Reversing Type 2 Diabetes: Skeletal Muscle as a Master Regulator of Metabolic Health
Stop just managing diabetes—start reversing it. Discover how lifting weights transforms your muscles into endocrine powerhouses that lower blood sugar and "cool down" systemic inflammation
DIABETES
Dr. T.S. Didwal, M.D.(Internal Medicine)
12/28/202514 min read
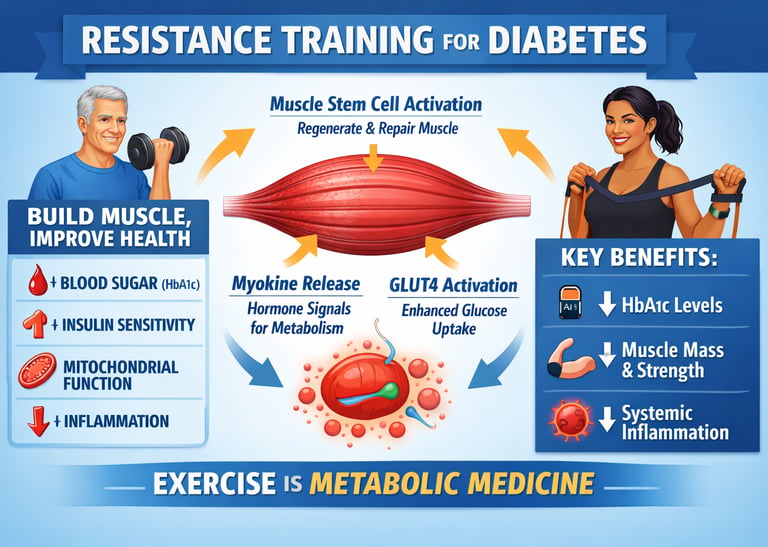
For decades, people living with type 2 diabetes have been told a familiar message: manage your blood sugar, take your medications, and accept that the disease will slowly progress. But emerging science is challenging this narrative—revealing that skeletal muscle, when properly stimulated through resistance training, can actively reverse key drivers of metabolic dysfunction.
Far from being passive tissue, skeletal muscle is now recognized as a powerful endocrine organ that regulates glucose metabolism, inflammation, and insulin sensitivity through the secretion of hundreds of signaling molecules known as myokines (Iglesias, 2025). These muscle-derived factors communicate directly with the liver, pancreas, adipose tissue, and even the brain, reshaping whole-body metabolic health.
Even more compelling, resistance training triggers deep cellular and molecular adaptations within muscle itself. Studies show that exercise activates dormant muscle stem cells, improves mitochondrial efficiency, and enhances glucose uptake through both insulin-dependent and insulin-independent pathways (Fukada & Nakamura, 2021; Masuda & Matsuzaka, 2025). These changes allow muscle to dispose of glucose more effectively—even in the presence of insulin resistance.
Large clinical analyses confirm that these biological shifts translate into meaningful outcomes: lower HbA1c, improved insulin sensitivity, increased muscle mass, and reduced systemic inflammation in people with type 2 diabetes (Wang et al., 20
Let me walk you through the latest research that's revolutionizing how we understand the relationship between skeletal muscle, endocrine function, and metabolic disease. By the end of this post, you'll understand exactly why your muscles are far more than movement machines—they're powerful endocrine organs that could hold the key to reversing metabolic dysfunction.
Clinical Pearls
1. The "Wake-Up Call" for Muscle Stem Cells
Your muscles contain special repair units called satellite cells. In a sedentary state, these cells become "quiescent"—essentially falling into a deep sleep that leads to muscle wasting. Resistance training sends a mechanical signal through pathways like Notch signaling that acts as a molecular alarm clock. This awakens those dormant stem cells to build new, high-quality muscle fibers that are far more efficient at processing blood sugar than the old ones.
2. The Metabolic "Side Door" for Blood Sugar
In Type 2 Diabetes, the "front door" for sugar (the insulin receptor) is often stuck or broken. Strength training activates an alternative, insulin-independent pathway called GLUT4 translocation. When your muscles work against resistance, they create a metabolic "side door" that pulls glucose directly out of the bloodstream to use as fuel. This allows you to lower your blood sugar effectively, even if your body’s insulin isn't working perfectly.
3. Your Muscles as a "Natural Pharmacy"
We now know that skeletal muscle is actually a powerful endocrine organ. When you lift weights, your muscles secrete "messenger chemicals" called myokines (such as Irisin and IL-6). These travel through your blood to "talk" to other organs—telling your body fat to burn faster, your brain to stay sharp, and your immune system to lower inflammation. Think of every rep as a tiny dose of custom-made medicine your body produces for itself.
4. Cleaning the Cellular "Engines"
Every muscle cell is powered by tiny engines called mitochondria. In metabolic disease, these engines often get "clogged" with waste, making you feel sluggish and insulin resistant. Resistance exercise triggers mitochondrial biogenesis—a process where your body clears out the old, smokey engines and builds brand-new, clean-burning ones. This "cellular spring cleaning" makes your body much better at burning both sugar and fat.
5. The "Afterburn" Effect on Blood Sugar
Building muscle creates a massive "glucose sink" in the body. For up to 48 hours after a strength session, your muscles stay in a state of high repair, continuously pulling sugar from your blood to restock their energy stores. While this is great for long-term health, it’s important to stay hydrated and monitor your levels, as this "metabolic afterburn" means your body is working for you even while you sleep.
Your Muscles Are Endocrine Powerhouses: Understanding the Muscle-Hormone Connection
The Dual Role of Muscle in Your Endocrine System
Skeletal muscle plays a dual role in endocrinology. First, it responds to various hormones including insulin, growth hormone, thyroid hormones, and sex steroids. These hormones regulate muscle protein synthesis, glucose uptake, and overall metabolic function. Second, and perhaps more fascinating, muscle tissue secretes over 600 different myokines—signaling proteins that communicate with virtually every organ system in your body (Iglesias, 2025).
These myokines influence glucose metabolism, lipid oxidation, inflammation, bone health, and even cognitive function. When you engage in resistance training, you're not just building bigger muscles—you're optimizing an entire communication network that regulates your metabolic health.
Key myokines identified in recent research include:
Interleukin-6 (IL-6): Enhances glucose uptake and fat oxidation during exercise
Irisin: Promotes browning of white adipose tissue and improves insulin sensitivity
Myostatin: Regulates muscle growth (exercise reduces myostatin, allowing muscle development)
Brain-derived neurotrophic factor (BDNF): Supports cognitive function and neuroprotection
The implications are profound. Your muscles aren't passive tissues waiting for instructions—they're active participants in hormone regulation and metabolic control. This helps explain why muscle loss (sarcopenia) is so strongly associated with metabolic diseases, and why building muscle through resistance training can reverse metabolic dysfunction.
How Resistance Training Rebuilds Your Metabolic Foundation at the Cellular Level
Now let's dig deeper into what happens inside your muscle cells when you engage in resistance training, particularly if you're dealing with type 2 diabetes or metabolic syndrome.
The Stem Cell Revolution: How Exercise Rejuvenates Aging Muscle
Muscle stem cells (also called satellite cells) are responsible for muscle repair, regeneration, and adaptation. Here's what makes this so important: as we age, our muscle stem cells become less responsive and enter a state called quiescence—essentially going dormant.
Research has found that resistance exercise activates these dormant stem cells, triggering them to proliferate and differentiate into new muscle fibers. This process involves complex signaling pathways including Notch signaling, Wnt signaling, and various growth factors (Fukada & Nakamura, 2021).
What's particularly relevant for people with metabolic disorders is that this stem cell activation doesn't just increase muscle size—it improves muscle quality. The newly formed muscle tissue has enhanced insulin receptor density, improved mitochondrial function, and better glucose transporter expression. Essentially, resistance training gives you metabolically healthier muscle tissue that's more responsive to insulin.
The mechanical stress from resistance exercise creates microtrauma in muscle fibers, which triggers the satellite cell response. This isn't damage in a harmful sense—it's the stimulus that drives adaptation and metabolic improvement.
Personalized Molecular Insights: Why Your Muscles Respond Differently to Exercise
One of the most fascinating recent developments involves using cutting-edge phosphoproteomics to understand how exercise-induced insulin sensitization occurs at the molecular level in skeletal muscle.
Phosphoproteomics is a technique that maps all the protein phosphorylation changes in cells—essentially tracking how exercise flips molecular switches that control insulin signaling. Research has discovered that exercise triggers thousands of phosphorylation events that enhance insulin sensitivity, but here's the remarkable finding: these molecular responses vary significantly between individuals (Masuda & Matsuzaka, 2025).
Insulin resistance in skeletal muscle involves specific disruptions in insulin signaling pathways, particularly affecting proteins like Akt, mTOR, and various glucose transporters. When you perform resistance exercise, you're essentially reprogramming these pathways at the molecular level.
Exercise increases GLUT4 translocation—the movement of glucose transporters to the cell membrane where they can actually import glucose from the bloodstream. Importantly, this exercise-mediated glucose uptake occurs through insulin-independent pathways, meaning exercise can improve glucose control even when insulin signaling is impaired.
The personalized aspect is crucial. Individuals have unique molecular responses to exercise, which explains why some people see dramatic improvements in insulin sensitivity while others respond more gradually. This suggests that personalized exercise prescriptions based on molecular profiling could optimize outcomes for people with type 2 diabetes.
The Complete Picture: Multiple Pathways to Enhanced Insulin Sensitivity
Exercise creates multiple pathways to enhanced insulin sensitivity and improved skeletal muscle health in type 2 diabetes. Recent comprehensive analysis has identified several key mechanisms across molecular, cellular, and systemic levels (Zierath et al., 2025).
Mitochondrial adaptations: Exercise increases both the number and function of mitochondria in muscle cells. These cellular powerhouses become more efficient at burning both glucose and fatty acids, reducing the accumulation of harmful lipid metabolites that interfere with insulin signaling.
Inflammatory modulation: Type 2 diabetes is characterized by chronic low-grade inflammation. Research shows that exercise reduces pro-inflammatory cytokines while increasing anti-inflammatory myokines, creating a more favorable metabolic environment.
Capillary density: Resistance training increases the capillary network within muscle tissue, improving blood flow and nutrient delivery. This enhanced vascularization means glucose and insulin reach muscle cells more efficiently.
Protein quality control: Exercise enhances cellular systems that maintain protein quality, including the ubiquitin-proteasome system and autophagy. These mechanisms remove damaged proteins and organelles that accumulate in diabetic muscle tissue.
These adaptations are interconnected—improvements in one area cascade to enhance others, creating a positive feedback loop that progressively improves metabolic health.
The Meta-Analysis That Changes Everything: Quantifying the Benefits of Resistance Training
While understanding mechanisms is fascinating, you're probably wondering: what are the actual, measurable benefits of resistance training for people with type 2 diabetes? A comprehensive meta-analysis examining multiple studies provides impressive answers with statistical precision (Wang et al., 2025).
Metabolic Transformations: The Numbers That Matter
Studies involving middle-aged and older adults with type 2 diabetes who engaged in resistance training programs have produced remarkable results:
Glycemic control improvements: Resistance training significantly reduced HbA1c levels—the gold standard measure of long-term blood sugar control. The improvements were clinically meaningful, often reducing HbA1c by 0.5-0.8%, which translates to substantially lower diabetes complications risk.
Fasting glucose reduction: Participants experienced significant decreases in fasting blood glucose, indicating improved basal metabolic function even during periods without food intake.
Insulin sensitivity enhancement: Research found consistent improvements in insulin sensitivity indices, meaning the body required less insulin to manage the same amount of glucose—a fundamental reversal of insulin resistance.
Muscular Health: Building Metabolically Active Tissue
Beyond blood sugar control, documented improvements in muscular health include:
Muscle mass increases: Resistance training led to measurable increases in lean body mass and muscle cross-sectional area. This is crucial because muscle tissue is the primary site of glucose disposal—more muscle means greater glucose-handling capacity.
Muscle strength gains: Participants experienced substantial improvements in muscle strength, which correlates with improved physical function, reduced fall risk, and enhanced quality of life.
Body composition changes: Studies showed favorable changes in body composition, with reductions in fat mass particularly visceral adipose tissue—the dangerous fat around internal organs that drives metabolic dysfunction.
Systemic Inflammation: Cooling Down Metabolic Fire
Perhaps most exciting were the findings on systemic inflammation. Resistance training significantly reduced inflammatory markers including (Wang et al., 2025):
C-reactive protein (CRP): A key marker of systemic inflammation dropped substantially with regular resistance training, indicating reduced cardiovascular risk.
Tumor necrosis factor-alpha (TNF-α): This pro-inflammatory cytokine, elevated in diabetes and associated with insulin resistance, decreased with resistance training.
Interleukin-6 (IL-6): While IL-6 increases acutely during exercise (which is beneficial), chronic elevated levels associated with metabolic disease decreased with regular training.
This reduction in chronic inflammation is crucial because inflammation is a key driver of insulin resistance, cardiovascular disease, and diabetic complications. By lowering systemic inflammation, resistance training addresses one of the root causes of metabolic dysfunction.
These benefits were observed across diverse populations, various resistance training protocols, and different study durations, suggesting the findings are robust and broadly applicable.
Practical Implementation: Translating Science into Action
Understanding the science is one thing—applying it is another. Based on the research reviewed, here's how to implement an effective resistance training program for metabolic health:
Training Parameters That Work
The studies examined various training protocols, but certain principles emerged consistently:
Frequency: Training 2-3 times per week produced significant benefits. More frequent training didn't necessarily produce proportionally greater benefits, suggesting adequate recovery is important.
Intensity: Moderate to high intensity (60-80% of one-repetition maximum) was most effective. The mechanical stress needs to be sufficient to trigger the cellular adaptations discussed earlier.
Volume: Programs typically included 8-10 exercises targeting major muscle groups, with 2-3 sets of 8-12 repetitions per exercise.
Progression: Gradually increasing resistance over time (progressive overload) is essential for continued adaptations.
Combining Resistance Training with Other Interventions
While resistance training is powerful, research suggests it works synergistically with other interventions:
Nutrition: Adequate protein intake (1.6-2.2g/kg body weight) supports muscle protein synthesis and maximizes the benefits of resistance training.
Aerobic exercise: Combining resistance training with aerobic exercise may provide additional cardiovascular and metabolic benefits.
Sleep and recovery: The cellular adaptations occur during recovery periods, making adequate sleep (7-9 hours) crucial.
Medication compliance: Resistance training should complement, not replace, prescribed diabetes medications—always work with your healthcare provider.
The Future of Exercise as Metabolic Medicine
The research we've explored represents a fundamental shift in how we understand and treat type 2 diabetes and metabolic disease. We're moving from viewing exercise as a helpful lifestyle factor to recognizing it as a powerful metabolic intervention that addresses the root causes of disease at the cellular and molecular level.
The myokine research opens possibilities for developing pharmaceuticals that mimic exercise effects. The phosphoproteomic work suggests we'll soon have personalized exercise prescriptions optimized for individual molecular profiles. The stem cell research hints at interventions that could enhance muscle regeneration in aging populations.
But here's the crucial point: we don't need to wait for future developments. The interventions we have now—resistance training combined with proper nutrition and lifestyle management—are remarkably effective when consistently applied.
Key Takeaways: What You Need to Remember
🔑 Your muscles are endocrine organs: Skeletal muscle secretes hundreds of myokines that regulate metabolism throughout your body, making muscle health central to metabolic health.
🔑 Resistance training activates muscle stem cells: Exercise awakens dormant satellite cells, creating new, metabolically healthy muscle tissue with enhanced insulin sensitivity.
🔑 Molecular reprogramming occurs with exercise: Resistance training triggers thousands of molecular changes that enhance insulin signaling through both insulin-dependent and insulin-independent pathways.
🔑 Multiple mechanisms work synergistically: Exercise improves mitochondrial function, reduces inflammation, enhances blood flow, and optimizes protein quality control simultaneously.
🔑 Quantifiable metabolic benefits: Meta-analysis confirms significant improvements in HbA1c, fasting glucose, insulin sensitivity, muscle mass, strength, and systemic inflammation markers.
🔑 Inflammation reduction is key: Resistance training substantially lowers chronic inflammation, addressing a root cause of insulin resistance and cardiovascular complications.
🔑 Frequency matters more than volume: Training 2-3 times weekly with moderate-to-high intensity produces significant benefits without requiring excessive time commitment.
Frequently Asked Questions
Q: How long does it take to see improvements in blood sugar control from resistance training?
A: Research shows measurable improvements in insulin sensitivity can occur within 2-4 weeks, though more substantial changes in HbA1c typically appear after 8-12 weeks of consistent training. The molecular changes begin immediately—your muscles start adapting from your very first workout.
Q: Can resistance training help if I'm already taking diabetes medications?
A: Absolutely. Resistance training works through different mechanisms than most diabetes medications, providing complementary benefits. Many people find they can reduce medication doses under medical supervision as their metabolic health improves. Always coordinate exercise programs with your healthcare provider.
Q: I'm older and haven't exercised in years. Is it too late to benefit from resistance training?
A: It's never too late. Research specifically examined middle-aged and older adults and found significant benefits regardless of training history. Your muscle stem cells retain the ability to respond to resistance training even in advanced age, though proper progression and technique become increasingly important.
Q: How is resistance training different from just walking or doing cardio?
A: While aerobic exercise provides important cardiovascular benefits, resistance training uniquely builds muscle mass and triggers specific myokine secretion patterns. The mechanical stress creates cellular adaptations that improve insulin sensitivity through distinct pathways. Ideally, you'd include both types of exercise.
Q: Do I need to go to a gym, or can I do resistance training at home?
A: You can absolutely train effectively at home. Bodyweight exercises, resistance bands, and basic equipment like dumbbells can provide adequate stimulus for metabolic adaptations. The key is progressive overload—consistently challenging your muscles with increasing resistance over time.
Q: Will resistance training help with weight loss?
A: Resistance training often produces favorable body composition changes—increasing muscle while decreasing fat—even if overall weight doesn't change dramatically. Muscle tissue is metabolically active and burns more calories at rest than fat tissue. The metabolic improvements occur regardless of weight loss, though combining resistance training with appropriate nutrition enhances fat loss.
Q: How do I know if I'm working out at the right intensity?
A: For metabolic benefits, aim for moderate to high intensity where you can complete 8-12 repetitions before reaching muscle fatigue. The last 2-3 repetitions should feel challenging but not impossible. If you can easily do 15+ repetitions, increase the resistance. Consider working with a qualified trainer initially to learn proper form and intensity.
Q: What role does protein intake play in maximizing benefits?
A: Adequate protein (1.6-2.2g per kg of body weight daily) supports muscle protein synthesis and recovery. Distributing protein intake across meals (20-40g per meal) optimizes muscle building. This is particularly important for older adults who have reduced muscle protein synthesis efficiency.
Take Action: Your Next Steps Toward Metabolic Transformation
The science is clear and compelling: resistance training is one of the most powerful interventions available for type 2 diabetes and metabolic health. But knowledge without action changes nothing. Here's how to start your transformation today:
Start This Week
Schedule your first session: Block out three 45-minute time slots in your calendar this week for resistance training. Treat these appointments with the same importance as doctor's visits—because they're equally crucial for your health.
Choose your approach: Decide whether you'll join a gym, work with a trainer, or start with home-based training. If you're new to resistance training, consider investing in 2-3 sessions with a qualified trainer to learn proper technique.
Get medical clearance: If you have existing health conditions or haven't exercised recently, consult your healthcare provider. Share this research with them—most physicians are enthusiastic about evidence-based exercise interventions.
Build Your Foundation
Master the basics: Focus initially on compound movements that work multiple muscle groups: squats, deadlifts, presses, rows, and core exercises. These provide maximum metabolic benefit.
Track your progress: Monitor not just your workouts but also your blood glucose patterns, how you feel, energy levels, and sleep quality. You'll likely notice improvements beyond just blood sugar.
Optimize your nutrition: Ensure adequate protein intake and maintain consistent meal timing to support your training and blood sugar management
.
Commit to the Long Game
Think in months, not weeks: The cellular and molecular adaptations we've discussed develop over time. Commit to at least 12 weeks before evaluating results—though you'll likely feel better much sooner.
Join a community: Whether it's a gym, online forum, or local diabetes support group with an exercise focus, social support dramatically improves adherence.
Educate yourself continuously: The research in this field is evolving rapidly. Stay informed about new findings, but remember: the fundamentals we've covered remain rock-solid.
Your Muscles Are Waiting
Every day you delay starting resistance training is a day your muscle stem cells remain dormant, your myokine secretion stays suboptimal, and your insulin sensitivity doesn't improve. But here's the encouraging truth: your muscles retain the remarkable capacity to adapt, regenerate, and transform your metabolic health regardless of your current condition.
The research reviewed here—from the endocrine functions of muscle to stem cell activation, from molecular reprogramming to comprehensive metabolic benefits—all points to the same conclusion: resistance training is not optional for metabolic health. It's essential.
Your body is capable of extraordinary adaptation. Your muscles are sophisticated endocrine organs waiting to optimize your metabolism. The question isn't whether resistance training works—the science proves it does. The question is: when will you start?
Make today day one. Your metabolically transformed future self will thank you.
Medical Disclaimer
The information in this article, including the research findings, is for educational purposes only and does not constitute medical advice, diagnosis, or treatment. Before starting any new strength training exercise program, you must consult with a qualified healthcare professional, especially if you have existing health conditions (such as cardiovascular disease, uncontrolled hypertension, or advanced metabolic disease). Exercise carries inherent risks, and you assume full responsibility for your actions. This article does not establish a doctor-patient relationship.
Related Articles
Is a Functional Cure for Diabetes Within Reach? The Science of Beta-Cell Restoration | DR T S DIDWAL
Dietary Protein and Glycemic Control: Evidence from the Latest Diabetes Research | DR T S DIDWAL
The Metabolic Triad: Why Diabetes, Obesity & CVD Are One Epidemic | DR T S DIDWAL
What’s New in the 2025 Blood Pressure Guidelines? A Complete Scientific Breakdown | DR T S DIDWAL
Manage Diabetes Naturally: How Beta-Glucans Control Blood Sugar | DR T S DIDWAL
Exercise as Metabolic Medicine: Latest Research on Glucose and Heart Health| DR T S DIDWAL
References
Fukada, S.-I., & Nakamura, A. (2021). Exercise/resistance training and muscle stem cells. Endocrinology and Metabolism, 36(4), 737–744. https://doi.org/10.3803/EnM.2021.401
Iglesias, P. (2025). Muscle in endocrinology: From skeletal muscle hormone regulation to myokine secretion and its implications in endocrine-metabolic diseases. Journal of Clinical Medicine, 14(13), 4490. https://doi.org/10.3390/jcm14134490
Masuda, S., & Matsuzaka, T. (2025). Insulin resistance and exercise-induced insulin sensitization in skeletal muscle: Insights from personalized phosphoproteomics. Journal of Diabetes Investigation, 16, Article e70113. https://doi.org/10.1111/jdi.70113
Wang, J., Fan, S., & Wang, J. (2025). Resistance training enhances metabolic and muscular health and reduces systemic inflammation in middle-aged and older adults with type 2 diabetes: A meta-analysis. Diabetes Research and Clinical Practice, 229, 112941. https://doi.org/10.1016/j.diabres.2025.112941
Zierath, J. R., Brady, A. J., Macgregor, K. A., Ortiz de Zevallos, J., & Stocks, B. (2025). Unlocking the secrets of exercise: A pathway to enhanced insulin sensitivity and skeletal muscle health in type 2 diabetes. Journal of Sport and Health Science, 14, Article 100980. https://doi.org/10.1016/j.jshs.2024.100980