar control?
A: Yes, according to Suganya et al. (2025), optimizing thyroid function improves glycemic control and can reduce medication requirements in some patients.
Q4: Is the METS-IR better than HOMA-IR for assessing insulin resistance?
A: Both are useful, but METS-IR (as highlighted by Safari et al.) incorporates additional metabolic parameters, providing a more comprehensive assessment. Ask your doctor which they use.
Q5: Can insulin resistance cause thyroid disease?
A: The relationship is bidirectional. While insulin resistance doesn't directly cause thyroid disease, it worsens existing thyroid dysfunction and impairs thyroid hormone effectiveness.
Q6: Are there natural ways to improve both thyroid and insulin sensitivity?
A: Diet and exercise significantly help, particularly resistance training and anti-inflammatory nutrition. However, medical treatment is often necessary. Discuss integrating both approaches with your provider.
Q7: Why do some people with thyroid disease still struggle with weight despite treatment?
A: Unaddressed insulin resistance is a common culprit. Treating the thyroid alone without addressing metabolic dysfunction leaves a critical piece of the puzzle untreated.
Q8: Is the connection between thyroid disease and diabetes universal across all populations?
A: Yes, according to Sharma et al. (2025), the association appears across diverse geographic regions and ethnic groups, though prevalence rates may vary.
Q9: How often should thyroid and metabolic markers be checked?
A: At minimum annually if you have diabetes, prediabetes, or thyroid disease. More frequent monitoring (every 6-8 weeks) may be warranted during dose adjustments or lifestyle interventions.
Q10: Can thyroid cancer patients benefit from managing insulin resistance?
A: According to Iuliano et al. (2025), yes—managing metabolic health may improve outcomes in thyroid cancer patients and deserves serious consideration.
Key Takeaways: What You Need to Remember
Thyroid dysfunction and insulin resistance are interconnected conditions that frequently occur together, creating a "double hit" to metabolic health.
Recent 2025 research confirms that the thyroid-metabolic connection is significant, bidirectional, and deserving of serious clinical attention.
If you have diabetes, prediabetes, or thyroid disease, comprehensive screening for the other condition is clinically justified.
Sophisticated assessments like METS-IR provide better insight into metabolic health than basic glucose and insulin testing.
Thyroid disorders significantly complicate diabetes management, making thyroid optimization essential for glycemic control.
Treatment requires an integrated approach combining medical management, nutrition, exercise, stress reduction, and sleep optimization.
The relationship works both directions—untreated thyroid dysfunction sabotages diabetes management, and vice versa.
Geographic and ethnic diversity of affected populations suggests this is a universal health challenge, not isolated to specific groups.
Early detection and integrated treatment offer opportunities for better outcomes and quality of life.
Your healthcare provider should evaluate both systems simultaneously rather than in isolation.
Call to Action: Take Control of Your Metabolic Health
If You Have Thyroid Disease:
Request comprehensive metabolic screening including fasting glucose, insulin, HbA1c, METS-IR if available, and a lipid panel. Don't assume your thyroid treatment is sufficient without addressing potential insulin resistance.
If You Have Diabetes or Prediabetes:
Ask your doctor for a comprehensive thyroid panel including TSH, Free T4, and thyroid antibodies. Managing thyroid dysfunction could be the missing piece in your blood sugar control efforts.
For Everyone:
Schedule a preventive health assessment if you have a family history of diabetes or thyroid disease
Evaluate your stress levels, sleep quality, and physical activity—these dramatically impact both systems
Consider working with healthcare providers experienced in metabolic medicine and endocrinology
Ask specifically about insulin resistance assessment and thyroid optimization, not just basic screening
Next Steps:
Schedule an appointment with your primary care provider or endocrinologist
Bring this information—awareness drives better clinical decision-making
Request appropriate testing if not recently completed
Discuss integrated treatment strategies addressing both systems
Commit to lifestyle modifications that support both thyroid and metabolic health
Remember: Your health is interconnected. Treating one system in isolation leaves you operating at a disadvantage. By understanding and addressing the thyroid-insulin resistance connection, you're taking control of your long-term health and wellbeing.
Author’s Note
As a physician and researcher deeply engaged in the study of metabolic disorders, my goal in writing this article is to bridge the gap between cutting-edge scientific evidence and practical clinical understanding. Thyroid dysfunction and insulin resistance are often treated as separate conditions in routine medical practice, yet emerging research from 2024–2026 consistently shows that they are tightly interconnected and frequently coexist long before a formal diagnosis is made.
Too many patients struggle for years with unresolved symptoms—fatigue, weight gain, brain fog, fluctuating blood sugar—while the underlying metabolic drivers remain misdiagnosed or untreated. This article was written to highlight the bidirectional nature of this relationship, empowering both patients and clinicians to take a more comprehensive and proactive approach to testing, management, and long-term prevention.
By synthesizing the latest peer-reviewed studies with real-world clinical insights, my intention is to provide a clear, evidence-based roadmap that can help improve metabolic health outcomes. I hope this work encourages healthcare professionals to broaden their diagnostic perspective and inspires individuals to understand their conditions more holistically.
Your metabolic health is not determined by a single hormone or lab value—it is the result of a finely tuned, interconnected system. Recognizing this is the first step toward meaningful and lasting change.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Individual circumstances vary, and treatment decisions should always be made in consultation with qualified healthcare professionals.
Related Articles
Feed Your Gut, Fuel Your Health: Diet, Microbiota, and Systemic Health | DR T S DIDWAL
What’s New in the 2025 Blood Pressure Guidelines? A Complete Scientific Breakdown | DR T S DIDWAL
Low-Fat vs. Low-Carb: Which Diet is Best for Weight Loss? | DR T S DIDWAL
5 Steps to Reverse Metabolic Syndrome: Diet, Habit, & Lifestyle Plan | DR T S DIDWAL
The Role of Cholesterol in Health and Disease: Beyond the "Bad" Label | DR T S DIDWAL
Lowering Cholesterol with Food: 4 Phases of Dietary Dyslipidemia Treatment | DR T S DIDWAL
High Triglyceride Levels: 5 New Facts to Help You Lower Your Risk | DR T S DIDWAL
The Best Dietary Fat Balance for Insulin Sensitivity, Inflammation, and Longevity | DR T S DIDWA
References
Iuliano, S., Mirabelli, M., Giuliano, S., & Brunetti, A. (2025). Insulin resistance and metabolic dysfunction in thyroid nodules and differentiated thyroid cancer. Current Opinion in Oncology. https://doi.org/10.1097/CCO.0000000000001202
Krishnamurthy, H., Suresh, C., Siriwardhane, T., Krishna, K., Song, Q., Jayaraman, V., Wang, T., Bei, K., & Rajasekaran, J. J. (2025). Association between thyroid dysfunction and insulin resistance: a retrospective cohort study. BMJ Open, 15(1), e076397. https://doi.org/10.1136/bmjopen-2023-076397
Razvi, S. (2026). The public health burden of diabetes mellitus and thyroid disease: Twin epidemics. Nature Reviews Endocrinology. https://doi.org/10.1038/s41574-025-01226-5
Safari, F., Nabavizadeh, A., & Vardanjani, H. M. (2024). The association between thyroid function and insulin resistance as measured by the metabolic score for insulin resistance (METS-IR): Insights from NHANES 2007–2012. BMC Endocrine Disorders, 24, 267. https://doi.org/10.1186/s12902-024-01779-y
Sharma, B., Chaudhary, V., Kumari, S., & Pal, B. (2025). Prevalence of thyroid disorders in patients with diabetes and hypertension in India: A systematic review and meta-analysis. Obesity Medicine, 55, 100609. https://doi.org/10.1016/j.obmed.2025.100609
Suganya, V., Bathena, A. K., & Ponambalaganapathi, A. (2025). A cross-sectional study on impact of thyroid disorders in type 2 diabetes mellitus. Romanian Medical Journal, 72(2), Article 10. https://doi.org/10.37897/RMJ.2025.2.10