Can You Reverse Diabesity? A 6-Step Plan to Improve Weight, Blood Sugar, and Metabolic Health
Diabesity reflects shared metabolic dysfunction between obesity and type 2 diabetes. Explore a 6-step, evidence-based strategy to improve weight and glycemic control.
DIABETESOBESITY
Dr. T.S. Didwal, M.D.(Internal Medicine)
1/28/202613 min read
What if the two most powerful drivers of modern chronic disease were not separate epidemics—but a single disorder expressed through two intertwined pathways?
Across healthcare systems worldwide, clinicians are witnessing a familiar trajectory: progressive weight gain, rising fasting glucose, expanding waistlines, escalating medication lists—and yet worsening metabolic health. Traditionally, obesity and type 2 diabetes mellitus have been treated as distinct clinical entities. Contemporary research, however, challenges this fragmented view. A growing body of evidence now recognizes these conditions as biologically interconnected manifestations of a unified metabolic disorder known as diabesity (Nobre & Esteves, 2025; Galasso et al., 2026).
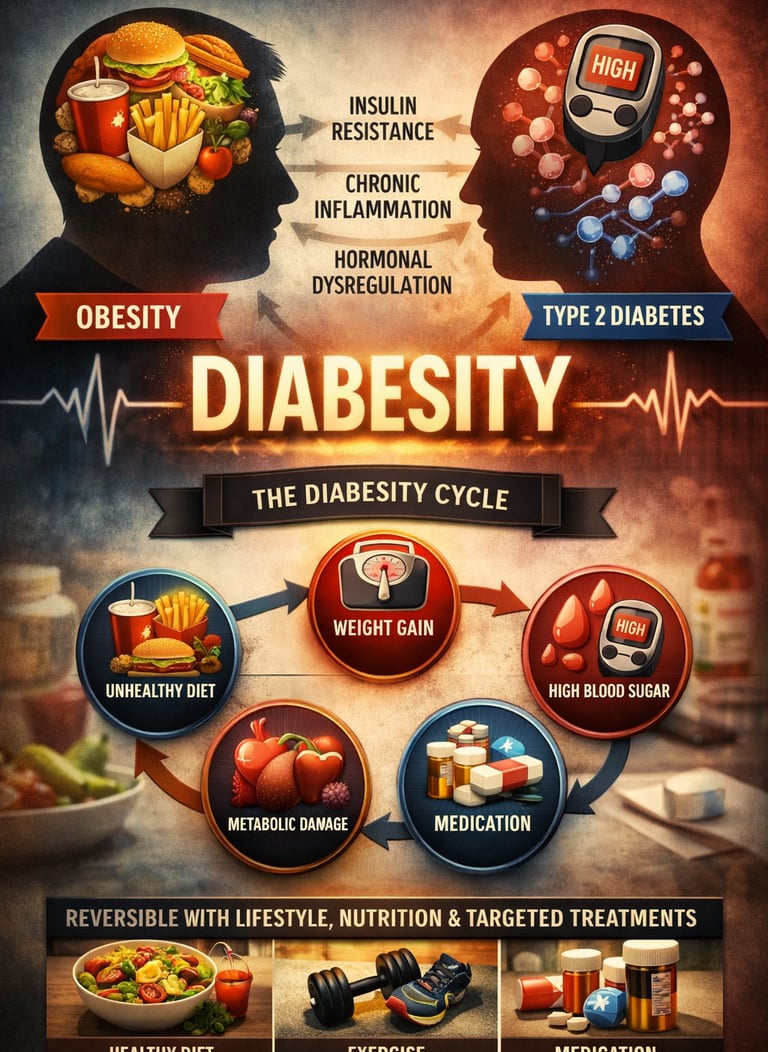
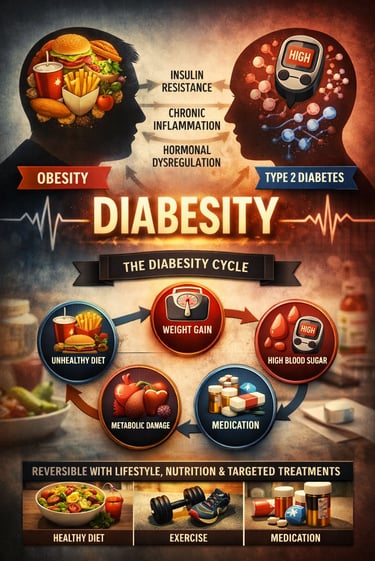
Diabesity is driven by shared pathophysiological mechanisms, including insulin resistance, visceral adiposity, chronic low-grade inflammation, and hormonal dysregulation, all of which reinforce one another in a vicious metabolic cycle (Chai et al., 2025). Crucially, diabesity is not a consequence of individual failure or lack of discipline. Rather, it reflects a predictable physiological response to a modern environment characterized by ultra-processed diets, physical inactivity, chronic stress, sleep disruption, and circadian misalignment (Bizimana, 2024).
The clinical consequences are profound. Long before diagnostic thresholds for diabetes are reached, diabesity accelerates vascular dysfunction, hepatic steatosis, renal injury, and cardiovascular disease, silently increasing long-term morbidity and mortality (Bajaj et al., 2025). By the time hyperglycemia meets formal diagnostic criteria, metabolic injury has often been evolving for years.
Encouragingly, diabesity is not inevitable nor irreversible. High-quality randomized trials and guideline-based evidence demonstrate that targeted lifestyle interventions, nutritional pattern modification, and—when indicated—modern pharmacologic therapies can prevent disease progression, restore normoglycemia in prediabetes, promote sustainable weight reduction, and significantly lower cardiometabolic risk (Chai et al., 2025; Galasso et al., 2026; Bajaj et al., 2025). Recognizing diabesity as a unified condition fundamentally reshapes prevention and treatment strategies—and opens a critical window for early, effective intervention.
Clinical pearls
1. The "Phenotype" Pivot: One Size Does Not Fit All
Prediabetes is a heterogeneous condition. Pathophysiology varies—some patients have impaired fasting glucose (hepatic insulin resistance), while others have impaired glucose tolerance (muscle insulin resistance).
Not everyone’s prediabetes is the same. Your body might struggle with sugar in the morning, while someone else’s struggles after a meal. This means your "best" diet or workout might look different from a friend's. Personalised plans beat generic advice.
2. The 5-10% Threshold: Small Losses, Massive Wins
Clinical trials show a non-linear relationship between weight loss and metabolic improvement. A 5-10% reduction in total body weight can lead to a disproportionate ~50-60% reduction in T2D progression.
You don’t need to reach your "high school weight" to be healthy. Losing just 5 to 10 pounds for every 100 pounds you weigh is often the "magic number" that resets your internal chemistry and protects your heart.
3. Muscle as a Metabolic Sink
Skeletal muscle is responsible for over 80% of postprandial glucose disposal. Resistance training increases GLUT4 translocation, improving insulin sensitivity independently of adipose tissue loss.
Think of your muscles as a "sponge" for sugar. The more muscle you have (and the more you use it), the more sugar your body can soak up out of your blood. Lifting weights is just as important as going for a walk.
4. "Metabolic Legacy": The Value of Early Intervention
The "Legacy Effect" or "Metabolic Memory" suggests that early glycemic control provides long-term protection against microvascular complications, even if glycemic control later in life fluctuates.
Managing your blood sugar now pays "interest" for decades. By taking action during the prediabetes stage, you are effectively "shielding" your eyes, kidneys, and nerves from damage that would otherwise show up 20 years down the line.
5. Beyond the Scale: Cardiometabolic Protection
Modern pharmacotherapy (GLP-1 RAs and SGLT-2i) has shifted the goal from "glucocentric" (only lowering A1C) to "organoprotective" (reducing MACE and renal decline).
Modern medications do more than just lower a number on a lab test; they act like "bodyguards" for your heart and kidneys. Even if your weight or sugar doesn't drop as fast as you’d like, these treatments are often working behind the scenes to prevent heart attacks and kidney failure.
Diabesity Prevention and Management: The Complete Guide to Foods, Lifestyle, and Emerging Treatments
What Exactly is Diabesity? Defining the Condition
Diabesity combines the clinical features of both obesity and type 2 diabetes mellitus, creating a state where metabolic dysfunction operates at multiple levels simultaneously. Rather than treating weight gain and blood sugar dysregulation as separate problems, the diabesity framework acknowledges their common underlying mechanisms: insulin resistance, chronic inflammation, and impaired glucose metabolism.
Understanding this connection is crucial because addressing one component often positively impacts the other. This is why effective diabesity management requires simultaneous attention to diet, physical activity, weight management, and—when necessary—pharmacological interventions.
Study 1: Editorial on Foods, Diet, and Dietary Patterns in Diabesity Prevention
This editorial by Nobre & Esteves (2025) emphasizes a paradigm shift: rather than focusing narrowly on calorie restriction, modern diabesity prevention prioritizes the quality and composition of foods consumed. The research underscores that dietary patterns—the habitual way people combine different foods—matter more than individual nutrients in isolation.
The editorial highlights that ultra-processed foods, high in refined carbohydrates and unhealthy fats, actively promote the metabolic dysfunction underlying diabesity, while whole food-based diets rich in fiber, plant compounds, and natural nutrients support metabolic health and sustainable weight management.
Key Takeaways
Whole foods matter more than calories: Focus on minimally processed foods rather than calorie counting
Dietary patterns are preventive: Consistent eating patterns reduce type 2 diabetes risk more effectively than sporadic diet changes
Individual foods have secondary importance: The overall dietary pattern determines long-term success
Nutrient density trumps energy density: Foods with high nutritional value relative to calorie content support better health outcomes
Consider adopting a Mediterranean-style pattern emphasizing vegetables, legumes, whole grains, nuts, and quality olive oil, or a DASH diet (Dietary Approaches to Stop Hypertension) pattern proven to lower blood pressure and improve insulin sensitivity.
Study 2: Lifestyle Modifications for Type 2 Diabetes Prevention and Management
Bizimana's comprehensive review demonstrates that lifestyle modifications—encompassing diet, physical activity, weight reduction, and stress management—represent the most cost-effective, evidence-based approach to type 2 diabetes prevention. The research provides quantifiable evidence that even modest lifestyle changes produce measurable improvements in glycemic control and metabolic markers.
The study confirms that individuals with prediabetes who implement lifestyle modifications have approximately 58% reduced risk of progressing to clinical type 2 diabetes compared to control groups. These benefits emerge within 3-6 months, providing rapid feedback that motivates continued adherence.
Key Takeaways
Modest weight loss (5-10%) yields significant metabolic benefits: Complete weight normalization isn't necessary for health improvements
Physical activity independently reduces diabetes risk: Exercise benefits metabolism regardless of weight loss
Behavior change is sustainable when incremental: Small, progressive modifications show better long-term adherence than drastic changes
Early intervention in prediabetes is critical: Prevention is dramatically more effective than managing established diabetes
Multifactorial approaches outperform single interventions: Combining diet, exercise, and behavioral support produces superior outcomes
Aim for 150 minutes of moderate-intensity physical activity weekly (30 minutes, 5 days per week), combined with resistance training 2-3 times weekly. Simultaneously, increase vegetable consumption, reduce refined carbohydrate intake, and establish regular meal timing to stabilize blood sugar throughout the day.
Study 3: Special Issue on Lifestyle and Supplements for Diabetes Prevention and Control
This special issue collection iin the Journal of Diabetes Research. (2025). synthesizes multiple studies examining both lifestyle interventions and supplemental approaches to diabetes prevention and management. The research indicates that while lifestyle modifications remain the cornerstone of treatment, certain supplements may offer adjunctive benefits when combined with evidence-based lifestyle strategies.
The special issue highlights that micronutrient status, including deficiency in chromium, magnesium, and vitamin D, correlates with increased type 2 diabetes risk. Strategic supplementation in deficient individuals may enhance the metabolic benefits of lifestyle modification.
Key Takeaways
Lifestyle interventions are foundational: No supplement replaces diet and exercise
Targeted supplementation has modest benefits: Certain supplements may accelerate metabolic improvements in deficient individuals
Nutrient status should be assessed: Blood work identifying vitamin D deficiency, magnesium deficiency, or micronutrient insufficiencies informs supplementation decisions
Supplement quality varies: Choose products third-party tested for purity and potency
Whole foods remain superior to supplements: Obtaining nutrients from food sources provides additional beneficial compounds beyond single nutrients
Rather than indiscriminate supplementation, work with your healthcare provider to identify specific micronutrient deficiencies through blood work. If deficient in magnesium (approximately 45% of adults), consider increasing intake through pumpkin seeds, leafy greens, and almonds, supplementing only if dietary changes prove insufficient.
Study 4: Pharmacological Management of Diabesity—Current and Emerging Therapies
The comprehensive analysis by Galasso et al. (2026) examines pharmacological approaches to diabesity management, documenting both established medications and emerging treatments. The research emphasizes that while lifestyle modification remains primary, pharmacotherapy plays an essential role—particularly for individuals unable to achieve sufficient weight loss or glycemic control through lifestyle changes alone.
The study highlights newer GLP-1 receptor agonists (like semaglutide) and SGLT-2 inhibitors that demonstrate dual benefits for both glucose control and weight reduction, addressing the interconnected nature of diabesity. These agents represent a shift toward medications specifically designed to impact both metabolic dimensions of this condition.
Key Takeaways
Pharmacotherapy complements, not replaces, lifestyle changes: Medications work best combined with diet and exercise modification
GLP-1 receptor agonists provide dual benefits: They improve glycemic control while promoting weight loss through appetite suppression
SGLT-2 inhibitors offer metabolic advantages: Beyond glucose control, they provide cardiovascular protection and renal preservation
Newer agents demonstrate superiority: Contemporary pharmacological agents outperform older medications in efficacy and side effect profiles
Individualized therapy is essential: Treatment selection depends on patient characteristics, comorbidities, and treatment goals
If lifestyle modifications alone prove insufficient after 3-6 months of consistent adherence, discuss pharmacological options with your provider. For individuals with heart disease or chronic kidney disease, SGLT-2 inhibitors may offer particular benefits. For those struggling with weight loss, GLP-1 receptor agonists represent an evidence-based option that addresses both components of diabesity.
Study 5: Standards of Care in Diabetes—Pharmacologic Approaches to Glycemic Treatment
The American Diabetes Association's authoritative standards of care (Bajaj et al., 2025) provide comprehensive, evidence-based guidance on pharmacological management of diabetes mellitus. This comprehensive resource establishes that successful glycemic treatment requires individualized approaches considering patient age, kidney function, cardiovascular status, weight status, and hypoglycemia risk.
The standards emphasize a shift from glucose-centric treatment toward cardiometabolic risk reduction. Many newer medications benefit patients beyond simple blood glucose lowering, providing cardiovascular protection, weight reduction, or kidney disease prevention—all critical considerations in diabesity management.
Key Takeaways
Individualized treatment is essential: No single medication suits all patients; treatment selection depends on multiple patient factors
Cardiometabolic risk reduction is primary: Beyond lowering glucose, consider medications providing cardiovascular protection
Multiple medication classes address different pathways: Metformin, GLP-1 agonists, SGLT-2 inhibitors, DPP-4 inhibitors, and sulfonylureas work through distinct mechanisms
Combination therapy is often necessary: Most patients require multiple agents to achieve glycemic targets safely
Regular monitoring enables optimization: Blood work, A1C testing, and clinical assessment guide medication adjustments
Work with your healthcare provider to establish an individualized treatment plan that considers not only blood glucose control but also your cardiovascular health, kidney function, and weight management goals. Request A1C testing every 3 months until stable, then every 6 months—this provides objective feedback on medication effectiveness.
Study 6: Lifestyle Interventions and Prediabetes Phenotypes—Meta-Analysis of RCTs
This rigorous meta-analysis of randomized controlled trials by Chai et al. (2025) synthesizes evidence from multiple intervention studies, examining how lifestyle interventions prevent type 2 diabetes and—critically—enable reversion to normoglycemia (return to normal blood sugar levels). The research reveals that prediabetes isn't irreversible; substantial proportions of individuals can return to normal glucose regulation through sustained lifestyle modification.
The analysis highlights that effects vary by prediabetes phenotype—individuals with different presentations of prediabetic pathophysiology respond differently to interventions. This finding supports personalized approaches rather than one-size-fits-all strategies.
Key Takeaways
Prediabetes is reversible: 30-50% of individuals with prediabetes revert to normoglycemia with sustained lifestyle intervention over 2-3 years
Lifestyle interventions prevent diabetes: Lifestyle modification reduces type 2 diabetes incidence by approximately 58% compared to usual care
Heterogeneous responses exist: Prediabetes phenotypes predict intervention response; personalized approaches improve outcomes
Duration matters: Shorter interventions (<6 months) show modest benefits; sustained efforts (2+ years) demonstrate dramatic improvements
Combination approaches work best: Simultaneous dietary modification, physical activity, and behavioral support yield superior outcomes
If recently diagnosed with prediabetes, understand that you have a critical opportunity for prevention. With consistent adherence to lifestyle modifications for 2-3 years, many individuals completely reverse their prediabetes status. Focus on sustainable changes—finding an exercise you enjoy, gradually shifting your diet toward whole foods, and building supportive social structures around your health goals.
Synthesizing the Evidence: A Comprehensive Approach to Diabesity
The six studies presented above paint a clear picture: diabesity prevention and management require coordinated attention across multiple domains:
Dietary Foundation
Begin with whole food-based eating patterns emphasizing vegetables, legumes, whole grains, nuts, and quality fats. Mediterranean and DASH dietary patterns show particular promise. Minimize ultra-processed foods and refined carbohydrates. This isn't about perfection; gradual improvements in dietary patterns accumulate into substantial metabolic benefits.
Physical Activity Integration
Establish 150 minutes weekly of moderate-intensity aerobic activity combined with 2-3 weekly sessions of resistance training. This combination addresses both glucose control and metabolic health while supporting sustainable weight loss. Find activities you enjoy; adherence matters more than intensity for long-term success.
Micronutrient Optimization
Rather than indiscriminate supplementation, identify specific deficiencies through blood work. Prioritize whole food sources of magnesium, vitamin D, and chromium. Supplement strategically only when dietary changes prove insufficient.
Behavior Change Support
Sustainable improvement requires addressing eating patterns, stress management, sleep quality, and social support. Consider working with a registered dietitian, health coach, or therapist specializing in behavior change. Many individuals succeed better with structured support than attempting changes alone
.
Pharmacological Optimization (When Needed)
If lifestyle modifications alone prove insufficient after 3-6 months of consistent effort, discuss pharmacological options with your healthcare provider. Newer agents like GLP-1 receptor agonists and SGLT-2 inhibitors address both glucose control and weight reduction, directly targeting diabesity pathophysiology.
Regular Monitoring and Adjustment
Establish a monitoring schedule including A1C testing, fasting glucose, lipid panels, and blood pressure assessment. Regular monitoring provides objective feedback on strategy effectiveness and enables timely adjustments.
Frequently Asked Questions (FAQs)
Q: What's the difference between prediabetes and type 2 diabetes?
A: Prediabetes represents an intermediate state where blood sugar is elevated but not yet high enough for a type 2 diabetes diagnosis. Importantly, prediabetes is often reversible through lifestyle modification. Type 2 diabetes involves higher blood glucose levels and typically requires pharmacological intervention alongside lifestyle changes. Early intervention during the prediabetes stage prevents disease progression in many individuals.
Q: How quickly can I see results from lifestyle changes?
A: Metabolic improvements begin within weeks of consistent change. Insulin sensitivity improves within 2-4 weeks; blood pressure often decreases within 4-6 weeks; meaningful weight loss typically emerges within 6-8 weeks. However, prediabetes reversal and sustained weight management require 2-3 years of consistent effort. This extended timeline isn't discouraging—it reflects realistic physiology and supports lasting change over quick fixes.
Q: Do I need medications if I'm losing weight successfully?
A: This depends on your baseline metabolic status and treatment goals. Some individuals achieve excellent glycemic control through lifestyle modification alone. Others benefit from medications even while actively engaging in lifestyle changes. This decision should be made collaboratively with your healthcare provider considering your A1C levels, cardiovascular risk factors, and personal circumstances. Remember: medications complement, don't replace, lifestyle change.
Q: Which diet is best for diabesity?
A: Research supports multiple dietary patterns including Mediterranean, DASH, low-glycemic-load, and plant-based diets. The "best" diet is the one you can sustain long-term. Focus on whole foods, minimize ultra-processed foods, control portions, and emphasize vegetables, legumes, and quality proteins. Consistency with a sustainable approach surpasses perfection with an unsustainable one.
Q: How much exercise do I need?
A: The evidence-based recommendation is 150 minutes weekly of moderate-intensity aerobic activity (activities where you can talk but not sing), plus 2-3 sessions weekly of resistance training (weights, resistance bands, or bodyweight exercises). However, any increase in physical activity provides benefits. Begin where you are; progress gradually. Even 10 minutes of activity is better than none.
Q: Can supplements alone help with diabesity?
A: No. Supplements complement but cannot replace lifestyle modifications. While certain micronutrient supplements may modestly enhance metabolic function, they work best when combined with dietary improvement, physical activity, and behavior change. Avoid supplement-focused approaches to diabesity; instead, prioritize foundational lifestyle strategies.
Q: How often should I get blood work?
A: Until glycemic control is stable, obtain A1C testing every 3 months. Once stable, testing every 6 months is appropriate. Additionally, annual assessment should include lipid panels, liver function tests, kidney function tests, and blood pressure measurement. More frequent monitoring may be warranted during medication adjustments or when complications develop.
Q: Is weight loss necessary to prevent type 2 diabetes?
A: No, though modest weight loss (5-10%) provides significant metabolic benefits. The research clearly demonstrates that physical activity and dietary improvement reduce diabetes risk independent of weight change. However, weight loss typically accompanies sustained lifestyle modification and provides additional metabolic benefits beyond what either strategy achieves alone.
Key Takeaways: Your Action Plan
Start with dietary foundation: Shift gradually toward whole foods, minimizing ultra-processed foods and refined carbohydrates
Establish physical activity routine: Aim for 150 minutes weekly of moderate-intensity activity plus resistance training 2-3 times weekly
Identify and address micronutrient deficiencies: Work with your provider to assess nutritional status and supplement strategically
Seek behavioral support: Consider working with a registered dietitian, health coach, or therapist for structured change support
Discuss pharmacotherapy if needed: After 3-6 months of consistent lifestyle effort, discuss medications if metabolic goals remain unmet
Commit to regular monitoring: Establish a testing schedule and review results with your healthcare provider quarterly
Author’s Note
The concept of diabesity reflects a fundamental shift in how modern medicine understands metabolic disease. During years of clinical practice and engagement with contemporary research, it has become increasingly clear that obesity and type 2 diabetes are not isolated conditions, but deeply interconnected manifestations of shared metabolic dysfunction. Treating them separately often leads to incomplete care and missed opportunities for prevention.
This article was written with a singular goal: to bridge the gap between cutting-edge scientific evidence and practical, clinically meaningful guidance. Every recommendation presented here is grounded in peer-reviewed research, major international guidelines, and outcomes observed in real-world clinical settings. Wherever possible, emphasis has been placed on interventions that are sustainable, individualized, and respectful of human physiology rather than short-term fixes.
Equally important, this work aims to challenge the stigma often associated with metabolic disease. Diabesity is not a failure of willpower or character—it is a predictable biological response to modern environmental pressures acting on genetically susceptible individuals. Recognizing this reality allows both clinicians and patients to move away from blame and toward effective, compassionate care.
Finally, this guide is not intended to replace personalized medical advice, but to empower informed decision-making and productive dialogue between individuals and their healthcare providers. With early recognition, evidence-based intervention, and sustained support, diabesity can be prevented, reversed, or successfully managed—changing the trajectory of metabolic health for millions.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Individual circumstances vary, and treatment decisions should always be made in consultation with qualified healthcare professionals.
Related Articles
Managing Diabesity: A Complete Guide to Weight Loss and Blood Sugar Control | DR T S DIDWAL
Is Prediabetes Reversible? What the Latest 2025 Studies Reveal | DR T S DIDWAL
Stop the Clock: Proven Ways to Reverse Early Aging if You Have Diabetes | DR T S DIDWAL
Low-Fat vs. Low-Carb: Which Diet is Best for Weight Loss? | DR T S DIDWAL
5 Steps to Reverse Metabolic Syndrome: Diet, Habit, & Lifestyle Plan | DR T S DIDWAL
References
Bajaj, M., McCoy, R. G., Balapattabi, K., Bannuru, R. R., Bellini, N. J., Bennett, A. K., Beverly, E. A., Briggs Early, K., Challasivakanaka, S., Echouffo-Tcheugui, J. B., Everett, B. M., Rajesh, G., Laffel, L. M., Lal, R., Matfin, G., Nelson, A. B., Neumiller, J. J., Pandya, N., Pekas, E. J., Peters, A. L., Pilla, S. J., Romeo, G. R., Rosas, S. E., Sadhu, A. R., Segal, A. R., Simmons, K. M., Szmuilowicz, E. D., & Elsayed, N. A. (2025). 9. Pharmacologic approaches to glycemic treatment: Standards of care in diabetes—2026. Diabetes Care, 49(Supplement_1), S183–S215. https://doi.org/10.2337/dc26-S009
Bizimana, R. T. (2024). The impact of lifestyle modifications on type 2 diabetes prevention and management. IDOSR Journal of Biochemistry, Biotechnology and Allied Fields, 9(3), 18–24. https://doi.org/10.59298/IDOSR/JBBAF/24/93.1824000
Chai, X., Wang, Y., Yin, X., Gong, Q., Zhang, J., Shao, R., & Li, G. (2025). Effects of lifestyle interventions on the prevention of type 2 diabetes and reversion to normoglycemia by prediabetes phenotype: A systematic review and meta-analysis of randomized controlled trials. Diabetes & Metabolic Syndrome, 19(1), 103184. https://doi.org/10.1016/j.dsx.2025.103184
Galasso, M., Caporusso, M., Volatile, A., Verde, L., Esposito, K., Giorgino, F., Perrini, S., Colao, A., Barrea, L., Muscogiuri, G., & Obesity Programs of nutrition, Education, Research and Assessment (OPERA) Group (2026). Pharmacological management of diabesity: Current and emerging therapies. Current Obesity Reports, 15(1), 5. https://doi.org/10.1007/s13679-025-00681-5
Journal of Diabetes Research. (2025). Special issue: Lifestyle and supplements for prevention and control of diabetes mellitus [Special issue]. Journal of Diabetes Research, 2025(1485.si.997434). https://doi.org/10.1155/1485.si.997434
Nobre, L. N., & Esteves, E. A. (2025). Editorial: The role of foods, diet, and dietary patterns in the prevention and management of diabesity. Frontiers in Nutrition, 12, 1632666. https://doi.org/10.3389/fnut.2025.1632666