The Mediterranean–Plant-Based Hybrid Diet: Why Scientists Now Call It the New Gold Standard for Longevity
Is the Mediterranean–plant-based hybrid the ultimate longevity diet? Explore the science behind heart health, LDL reduction, and anti-inflammatory benefits.
NUTRITION
Dr. T.S. Didwal, M.D.(Internal Medicine)
2/20/202615 min read
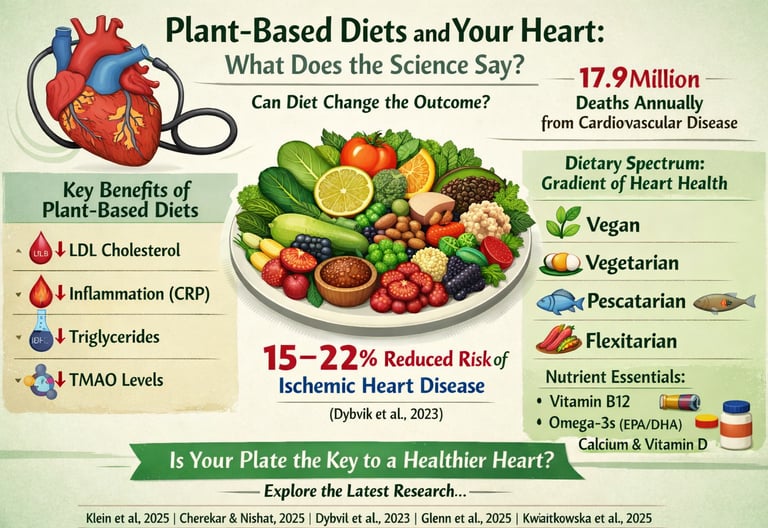
Cardiovascular disease (CVD) remains the leading cause of global mortality, responsible for nearly 17.9 million deaths annually. Yet one of the most powerful tools for preventing atherosclerosis, heart attack, and stroke may not be found in a prescription bottle — but on your plate. A rapidly expanding body of evidence suggests that a plant-based diet for cardiovascular health can significantly improve lipid profiles, reduce systemic inflammation, enhance insulin sensitivity, and lower long-term risk of ischemic heart disease.
Recent high-quality studies demonstrate that dietary patterns rich in whole grains, legumes, fruits, vegetables, nuts, and seeds are associated with lower LDL cholesterol, reduced C-reactive protein (CRP), improved triglyceride levels, and favorable shifts in fatty acid composition (Klein et al., 2025; Cherekar & Nishat, 2025). Prospective cohort data further show that vegetarian and vegan dietary patterns are linked to a 15–22% lower risk of ischemic heart disease compared with omnivorous diets (Dybvik et al., 2023). Even metabolomic analyses reveal reductions in pro-atherogenic compounds such as trimethylamine N-oxide (TMAO) and beneficial shifts in bile acid metabolism following plant-based interventions (Glenn et al., 2025).
Importantly, cardiovascular benefit appears to follow a gradient: vegan, vegetarian, pescatarian, and flexitarian diets each confer progressively measurable improvements in cardiometabolic biomarkers (Kwiatkowska et al., 2025). However, nutrient adequacy — particularly vitamin B12, omega-3 fatty acids (EPA/DHA), calcium, and vitamin D — remains essential for optimizing outcomes.
So what does the latest research truly say about vegan, vegetarian, and Mediterranean-style diets for heart disease prevention? Let’s examine the science behind plant-based nutrition and cardiovascular risk reduction.
Clinical pearls
1. The "B12-Homocysteine" Paradox
Scientific Perspective: While plant-based diets are high in folate (which typically lowers homocysteine), a lack of Vitamin B12 inhibits the methionine synthase enzyme. This leads to an accumulation of homocysteine, a known independent risk factor for arterial damage and thrombosis.
Patient Perspective: "Eating more greens is great for your heart, but without a B12 supplement, your body can’t process certain proteins correctly. This can actually create a 'hidden' risk for your arteries even if your cholesterol looks perfect."
2. The Algae-Omega Connection
Scientific Perspective: Vegans often show high levels of Alpha-Linolenic Acid (ALA) but low levels of EPA and DHA due to the poor conversion rate in the human body. These long-chain fatty acids are critical for modulating cardiac rhythm and lowering systemic inflammation (IL-6).
Flax and chia seeds are good, but they don't provide the specific 'long-chain' fats your heart needs to stay in a steady rhythm. Think about adding an algae-based supplement—it’s essentially 'fish oil' without the fish.
3. "TMAO" as a Biological Fingerprint
Scientific Perspective: Metabolomic profiling shows that plant-based diets significantly reduce Trimethylamine N-oxide (TMAO). TMAO is a byproduct of gut bacteria processing choline and carnitine (found in red meat/eggs) and is directly linked to the formation of arterial plaque.
When you eat less meat, you aren't just cutting fat; you are actually changing your gut chemistry. You stop producing a specific toxin (TMAO) that acts like 'rust' on the inside of your blood vessels."
4. Adherence vs. Absolute Efficacy
Scientific Perspective: While strict vegan diets may offer a statistically superior reduction in LDL cholesterol in the short term, the Mediterranean diet often shows better long-term "real-world" outcomes due to higher palatability and inclusion of monounsaturated fats (olive oil).
A strict vegan diet is like a high-performance race car—it’s fast at lowering cholesterol, but hard to drive every day. A 'Mediterranean-style' plant-based diet is often the 'reliable SUV' that gets you to the finish line of long-term health."
5. The "Halo Effect" of Plant-Based Labels
Scientific Perspective: Cross-sectional data (Kwiatkowska et al., 2025) emphasizes that dietary quality (whole vs. processed) matters as much as the category. A "high-sugar" vegan diet can trigger inflammatory markers like C-reactive protein (CRP) just as easily as a poor omnivorous diet.
Just because a cookie or a bag of chips is 'vegan' doesn't mean it’s 'heart-healthy.' A soda-and-fries vegan diet will still raise your inflammation. Focus on foods that look like they just came out of the ground."
6. The "Gradient of Benefit" (Flexitarianism)
Scientific Perspective: The research demonstrates a dose-response relationship. You don't need 100% elimination of animal products to see a shift in metabolomic signatures or insulin sensitivity; even moving to a flexitarian pattern moves the biological dial.
Heart health isn't an 'all-or-nothing' game. You don't have to be a perfect vegan to protect your heart. Every time you swap a beef burger for a bean burger, you are physically changing your blood chemistry for the better."
The Heart of the Matter
What if the best longevity diet isn’t strictly Mediterranean—or fully plant-based—but a strategic fusion of both?
In 2025, nutrition science is moving beyond diet tribalism. A growing body of large cohort studies and cardiometabolic trials suggests that combining the anti-inflammatory, polyphenol-rich foundation of the Mediterranean diet with the fibre-dense, LDL-lowering power of plant-based eating may deliver superior protection against cardiovascular disease, metabolic dysfunction, and biological aging.
The traditional Mediterranean pattern—rich in extra virgin olive oil, legumes, vegetables, nuts, seafood, and moderate fermented dairy—has long been associated with reduced cardiovascular events and improved survival. Meanwhile, well-formulated plant-forward diets consistently demonstrate reductions in LDL cholesterol, systemic inflammation, insulin resistance, and TMAO levels.
But here’s the shift: emerging evidence suggests that a Mediterranean–plant-based hybrid—prioritizing whole plants, minimizing ultra-processed foods, using olive oil as the primary fat, emphasizing legumes over red meat, and incorporating modest fish intake—may optimize both cardiovascular resilience and metabolic flexibility.
Unlike restrictive dietary extremes, this hybrid model appears sustainable, culturally adaptable, and cardiometabolically protective. It aligns with mechanistic pathways linked to longevity, including improved endothelial function, enhanced gut microbiome diversity, lower oxidative stress, and reduced chronic inflammation.
In a world where heart disease remains the leading global cause of death, and metabolic disease continues to rise, the question is no longer “Mediterranean or plant-based?”
Fatty Acids and Diet: What Your Blood Reveals About What You Eat
One of the most illuminating windows into dietary quality is the fatty acid composition of the blood. A 2025 study published in Lipids Health and Disease by Klein et al. investigated exactly this, drawing on data from the NuEva (Nutrition Evaluation) cohort to compare fatty acid profiles across four dietary groups: omnivores, flexitarians, vegetarians, and vegans.
The study found meaningful and systematic differences in fatty acid profiles that tracked closely with dietary patterns. Individuals following vegan and vegetarian diets demonstrated higher levels of linoleic acid and alpha-linolenic acid — the primary plant-derived omega-6 and omega-3 fatty acids, respectively. Omnivores, in contrast, showed higher concentrations of long-chain saturated fatty acids and arachidonic acid, a pro-inflammatory omega-6 fatty acid predominantly found in animal-derived foods.
A particularly noteworthy finding was the lower eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) levels in vegans compared to omnivores and flexitarians. These long-chain omega-3 fatty acids, typically abundant in fatty fish, play critical roles in reducing triglycerides, modulating inflammation, and supporting cardiac rhythm. The data suggest that while plant-forward diets excel in several fatty acid metrics, they may require supplementation strategies — such as algae-based omega-3 products — to fully optimise cardiovascular protection.
🔑 Key Takeaway (Klein et al., 2025): Plant-based dietary patterns produce measurably healthier fatty acid profiles overall, but vegans specifically show lower EPA and DHA levels, highlighting the importance of targeted omega-3 supplementation or algae-based dietary sources.
LDL Cholesterol: Plants vs. the Mediterranean Model
Low-density lipoprotein (LDL) cholesterol is widely regarded as a primary driver of atherosclerosis and cardiovascular events. Two dietary patterns have generated the most robust evidence for LDL reduction: plant-based vegan diets and the Mediterranean diet. Leoni et al. (2025), writing in the Mediterranean Journal of Nutrition and Metabolism, took a comparative approach to examine which of these two paradigms performs better at lowering LDL.
The review found that both dietary patterns achieved meaningful LDL reductions compared to standard Western diets, but through different mechanisms. Plant-based vegan diets exert their cholesterol-lowering effects primarily through the elimination of dietary cholesterol, the reduction of saturated fat intake, and the increased intake of soluble fibre, plant sterols, and phytochemicals that inhibit cholesterol absorption. The Mediterranean diet, by contrast, relies more heavily on the protective effects of monounsaturated fatty acids from olive oil and the anti-inflammatory properties of polyphenols.
Leoni et al. concluded that strict plant-based vegan diets demonstrated a modest but consistent edge over Mediterranean diets in LDL reduction, particularly in short-term intervention studies. However, the Mediterranean diet's greater palatability and long-term adherence rates make it a powerful tool in clinical practice, where sustainability is as important as short-term efficacy.
The authors advocate for a nuanced "best of both worlds" approach — encouraging clinicians to guide patients toward diets that are rich in whole plant foods while also incorporating Mediterranean principles such as olive oil, legumes, nuts, and moderate consumption of oily fish.
🔑 Key Takeaway (Leoni et al., 2025): Vegan diets may produce slightly greater LDL reductions than Mediterranean diets in the short term, but long-term adherence and clinical applicability may favour Mediterranean-style eating for many patients.
Blood Biomarkers Tell a Broader Story
Beyond lipid profiles, a range of blood biomarkers provides a more comprehensive view of cardiovascular risk. Cherekar and Nishat (2025), writing in the European Journal of Cardiovascular Medicine, conducted a comparative analysis of blood biomarkers between vegetarians and non-vegetarians with specific attention to cardiovascular implications.
The study found that vegetarians consistently demonstrated lower total cholesterol, LDL cholesterol, triglycerides, fasting blood glucose, and markers of systemic inflammation — including C-reactive protein (CRP) — compared to their non-vegetarian counterparts. High-density lipoprotein (HDL) cholesterol, often called "good cholesterol," was similar across groups, though some sub-analyses suggested slightly lower HDL in strict vegans.
Crucially, vegetarians in this study also showed lower levels of homocysteine — an amino acid associated with an increased risk of cardiovascular disease when elevated — though the difference was modest and partly attributed to B12 status. This raises an important clinical point: vegetarian and vegan diets can reduce homocysteine risk through higher folate intakes, but may paradoxically elevate homocysteine if vitamin B12 deficiency is present, as B12 is needed for homocysteine metabolism.
The study reinforces the view that a well-planned plant-based diet provides a cardiovascularly favourable biomarker profile, but adequate supplementation — particularly for B12, iron, zinc, and omega-3 fatty acids — is essential to avoid nutrient gaps that could undermine those benefits.
🔑 Key Takeaway (Cherekar & Nishat, 2025): Vegetarian diets are associated with significantly better cardiovascular biomarker profiles including lower LDL, CRP, and triglycerides, but attention to micronutrient sufficiency — especially vitamin B12 — is critical to realising these benefits safely.
The Long View: Cohort Studies on Disease Risk
While biomarker studies capture mechanistic snapshots, prospective cohort studies tell us what ultimately happens to people over years and decades. Dybvik et al. (2023), in a systematic review and meta-analysis published in the European Journal of Nutrition, synthesised data from multiple prospective studies to evaluate whether vegetarian and vegan diets are associated with lower risks of cardiovascular disease, ischemic heart disease, and stroke.
Their findings were broadly supportive of plant-based dietary patterns: vegetarian and vegan diets were associated with a statistically significant 15–22% reduction in the risk of ischemic heart disease compared to omnivorous diets. The risk reduction was most pronounced for ischemic heart disease — the variety driven by coronary artery disease and reduced blood flow to the heart — which aligns with the mechanistic evidence around lipid and inflammatory improvements.
The picture for stroke was more nuanced. Some analyses suggested a potential small increase in hemorrhagic stroke risk among vegans, possibly linked to lower intakes of certain nutrients including calcium, vitamin D, and omega-3 fatty acids. However, the overall cardiovascular risk profile remained favourable, and the absolute risk increase for hemorrhagic stroke was small relative to the ischemic heart disease benefit.
The meta-analysis highlights an important caveat: much of the available cohort data comes from populations with specific socioeconomic and cultural characteristics, which limits generalisability. Nevertheless, the breadth and consistency of the data across populations provides compelling evidence that plant-forward diets offer meaningful long-term cardiovascular protection.
🔑 Key Takeaway (Dybvik et al., 2023): Vegetarian and vegan diets are associated with a 15–22% reduction in ischemic heart disease risk. The evidence for stroke is more complex, emphasising that dietary quality and nutrient sufficiency are as important as dietary category.
Diet, Lifestyle, and Inflammation: A Cross-Sectional Lens
Dietary patterns do not operate in isolation — they are deeply intertwined with lifestyle factors including physical activity, smoking, alcohol consumption, and sleep. Kwiatkowska et al. (2025), publishing in Nutrients, explored these interactions through a cross-sectional design comparing cardiovascular and inflammatory biomarkers across vegans, vegetarians, pescatarians, and omnivores.
The study found that vegans and vegetarians reported higher levels of physical activity and lower rates of smoking compared to omnivores, complicating the attribution of biomarker differences purely to diet. However, even after statistical adjustment for lifestyle confounders, plant-based groups maintained significantly lower levels of CRP, interleukin-6 (IL-6), and other inflammatory markers.
Pescatarians showed a particularly interesting profile: their inflammatory markers were similarly low to those of vegans and vegetarians, and their omega-3 fatty acid levels were substantially higher, reflecting regular fish consumption. This suggests that a pescatarian approach — predominantly plant-based with the addition of seafood — may represent an optimal middle ground that captures the anti-inflammatory benefits of both plant foods and marine omega-3s.
The study also highlighted significant variation within dietary categories. Not all vegan or vegetarian diets are equal — a vegan diet heavy in processed foods, refined carbohydrates, and added sugars could theoretically produce worse inflammatory outcomes than a well-designed omnivorous diet rich in vegetables, legumes, and whole grains. Dietary quality, not merely dietary label, is what ultimately determines cardiovascular outcomes.
🔑 Key Takeaway (Kwiatkowska et al., 2025): Plant-based diets are independently associated with lower inflammatory biomarkers, but dietary quality within categories matters enormously. Pescatarian diets may offer unique advantages by combining plant food benefits with marine omega-3 intake.
Metabolomics: Reading the Chemical Language of a Plant-Based Diet
Metabolomics — the large-scale study of small molecule metabolites — is one of the most exciting frontiers in nutritional science, offering an unprecedented view of how diet reshapes biochemistry at a molecular level. Glenn et al. (2025), writing in the European Journal of Clinical Nutrition, conducted metabolomic profiling of a cholesterol-lowering plant-based diet using data from two randomised controlled feeding trials.
Their findings revealed that the plant-based dietary intervention produced a distinct and favourable metabolomic signature. Levels of trimethylamine N-oxide (TMAO) — a gut-derived metabolite strongly linked to atherosclerosis and cardiovascular events — fell significantly in participants consuming plant-based diets, consistent with the reduced availability of TMAO precursors from animal products. Bile acid metabolites shifted in ways consistent with improved cholesterol excretion. Short-chain fatty acid precursors increased, reflecting enhanced prebiotic activity from dietary fibre.
Particularly striking was the upregulation of metabolites associated with improved insulin sensitivity and glucose regulation, suggesting that the cardiovascular benefits of plant-based diets extend beyond lipid changes into broader metabolic protection. The dual randomised controlled trial design strengthens the causal interpretation of these findings, moving beyond mere association to demonstrate that plant-based dietary changes produce these metabolomic shifts.
Glenn et al. also identified several novel metabolic pathways that may partly explain why plant-based diets outperform many pharmacological LDL-lowering interventions in metabolomic breadth — statins lower LDL effectively, but they do not replicate the wide-spectrum metabolic improvements that accompany dietary change.
🔑 Key Takeaway (Glenn et al., 2025): Plant-based diets produce a broad and favourable metabolomic signature — including reductions in TMAO, shifts in bile acid metabolism, and improvements in insulin sensitivity markers — that exceeds what single-nutrient interventions can achieve.
Synthesising the Evidence: What Does It All Mean?
Cardiovascular Disease Remains the Dominant Global Health Threat
Cardiovascular disease (CVD) accounts for approximately 17.9 million deaths annually worldwide. Dietary modification represents one of the most scalable, cost-effective, and biologically potent strategies for primary and secondary prevention.Plant-Based Diets Demonstrate Consistent Lipid-Lowering Effects
Across controlled trials and observational data, vegan and vegetarian dietary patterns are associated with meaningful reductions in LDL cholesterol, total cholesterol, and triglycerides. Comparative analyses suggest vegan diets may produce slightly greater short-term LDL reductions than Mediterranean diets, largely through elimination of dietary cholesterol and reduced saturated fat intake.Inflammatory Burden Is Significantly Reduced
Plant-forward dietary patterns correlate with lower levels of systemic inflammatory markers, including C-reactive protein (CRP) and interleukin-6. These reductions persist even after adjusting for lifestyle confounders such as smoking and physical activity.Favorable Fatty Acid Remodeling Occurs
Vegans and vegetarians exhibit higher circulating levels of plant-derived omega-3 (ALA) and omega-6 fatty acids, alongside lower long-chain saturated fats. However, reduced EPA and DHA levels in strict vegans underscore the importance of algae-based omega-3 supplementation.Prospective Cohort Data Support Long-Term Risk Reduction
Meta-analytic evidence indicates a 15–22% reduction in ischemic heart disease risk among vegetarian and vegan populations. Stroke data are more nuanced, with possible small increases in hemorrhagic stroke risk linked to nutrient insufficiency in poorly planned diets.Metabolomic Insights Strengthen Causal Interpretation
Randomised feeding trials reveal plant-based diets reduce pro-atherogenic metabolites such as trimethylamine N-oxide (TMAO) and favorably alter bile acid metabolism and insulin sensitivity pathways. These changes extend beyond traditional lipid metrics.A Gradient of Cardiovascular Benefit Exists
Cardiometabolic improvements generally follow plant density: vegan > vegetarian > pescatarian > flexitarian > omnivorous. Importantly, pescatarian patterns may offer an advantageous hybrid profile due to marine omega-3 intake.Dietary Quality Overrides Dietary Label
Whole-food, minimally processed plant-based diets drive benefit. Ultra-processed vegan diets may not confer similar protection.Micronutrient Sufficiency Is Non-Negotiable
Vitamin B12, EPA/DHA, calcium, vitamin D, iron, and zinc must be actively managed in plant-exclusive diets to avoid undermining cardiovascular gains.Clinical Implication: Diet as Foundational Therapy
The cumulative evidence positions plant-forward eating as a first-line cardiometabolic intervention, complementary to pharmacotherapy and lifestyle modification. Incremental dietary shifts can yield measurable biological dividends.
The convergence of mechanistic, biomarker, and longitudinal outcome data strongly supports plant-based dietary patterns as a cornerstone of cardiovascular prevention strategy — provided they are evidence-informed, nutritionally complete, and sustainably implemented.
Frequently Asked Questions (FAQs)
1. Do I have to go fully vegan to benefit my heart health? No. The evidence consistently shows a gradient of cardiovascular benefit, with even flexitarian and vegetarian diets demonstrating improvements over standard omnivorous eating. Meaningful reductions in cardiovascular risk markers can be achieved by simply increasing whole plant food consumption and reducing red and processed meat, without adopting a fully vegan lifestyle (Kwiatkowska et al., 2025; Dybvik et al., 2023).
2. Is a plant-based diet better than the Mediterranean diet for lowering cholesterol? Both approaches reduce LDL cholesterol significantly compared to standard Western diets. Strict plant-based vegan diets may offer a modest advantage in LDL reduction in controlled settings, but Mediterranean diets may be easier to maintain long term. Many experts recommend a "Mediterranean-plant-based hybrid" that emphasises legumes, wholegrains, vegetables, nuts, and olive oil (Leoni et al., 2025).
3. Should vegans take omega-3 supplements? The evidence from fatty acid profiling studies suggests that vegans typically have lower EPA and DHA levels — the long-chain omega-3s most associated with cardiac protection. Algae-based omega-3 supplements provide a plant-derived source of EPA and DHA and are recommended for vegans who wish to optimise their cardiovascular fatty acid profile (Klein et al., 2025).
4. What is TMAO and why does it matter for heart health? Trimethylamine N-oxide (TMAO) is a metabolite produced by gut bacteria when they process certain compounds found primarily in animal products such as red meat, eggs, and fish. Elevated TMAO levels in the blood are associated with increased risk of atherosclerosis and cardiovascular events. Plant-based diets significantly reduce TMAO levels by limiting the dietary precursors that gut bacteria use to produce it (Glenn et al., 2025).
5. Can a vegetarian diet actually cause any cardiovascular harm? The evidence generally indicates net cardiovascular benefit from vegetarian diets. However, Dybvik et al. (2023) noted a potential modest increase in hemorrhagic stroke risk in some vegan sub-groups, possibly linked to lower intakes of calcium, vitamin D, and long-chain omega-3s. This underscores the importance of dietary planning and supplementation rather than the dietary label alone.
6. How quickly do cardiovascular biomarkers improve after switching to a plant-based diet? Metabolomic and biomarker studies suggest improvements can occur relatively quickly — within weeks to months — following a shift to a plant-based dietary pattern. Glenn et al. (2025) observed significant metabolomic changes in controlled feeding trial settings, and lipid improvements, including LDL reductions, are typically measurable within four to eight weeks of dietary change.
7. Does a plant-based diet help with more than just cholesterol? Absolutely. The research reviewed here demonstrates improvements across multiple cardiovascular risk dimensions: reduced inflammation (lower CRP and IL-6), improved insulin sensitivity, lower triglycerides, reduced TMAO production, better fatty acid profiles, and long-term reductions in ischemic heart disease risk. These findings suggest systemic cardiovascular protection that goes well beyond cholesterol management alone (Kwiatkowska et al., 2025; Glenn et al., 2025; Cherekar & Nishat, 2025).
Author’s Note
As a physician trained in internal medicine and deeply engaged in cardiometabolic research, my goal in writing this article is not to promote a dietary ideology, but to present the best available scientific evidence in a clinically meaningful way. Nutrition discussions often become polarised — vegan versus omnivore, Mediterranean versus low-carb — yet the science consistently points toward a more nuanced truth: dietary patterns rich in whole, minimally processed plant foods are strongly associated with improved cardiovascular biomarkers and long-term heart health.
The studies synthesised here include randomised controlled trials, prospective cohort analyses, cross-sectional biomarker evaluations, and cutting-edge metabolomic research. Together, they provide a multidimensional understanding of how plant-forward eating influences LDL cholesterol, inflammation, fatty acid profiles, insulin sensitivity, and atherosclerotic risk pathways.
However, evidence-based nutrition also requires intellectual honesty. Plant-based diets are not automatically health-promoting unless they are well-planned. Attention to vitamin B12, omega-3 fatty acids (EPA/DHA), calcium, vitamin D, iron, and zinc is essential. Dietary quality matters more than dietary labels.
My hope is that this article empowers both clinicians and readers to make informed decisions grounded in physiology, biochemistry, and long-term outcome data — not trends. Food is not merely fuel; it is a modifiable determinant of cardiometabolic risk. And when applied thoughtfully, dietary strategy can complement — and sometimes rival — pharmacological intervention in reducing cardiovascular disease burden.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Individual circumstances vary, and treatment decisions should always be made in consultation with qualified healthcare professionals.
Related Articles
Beyond the Low-Fat Myth: 6 New Studies Redefining Dietary Fat and Heart Health | DR T S DIDWAL
Can Plant-Based Polyphenols Lower Biological Age? | DR T S DIDWAL
Time-Restricted Eating: Metabolic Advantage or Just Fewer Calories? | DR T S DIDWAL
Can You Revitalize Your Immune System? 7 Science-Backed Longevity Strategies | DR T S DIDWAL
Exercise and Longevity: The Science of Protecting Brain and Heart Health as You Age | DR T S DIDWAL
References
Cherekar, L. N., & Nishat, K. H. (2025). Comparison of blood biomarkers in vegetarian and non-vegetarian diets: Implications for cardiovascular health. European Journal of Cardiovascular Medicine, 15(5), 673–678. https://doi.org/10.61336/ejcm/2025-05-123
Dybvik, J. S., Svendsen, M., & Aune, D. (2023). Vegetarian and vegan diets and the risk of cardiovascular disease, ischemic heart disease and stroke: A systematic review and meta-analysis of prospective cohort studies. European Journal of Nutrition, 62(1), 51–69. https://doi.org/10.1007/s00394-022-02942-8
Glenn, A. J., Tessier, A.-J., Kavanagh, M. E., et al. (2025). Metabolomic profiling of a cholesterol lowering plant-based diet from two randomized controlled feeding trials. European Journal of Clinical Nutrition, 79, 863–875. https://doi.org/10.1038/s41430-025-01625-x
Klein, L., Lenz, C., Krüger, K., et al. (2025). Comparative analysis of fatty acid profiles across omnivorous, flexitarians, vegetarians, and vegans: Insights from the NuEva study. Lipids Health and Disease, 24, 133. https://doi.org/10.1186/s12944-025-02517-6
Kwiatkowska, I., Olszak, J., & Formanowicz, D. (2025). Dietary and lifestyle patterns and their associations with cardiovascular and inflammatory biomarkers in vegans, vegetarians, pescatarians, and omnivores: A cross-sectional study. Nutrients, 17(23), 3634. https://doi.org/10.3390/nu17233634
Leoni, L., Perazza, F., Maghetti, A., & Ravaioli, F. (2025). Balancing act: LDL-cholesterol control through plant-based vegan and Mediterranean diets. Mediterranean Journal of Nutrition and Metabolism, 18(2), 83–86. https://doi.org/10.1177/1973798X251322800