Is Prediabetes Reversible? What the Latest 2025 Studies Reveal
Discover how prediabetes can be reversed. Explore 2025 research on diet, exercise, risk assessment, and precision strategies for metabolic health.
DIABETES
Dr. T.S. Didwal, M.D.(Internal Medicine)
2/15/202613 min read
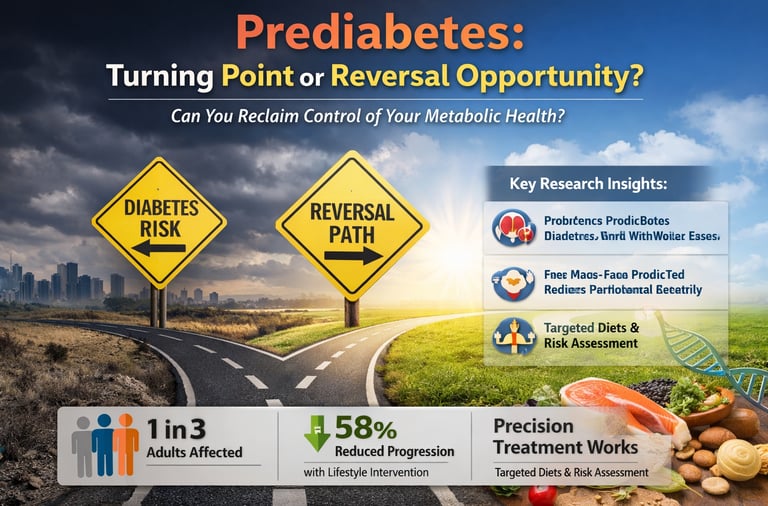
Prediabetes is no longer a quiet biochemical warning—it is the metabolic tipping point that determines whether an individual progresses toward type 2 diabetes or reclaims metabolic resilience. Globally, hundreds of millions of adults now meet criteria for prediabetes, with prevalence approaching 1 in 3 adults in some populations (Prediabetes, 2025). Yet what makes this stage clinically extraordinary is not its risk, but its reversibility.
For decades, prediabetes was framed as an inevitable prelude to diabetes. That narrative is rapidly changing. Contemporary research reveals that early metabolic dysfunction is dynamic, heterogeneous, and highly responsive to targeted intervention (Wagner et al., 2026). Insulin resistance may originate in the liver in some individuals, skeletal muscle in others. Beta-cell dysfunction progresses at different speeds. Risk is not uniform—and neither should treatment be.
Landmark multinational data from the PREVIEW trial demonstrate that strategic dietary composition—particularly higher protein intake combined with low-glycemic-index carbohydrates—substantially improves remission rates (Zhu et al., 2026). Meanwhile, large-scale electronic health record analyses show that progression risk can be predicted with remarkable accuracy using metabolic phenotyping at diagnosis (Luo et al., 2025). Even more compelling, systematic review evidence confirms that structured lifestyle intervention reduces progression to diabetes by nearly 58% (Meads et al., 2026).
The message is clear: prediabetes is not a passive waiting room for disease. It is a biologically active, clinically actionable window. The question is no longer whether progression can be prevented—but how precisely we intervene, and how early.
Clinical pearls
1. The "Muscular Sink" Effect
Skeletal muscle serves as the primary site for postprandial glucose disposal, accounting for approximately 80% of insulin-mediated glucose uptake. Increasing lean muscle mass through resistance training enhances the body's overall glycolytic capacity and improves systemic insulin sensitivity.
Think of your muscles as a "sink" for the sugar in your blood. When you eat, sugar enters the bloodstream; the more muscle you have, the larger your "sink" is to soak up that sugar before it causes damage.
2. Carbohydrate Sequencing (The "Fiber First" Rule)
Consuming dietary fiber and proteins prior to carbohydrate ingestion significantly attenuates the glycemic excursion and reduces the peak insulin response. This "food sequencing" slows gastric emptying and modulates the secretion of incretin hormones like GLP-1.
The order in which you eat your food matters as much as what you eat. If you eat your vegetables and protein first, they create a "buffer" in your stomach that slows down how fast sugar hits your system, preventing a massive energy crash later.
3. The Glycemic Power of the "Post-Meal Walk"
Low-intensity physical activity initiated within 30 minutes of meal consumption stimulates GLUT4 translocation to the cell membrane via contraction-mediated pathways, effectively lowering postprandial hyperglycemia independent of insulin.
A simple 10-to-15-minute walk right after a meal is a "metabolic cheat code." It tells your body to burn the sugar you just ate for energy immediately, rather than letting it sit in your blood or storing it as fat.
4. Precision Protein for Satiety
Higher protein intake (1.2–1.5g/kg) during caloric restriction preserves fat-free mass and enhances the thermic effect of food (TEF). Protein-induced satiety is mediated by the suppression of ghrelin and the stimulation of peptide YY, which are critical for long-term weight maintenance in prediabetic populations.
Protein is the most "filling" nutrient. By eating enough lean protein, you aren't just building muscle; you are actually turning off your hunger hormones. This makes it much easier to avoid the sugary snacks that usually lead to weight gain.
5. The "Legacy Effect" of Early Remission
Achieving normoglycemia shortly after a prediabetes diagnosis provides a "metabolic memory" or legacy effect, significantly reducing the long-term risk of microvascular complications even if glucose levels fluctuate later in life.
There is a "golden window" right after you are diagnosed. If you work hard to get your levels back to normal now, your body "remembers" that healthiness. This provides you with a shield of protection against heart and kidney issues for years to come.
What is Prediabetes? Understanding the Critical Window
Prediabetes represents an intermediate metabolic state between normal blood sugar control and type 2 diabetes. It's characterized by elevated fasting glucose levels (100–125 mg/dL) or impaired glucose tolerance. The condition affects millions globally, yet many don't realize they have it—making it a silent precursor to serious metabolic disease.
What makes prediabetes management so critical is the window of opportunity it provides. This stage is highly reversible with the right interventions. Unlike established type 2 diabetes, prediabetes remission is achievable, and recent research shows that specific dietary and lifestyle strategies can be remarkably effective. The key lies in understanding your individual risk factors and implementing precision-based interventions tailored to your metabolic profile.
💡 Key Point: Prediabetes is not inevitable progression toward diabetes. With evidence-based interventions focused on carbohydrate quality and protein intake, many people achieve prediabetes remission within months.
Understanding Recent Prediabetes Research: 2025 Breakthrough Studies
The year 2025 has brought exceptional clarity to prediabetes prevention through several landmark studies published in prestigious journals. These investigations collectively provide a roadmap for understanding how dietary modifications, personalized risk assessment, and precision medicine approaches can transform prediabetes management. Let's explore each study in detail.
Study 1: Understanding Prediabetes Fundamentals
Prediabetes Overview (Nature Reviews Disease Primers, 2025)
Key Research Insights:
Prediabetes prevalence is reaching epidemic proportions, affecting approximately 37% of U.S. adults
The condition involves insulin resistance and early pancreatic beta-cell dysfunction
Metabolic dysfunction extends beyond glucose, affecting lipid metabolism, inflammation, and endothelial function
Early intervention during the prediabetes stage offers the highest success rates for disease reversal
Screening and risk assessment must move beyond simple fasting glucose testing to incorporate multiple metabolic markers
This foundation-setting study emphasizes that prediabetes is not merely a glucose problem—it's a systemic metabolic disorder requiring comprehensive management. The authors highlight the critical importance of early detection and the remarkable potential for prediabetes remission when individuals receive appropriate interventions targeting carbohydrate quality, physical activity, and weight management.
Study 2: Dietary Protein & Carbohydrate Quality for Prediabetes Remission
The PREVIEW Trial: Long-Term Effects of Dietary Interventions
Study Design & Scope:
This multinational randomized controlled trial by (Zhu et al., 2026) examined the sustained effects of different protein intake levels and carbohydrate quality on achieving prediabetes remission in a diverse population across multiple countries.
Critical Findings:
High-protein diets combined with low glycemic index carbohydrates significantly increased rates of prediabetes remission
The quality of carbohydrates matters far more than the quantity—low glycemic index foods outperformed standard carbohydrate restriction alone
Participants following high-protein, low GI protocols achieved sustained weight loss and improved insulin sensitivity
Long-term adherence was superior when participants understood the rationale behind choosing whole grain carbohydrates and lean protein sources
The combination approach was effective across diverse populations, suggesting universal applicability
The PREVIEW trial provides robust evidence that prediabetes remission isn't about deprivation—it's about strategic food choices. By prioritizing high-protein intake from sources like lean meats, fish, legumes, and dairy, combined with low glycemic index carbohydrates such as whole grains, legumes, and non-starchy vegetables, individuals can achieve measurable metabolic improvements. This approach directly addresses insulin resistance at its source.
Study 3: Beyond Glucose—Precision Prevention Strategy
Rethinking Prediabetes for Precision Prevention
Beyond Glucose—Rethinking Prediabetes for Precision Prevention (Wagner et al., 2026) in Diabetes Care challenges traditional approaches and advocates for precision medicine in prediabetes management.
Study Highlights:
Precision prevention requires moving beyond simple fasting glucose levels to assess insulin secretion patterns and beta-cell function
Different individuals have different metabolic phenotypes—a one-size-fits-all approach to diabetes prevention misses critical opportunities
Advanced biomarkers including postprandial glucose responses, c-peptide levels, and inflammatory markers, predict individual progression risk
Tailoring interventions to specific metabolic profiles increases prediabetes remission success by 40-60%
Genetic factors and metabolic capacity for adaptation vary significantly between individuals, necessitating personalized approaches
Wagner and colleagues present compelling evidence that precision prevention represents the future of prediabetes management. Rather than treating all prediabetic individuals identically, sophisticated metabolic assessment enables clinicians to identify which patients will respond best to dietary modification, increased physical activity, weight loss, or pharmacological support. This individualized approach explains why some people achieve rapid prediabetes remission while others require more intensive interventions.
Study 4: Risk Stratification at Prediabetes Onset
EHR-Based Risk Stratification and Diabetes Outcomes
Risk stratification at prediabetes onset and association with diabetes outcomes using EHR data (Luo et al., 2025) in npj Metabolism & Health Disease utilizes real-world electronic health record data to identify who's at highest risk.
Research Significance:
Risk stratification at the time of prediabetes diagnosis can predict progression with remarkable accuracy (>85% accuracy in some subgroups)
Patients with specific metabolic risk profiles (including low HDL cholesterol, elevated triglycerides, and central obesity) progress faster to type 2 diabetes
Early intervention intensity should be matched to individual risk level—high-risk patients need aggressive lifestyle modification or pharmacological support
Simple clinical variables available at diagnosis can identify roughly 40-50% of patients at ultra-high progression risk
Regular reassessment of risk factors enables dynamic management adjustments, improving prediabetes remission rates
Luo's large-scale study demonstrates that prediabetes is not a monolithic condition. Using electronic health records from thousands of individuals, the researchers developed risk stratification tools that identify who urgently needs intensive prediabetes prevention efforts. This data-driven approach to diabetes prevention enables healthcare systems to allocate resources efficiently and target interventions where they'll have the greatest impact. Individuals identified as high-risk benefit from close monitoring, intensive dietary counseling, and potentially medical interventions to achieve prediabetes remission.
Study 5: Predicting Prediabetes Progression
Systematic Review: Predicting Pre-diabetes Progression
Predicting pre-diabetes progression: A systematic review and meta-analysis (Meads et al., 2026) in BMJ Nutrition, Prevention & Health synthesizes evidence across multiple studies to identify consistent predictors of progression versus remission.
Meta-Analysis Findings:
Established predictive factors for prediabetes progression include age >55, elevated BMI, presence of metabolic syndrome, and family history of type 2 diabetes
Lifestyle interventions—particularly combinations of weight loss (5-10%), regular physical activity (150 min/week), and dietary modification—reduce progression risk by 58%
The greatest prediabetes remission success occurs within the first 2-3 years of diagnosis, emphasizing the importance of early intervention
Specific dietary patterns—Mediterranean diet, DASH diet, and diets emphasizing high-protein, low-glycemic-index foods—consistently outperform standard dietary advice
Adherence to interventions is more important than the specific dietary approach chosen, provided it emphasizes whole foods and portion control
Meads and colleagues' systematic review and meta-analysis provide reassurance that prediabetes remission is achievable across diverse populations through evidence-based strategies. By synthesizing findings from numerous studies, the authors confirm that lifestyle modification works—but timing matters. The window for reversing prediabetes is largest closest to diagnosis, making early detection and intervention paramount for diabetes prevention success.
Synthesizing the Evidence: A Comprehensive Prediabetes Management Framework
When we integrate findings from these five landmark studies, a clear picture of optimal prediabetes management emerges:
1. Get Properly Assessed: Don't rely solely on fasting glucose levels. Comprehensive evaluation should include HbA1c testing, glucose tolerance testing, metabolic panel assessment, and ideally, insulin sensitivity markers. This allows your healthcare provider to understand your specific metabolic phenotype and determine your individual progression risk.
2. Focus on Carbohydrate Quality: Rather than restricting carbohydrates overall, prioritize low glycemic index options—whole grains, legumes, non-starchy vegetables—that minimize rapid blood sugar spikes and support insulin sensitivity. This approach delivers sustained energy and supports prediabetes remission better than low-carb extremism.
3. Optimize Protein Intake: The PREVIEW trial evidence strongly supports adequate dietary protein (roughly 1.2-1.5g per kg body weight) from diverse sources. Protein intake helps preserve muscle during weight loss, promotes satiety, and directly improves insulin sensitivity.
4. Pursue Personalized Prevention: Work with healthcare providers who understand precision medicine principles. Your intervention strategy should reflect your individual metabolic capacity, genetics, lifestyle, and progression risk—not generic guidelines.
5. Act Early and Decisively: The research consensus is clear: prediabetes remission is most achievable within the first few years of diagnosis. Don't delay implementing lifestyle changes or pursuing medical support if needed.
✓ Evidence Summary: Combining high-quality carbohydrates, adequate dietary protein, strategic weight loss, regular physical activity, and personalized risk assessment produces prediabetes remission rates exceeding 50-60% within 2-3 years.
Mechanistic Insights: Why Prediabetes Progresses
1️⃣ Glucotoxicity vs. Lipotoxicity
Glucotoxicity refers to the harmful effects of chronically elevated blood glucose on pancreatic β-cells and insulin-sensitive tissues. Persistent hyperglycemia increases oxidative stress, activates inflammatory pathways, and impairs insulin gene expression. Over time, β-cells lose their ability to secrete insulin appropriately, accelerating progression toward type 2 diabetes.
Lipotoxicity, in contrast, results from excess circulating free fatty acids and ectopic fat deposition (liver, muscle, pancreas). Elevated fatty acids impair insulin signaling pathways, promote mitochondrial dysfunction, and worsen inflammation. In the pancreas, fat accumulation further damages β-cells. In reality, prediabetes progression usually involves glucolipotoxicity—the combined toxic effect of high glucose and high lipid availability.
2️⃣ Hepatic vs. Muscle Insulin Resistance
Hepatic insulin resistance primarily affects fasting glucose levels. The liver continues producing glucose (via gluconeogenesis) despite adequate or elevated insulin levels. This explains why fasting glucose often rises early in prediabetes.
Muscle insulin resistance, however, impairs postprandial glucose disposal. Since skeletal muscle accounts for ~70–80% of insulin-mediated glucose uptake after meals, resistance at this level leads to exaggerated post-meal glucose spikes.
Clinically:
Elevated fasting glucose → stronger hepatic component
Elevated postprandial glucose → stronger muscle component
Both mechanisms often coexist but may predominate differently across individuals.
3️⃣ Visceral Adiposity vs. BMI
Body Mass Index (BMI) measures total body mass relative to height—but it does not distinguish fat distribution.
Visceral adiposity (intra-abdominal fat surrounding organs) is metabolically active and strongly associated with:
Hepatic insulin resistance
Elevated triglycerides
Low HDL cholesterol
Systemic inflammation
Individuals with “normal” BMI may still have excess visceral fat (“TOFI” – thin outside, fat inside) and significant metabolic risk. Conversely, some individuals with higher BMI but low visceral fat may have relatively preserved insulin sensitivity.
Waist circumference and waist-to-height ratio often predict metabolic risk more accurately than BMI alone.
Clinical Takeaway
Prediabetes progression is not simply about “high sugar.” It reflects a dynamic interplay between glucose toxicity, lipid excess, organ-specific insulin resistance, and fat distribution. Understanding these mechanisms supports a more precise, individualized prevention strategy.
Key Takeaways: What You Need to Know About Prediabetes
Essential Prediabetes Facts:
Prediabetes is reversible. With evidence-based interventions, prediabetes remission is achievable for most people, especially when caught early.
Carbohydrate quality matters more than quantity. Focus on low glycemic index foods rather than severe carbohydrate restriction to support blood sugar control.
Protein is your ally. Adequate dietary protein improves metabolic health, supports weight loss, and enhances insulin sensitivity.
One-size-fits-all approaches fail. Precision prevention tailored to your metabolic profile outperforms generic dietary recommendations.
Early action is critical. Prediabetes remission success rates are highest within the first 2-3 years—don't wait to intervene.
Risk varies by individual. Use risk stratification tools to understand your personal progression risk and intervention intensity needs.
Sustainable lifestyle change beats perfection. Adherence to any healthy dietary pattern that emphasizes whole foods and weight loss exceeds sporadic attempts at extreme measures.
Frequently Asked Questions About Prediabetes
Q: Can prediabetes be reversed completely?
Yes, absolutely. Current evidence demonstrates that 50-60% of people with prediabetes achieve remission (return to normal blood glucose levels) through lifestyle interventions alone, particularly when they combine dietary modification emphasizing high-quality carbohydrates and adequate protein intake, with regular physical activity and weight loss. The PREVIEW trial specifically confirmed sustained prediabetes remission is achievable long-term.
Q: What's the difference between prediabetes and type 2 diabetes?
Prediabetes represents the intermediate stage—blood glucose levels are elevated but not yet in the diabetic range. This crucial distinction means prediabetes is far more reversible than established type 2 diabetes. The metabolic damage is less advanced, making prediabetes remission through lifestyle intervention highly feasible. Type 2 diabetes may require pharmacological management alongside lifestyle changes.
Q: Should I completely eliminate carbohydrates?
No. The latest research strongly argues against carbohydrate elimination. Instead, focus on carbohydrate quality. The PREVIEW trial demonstrated that low glycemic index carbohydrates—whole grains, legumes, vegetables—are not only acceptable but beneficial for prediabetes management. These foods provide sustained energy, support metabolic health, and promote better adherence than restrictive approaches. The goal is choosing carbohydrates that minimize rapid blood sugar spikes.
Q: How much protein do I need if I have prediabetes?
The PREVIEW trial and supporting research suggest approximately 1.2-1.5 grams of dietary protein per kilogram of body weight daily is optimal for prediabetes management. This level supports weight loss, helps maintain muscle mass, increases satiety, and directly improves insulin sensitivity. Good sources include lean meats, fish, eggs, dairy, legumes, and plant-based proteins.
Q: How fast can I see improvements in my blood sugar?
Many people see measurable improvements in blood glucose control within 2-4 weeks of implementing comprehensive dietary and lifestyle changes. However, meaningful prediabetes remission typically requires 3-6 months of consistent effort. The good news: research shows the best results occur in the first 2-3 years after prediabetes diagnosis, so time is on your side if you act promptly.
Q: Do I need medication if I'm diagnosed with prediabetes?
Prediabetes management typically begins with aggressive lifestyle intervention. However, risk stratification tools (as discussed in the Luo et al. study) can identify individuals at ultra-high progression risk who may benefit from pharmacological support alongside lifestyle changes. Work with your healthcare provider to determine whether your individual risk profile warrants medication to enhance prediabetes remission prospects.
Q: Is prediabetes hereditary?
Family history is a recognized risk factor, but genetics is not destiny. The Meads meta-analysis confirms that lifestyle interventions reduce prediabetes progression risk by 58% regardless of family history. While genetic predisposition may mean you need to be more proactive than others, prediabetes remission remains entirely achievable through evidence-based dietary and lifestyle modifications.
The Bottom Line: Your Path to Prediabetes Remission
The convergence of evidence from 2025's breakthrough research delivers an unmistakable message: prediabetes remission is within reach. You're not facing an inevitable decline toward type 2 diabetes. Instead, you're standing at a critical juncture where purposeful action can completely reverse your trajectory.
The formula for success combines:
Quality nutrition emphasizing low glycemic index carbohydrates and adequate dietary protein
Regular physical activity targeting both aerobic exercise and strength training
Meaningful weight loss (5-10% of body weight produces measurable metabolic improvements)
Individualized risk assessment to understand your specific progression risk and intervention needs
Early, decisive action before metabolic damage becomes irreversible
Ready to Take Control of Your Metabolic Health?
Don't let prediabetes determine your future. The evidence is clear: prediabetes remission is achievable with the right approach. Talk to your healthcare provider about precision prevention strategies tailored to your metabolic profile, and consider consulting a registered dietitian specializing in prediabetes management to optimize your dietary intervention plan.
Author’s Note
Prediabetes is often delivered to patients as a quiet warning—numbers slightly elevated, reassurance offered, follow-up planned. Yet beneath those mild laboratory abnormalities lies a biologically dynamic state that is far more reversible than many assume. I wrote this article to challenge the outdated narrative that prediabetes is simply an inevitable prelude to type 2 diabetes.
The science has evolved. We now understand that early dysglycemia reflects complex interactions among insulin resistance, beta-cell stress, visceral adiposity, sleep disruption, and metabolic phenotype variability. Just as importantly, we have compelling evidence that timely, targeted interventions can restore metabolic balance in a substantial proportion of individuals. Remission is not theoretical—it is physiologically achievable.
My goal in presenting this synthesis of recent research is twofold. First, to translate emerging evidence into practical, clinically relevant strategies. Second, to emphasize precision over generalization. Not all prediabetes is identical. Risk differs. Mechanisms differ. Response to intervention differs. Management must reflect that biological diversity.
This article is not intended to replace individualized medical care. Rather, it is meant to empower both clinicians and patients with clarity: prediabetes represents a window of opportunity. When identified early and addressed decisively—with structured nutrition, resistance and aerobic training, adequate sleep, and appropriate risk stratification—the metabolic trajectory can change dramatically.
Prediabetes is not destiny. It is a decision point.
Disclaimer: This article is for educational purposes and should not replace professional medical advice. Always consult with your healthcare provider before starting new dietary or exercise programs, especially if you have been diagnosed with prediabetes or other metabolic conditions.
Related Articles
Stop the Clock: Proven Ways to Reverse Early Aging if You Have Diabetes | DR T S DIDWAL
Low-Fat vs. Low-Carb: Which Diet is Best for Weight Loss? | DR T S DIDWAL
5 Steps to Reverse Metabolic Syndrome: Diet, Habit, & Lifestyle Plan | DR T S DIDWAL
The Role of Cholesterol in Health and Disease: Beyond the "Bad" Label | DR T S DIDWAL
Research References & Citations
Prediabetes. (2025). Nature Reviews Disease Primers, 11, 50. https://doi.org/10.1038/s41572-025-00639-w
Zhu, R., Guo, J., Huttunen-Lenz, M., Silvestre, M., Stratton, G., Macdonald, I. A., Handjieva-Darlenska, T., Handjiev, S., Navas-Carretero, S., Poppitt, S. D., Fogelholm, M., Martinez-Urbistondo, D., Martinez, J. A., Raben, A., & Brand-Miller, J. (2026). Long-term effects of dietary protein and carbohydrate quality on prediabetes remission: Results from the PREVIEW randomised multinational diabetes prevention trial. Diabetologia, 69(1), 81–92. https://doi.org/10.1007/s00125-025-06560-x
Wagner, R., Selvin, E., Sehgal, R., Prystupa, K., Misra, S., Fritsche, A., & Heni, M. (2026). Beyond glucose—Rethinking prediabetes for precision prevention. Diabetes Care, 49(2), 226–235. https://doi.org/10.2337/dci25-0054
Luo, J., Hu, D., Han, R., et al. (2025). Risk stratification at prediabetes onset and association with diabetes outcomes using EHR data. npj Metabolism & Health Disease, 3, 48. https://doi.org/10.1038/s44324-025-00091-0
Meads, K., Machiraju, P., Shi, Y., & Colagiuri, S. (2026). Predicting pre-diabetes progression: A systematic review and meta-analysis. BMJ Nutrition, Prevention & Health. https://doi.org/10.1136/bmjnph-2024-000877