MASLD Nutrition Plan: How the Right Foods Heal Fatty Liver
Can you actually reverse fatty liver? Discover the evidence-based MASLD diet strategies that target liver fat at the source and restore your metabolic health naturally
METABOLISM
Dr. T.S. Didwal, M.D.(Internal Medicine)
2/17/202613 min read
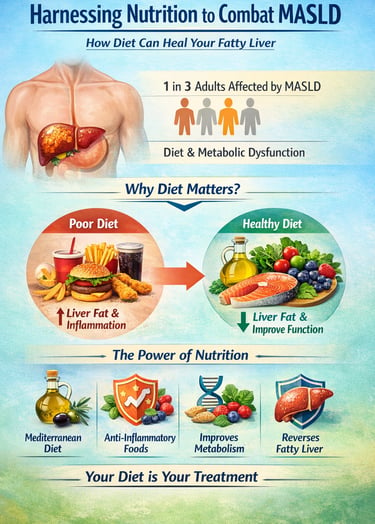
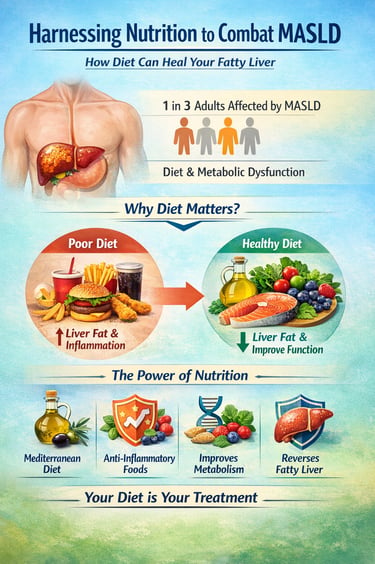
Metabolic dysfunction‑associated steatotic liver disease (MASLD) is rapidly emerging as the most common chronic liver condition worldwide, affecting an estimated one in three adults and closely linked to obesity, insulin resistance, and metabolic dysfunction (Zeng et al., 2024). Unlike traditional fatty liver classifications, MASLD places metabolic health at the center, highlighting that excess liver fat isn’t a cosmetic issue—it’s a metabolic crisis with systemic consequences. Fortunately, mounting evidence now shows that dietary intervention isn’t just supportive; it is foundational to reversing liver fat and restoring metabolic function (c Recent international consensus strongly emphasizes nutrition as first‑line therapy in MASLD management, often producing meaningful improvements in hepatic fat content and metabolic biomarkers even before medications are considered (Zeng et al., 2024). Scientific research identifies specific dietary patterns—especially the Mediterranean diet rich in whole grains, legumes, vegetables, olive oil, and fatty fish—as superior in reducing liver fat, improving insulin sensitivity, and mitigating inflammation associated with MASLD progression (Reytor‑González et al., 2025). Beyond overall patterns, particular food components such as soluble fiber, polyphenol‑rich fruits, and choline‑dense foods exert measurable hepatoprotective effects through biochemical pathways that reduce oxidative stress and improve lipid metabolism (Lamba & Bhavana, 2025). Importantly, the quality of what you eat—food sources, micronutrient density, and beverage choices—can outweigh simple calorie counts in determining liver outcomes. With MASLD now recognized as a metabolic disease, optimizing food intake becomes a powerful therapeutic strategy, capable of not only slowing progression but reversing liver fat accumulation and improving long‑term health.
Clinical pearls
1. The Fructose "Metabolic Trap"
Scientific Perspective: Unlike glucose, which is metabolized systemically, fructose is almost exclusively processed in the liver. High-fructose intake triggers de novo lipogenesis (the creation of new fat) and causes a rapid drop in hepatic ATP (energy), leading to oxidative stress and mitochondrial dysfunction.
Think of liquid sugar as "express delivery" fat for your liver. While your muscles can use regular sugar for energy, your liver has to do all the work to process fructose. Cutting out sodas and sweetened juices is the single fastest way to take the pressure off your liver cells.
2. Fiber as a "Metabolic Filter"
Scientific Perspective: High-viscosity soluble fiber (found in oats and legumes) modulates the gut-liver axis by slowing gastric emptying and reducing the absorption of bile acids. This forces the liver to use internal cholesterol stores to synthesize new bile, effectively lowering systemic lipid levels and improving insulin sensitivity.
Fiber acts like a "speed bump" for your digestion. It prevents sugar and fat from hitting your liver all at once. By eating more beans, lentils, and oats, you’re essentially giving your liver a "filter" that keeps it from being overwhelmed after a meal.
3. The Choline Connection
Scientific Perspective: Choline is a precursor to phosphatidylcholine, which is essential for the assembly and secretion of Very Low-Density Lipoproteins (VLDL). Without adequate choline, the liver cannot "export" fat, leading to intrahepatic accumulation even if you are eating a low-calorie diet.
Your liver needs a "taxi service" to move fat out of its cells and into the rest of your body. Choline (found in eggs and fish) is that taxi. If you don't get enough choline, the fat gets stuck at the station (your liver), leading to buildup even if you're trying to eat healthy.
4. Coffee: The Surprising Hepatoprotective Agent
Scientific Perspective: Coffee consumption is inversely associated with the severity of MASLD. Caffeine and its metabolite, paraxanthine, inhibit the expression of TGF-$\beta$, a key driver of hepatic stellate cell activation and fibrosis. Additionally, coffee polyphenols like chlorogenic acid reduce hepatic inflammation.
Your morning coffee is more than just a caffeine boost; it’s actually a "protective shield" for your liver. Studies show that 3 to 4 cups of coffee a day can help prevent liver scarring. As long as you don't load it with sugar and cream, it's one of the most effective "medicines" in your kitchen.
5. The "10% Rule" for Fibrosis Reversal
Scientific Perspective: While a 5% weight loss can reduce hepatic steatosis (fat), a minimum of 10% total body weight loss is typically required to induce regression of fibrosis (scarring) and improvement in MASH (inflammation). This threshold is critical for moving beyond symptom management into true disease reversal.
If you want to not only stop the disease but actually reverse it, aim for the 10% mark. Losing 5% of your weight cleans out the fat, but hitting 10% is like a "reset button" that allows your liver to start healing the deeper inflammation and scarring.
Why Diet Matters More Than Ever for Liver Health
If you've recently been diagnosed with metabolic dysfunction-associated fatty liver disease (MASLD), you're not alone. Millions of people worldwide are discovering that their livers are silently accumulating excess fat—often without any noticeable symptoms. The good news? Recent international research reveals that dietary modification isn't just helpful; it's transformative. In fact, leading health organizations now recognize nutrition as a foundational pillar in both preventing and managing this increasingly common condition.
But here's the challenge: With conflicting nutrition advice everywhere, understanding exactly what to eat and why can feel overwhelming. That's where this guide comes in. We've synthesized cutting-edge research from leading international experts to show you how food-based therapeutic strategies can genuinely improve your liver health and metabolic function.
Understanding MASLD: The Silent Metabolic Crisis
Before we dive into dietary solutions, let's clarify what MASLD actually is and why it deserves your attention.
Metabolic dysfunction-associated fatty liver disease represents a fundamental shift in how we understand fatty liver conditions. Unlike previous classifications, MASLD focuses on the metabolic dysfunction underlying fat accumulation rather than simply the absence of excess alcohol consumption. This distinction matters because it opens the door to metabolic intervention—and diet is your most powerful metabolic tool.
The condition exists on a spectrum, from simple hepatic steatosis (fatty infiltration) to metabolic dysfunction-associated steatohepatitis (MASHALTER), where inflammation and liver injury occur. Early detection and dietary intervention can prevent progression to more severe stages, including fibrosis and cirrhosis.
The Research Breakthrough: What International Experts Now Recommend
Three landmark studies published in 2024-2025 have fundamentally shaped our understanding of dietary management for MASLD. Let's explore each one and what their findings mean for you.
Study 1: The International Multidisciplinary Expert Consensus (2024)
This comprehensive consensus by Zeng et al., (2024).represents the most authoritative guidance on MASLD dietary management to date. The research team examined decades of clinical evidence to establish unified recommendations applicable across diverse populations and healthcare systems.
Key Takeaways:
Dietary modification stands as primary therapy: The consensus emphasizes that nutritional intervention should be the first-line approach before pharmaceutical interventions, even in moderate cases
Weight loss remains critical: A 5-10% reduction in body weight demonstrates meaningful improvements in liver histology and metabolic markers, with greater benefits at 10-15% weight loss
Macronutrient composition matters significantly: The type of carbohydrates, fats, and proteins consumed has distinct impacts on liver fat accumulation and insulin resistance
Sustainable dietary patterns outperform restrictive diets: Long-term adherence trumps short-term intensity in achieving lasting metabolic benefits
Personalization is essential: One-size-fits-all approaches are less effective than tailored nutritional strategies accounting for individual metabolic profiles, cultural preferences, and lifestyle factors
The consensus identifies several dietary patterns with robust evidence, which we'll explore in detail below.
Study 2: Optimising Dietary Interventions for MASLD—A Nutritional Perspective (2025)
Recent research by Lamba & Bhavana (2025).focuses specifically on the nutritional science underpinning MASLD management, examining how specific micronutrients, fiber types, and food components directly influence liver pathology.
Key Takeaways:
Micronutrient status significantly affects outcomes: Deficiencies in vitamin E, vitamin D, selenium, and choline are common in MASLD patients and correcting these deficiencies supports hepatic function and reduces oxidative stress
Fiber composition is nuanced: Not all fiber is created equal—soluble fiber from sources like oats and legumes demonstrates superior benefits for metabolic dysfunction compared to insoluble fiber alone
Polyphenol-rich foods provide anti-inflammatory protection: Foods containing high levels of polyphenols (found in berries, coffee, tea, and olive oil) actively reduce liver inflammation through multiple biochemical pathways
Dietary timing and meal frequency matter: Spreading nutrients across more frequent, smaller meals may optimize insulin sensitivity and metabolic flexibility better than traditional three-meal patterns
Hydration and beverage choices impact liver recovery: Replacing sugar-sweetened beverages with water, herbal teas, and coffee (3-4 cups daily showed benefits) accelerates metabolic improvements
The research particularly highlights the role of choline-rich foods (eggs, fish, cruciferous vegetables) and omega-3 fatty acids in reducing hepatic inflammation and improving lipid metabolism.
Study 3: Harnessing Nutrition to Combat MASLD—Food-Based Therapeutic Strategies (2025)
This study by Reytor‑González et al.,(2025) bridges the gap between nutritional science and practical implementation, examining specific whole foods and dietary patterns that demonstrate clinical efficacy in MASLD prevention and management.
Key Takeaways:
Mediterranean-style dietary patterns lead evidence: The Mediterranean diet, rich in olive oil, fish, legumes, whole grains, and vegetables, consistently outperforms other dietary approaches in reducing liver fat and improving fibrosis markers
Intermittent fasting shows promise but requires monitoring: Time-restricted eating and intermittent fasting protocols demonstrate benefits for weight loss and metabolic improvement in MASLD, though adherence challenges and individual variability require careful supervision
Ultra-processed foods accelerate disease progression: Beyond simple calorie excess, the inflammatory additives, refined sugars, and unhealthy fats in processed foods directly promote hepatic steatosis independent of weight
Plant-based proteins offer metabolic advantages: Legume-based proteins, when compared to processed meat sources, improve insulin sensitivity and reduce systemic inflammation more effectively
Specific culinary herbs and spices provide active medicinal benefits: Components like curcumin (turmeric), allicin (garlic), capsaicin (chili), and gingerol (ginger) demonstrate direct hepatoprotective and anti-inflammatory properties
Now that we understand the research foundation, let's translate this into actionable guidance. Based on the three landmark studies, here's what an evidence-based MASLD dietary approach looks like:
The Mediterranean Foundation
The research is unequivocal: the Mediterranean diet represents your best evidence-based foundation. This dietary pattern emphasizes:
Extra virgin olive oil as the primary fat source (with its unique polyphenol content)
Fatty fish (salmon, sardines, mackerel) 2-3 times weekly for omega-3 fatty acids
Plant-based proteins, including legumes, chickpeas, lentils, and beans
Whole grains (not refined carbohydrates) like farro, barley, and brown rice
Abundant vegetables consumed with olive oil-based dressings
Nuts and seeds as snacks and salad components
Moderate dairy from fermented sources like yogurt and cheese
Limited red meat consumption
Why it works: The Mediterranean pattern simultaneously addresses multiple pathogenic mechanisms—reducing oxidative stress, improving insulin sensitivity, supporting lipid metabolism, and promoting beneficial gut microbiota.
Strategic Macronutrient Distribution
The consensus research suggests:
Carbohydrates (40-50% of calories):
Prioritize low glycemic index sources
Emphasize whole grains, legumes, vegetables, and fruits
Minimize refined sugars, white bread, pastries, and sugary beverages
Include fiber-rich foods targeting 30-40g daily
Fats (25-35% of calories):
Emphasize monounsaturated fats from olive oil, avocados, and nuts
Include polyunsaturated fats from fish and plant sources
Limit saturated fats to less than 10% of total calories
Avoid trans fats entirely (industrial and processed sources)
Protein (15-25% of calories):
Emphasize lean fish, poultry, legumes, and plant proteins
Include eggs for their unique choline content
Moderate dairy intake from fermented sources
Minimize processed meats associated with inflammatory markers
Micronutrient Optimization
Given that MASLD patients frequently exhibit micronutrient deficiencies, targeted inclusion of the following is critical:
Vitamin E Sources:
Nuts and seeds (almonds, sunflower seeds)
Vegetable oils (olive oil, sunflower oil)
Leafy greens (spinach, kale)
Vitamin D and Selenium:
Fatty fish (sardines, salmon, mackerel)
Eggs (particularly yolks)
Mushrooms exposed to sunlight
Choline-Rich Foods:
Eggs (especially yolks)
Fish and shellfish
Cruciferous vegetables (broccoli, Brussels sprouts)
Legumes
Polyphenol-Rich Foods:
Berries (blueberries, raspberries, strawberries)
Grapes and red wine (moderate, up to 1-2 glasses daily)
Coffee and tea (3-4 cups daily associated with benefits)
Dark chocolate (70%+ cacao)
Olive oil
Strategic Beverage Choices
Research increasingly demonstrates that beverage selection profoundly impacts metabolic outcomes:
Water: Your primary beverage—aim for adequate hydration
Coffee: 3-4 cups daily showed inverse association with liver fibrosis
Tea: Both green and black tea contain beneficial polyphenols and catechins
Limit or eliminate: Sugar-sweetened beverages, high-fructose drinks, excessive alcoho
Special Considerations: Weight Loss and Adherence
The research is clear: weight loss remains the most powerful dietary intervention for MASLD improvement. However, the how and how much matter significantly.
Target Weight Loss
5-10% reduction: Demonstrates measurable improvements in liver fat content and metabolic markers
10-15% reduction: Produces more substantial improvements, potentially reversing fibrosis in some cases
Pace matters: Gradual loss (0.5-1kg weekly) proves more sustainable and metabolically healthier than rapid loss
Achieving Sustainable Adherence
The consensus research emphasizes that the "best diet is the one you'll actually follow." Consider these evidence-backed adherence strategies:
Align with cultural preferences: Mediterranean patterns can be adapted to various cultural dietary traditions
Build social support: Family involvement and group-based interventions improve adherence
Work with specialists: Registered dietitian nutritionists provide superior outcomes compared to generic nutrition advice
Set realistic, phased goals: Rather than complete dietary overhaul, implement changes progressively
Address behavioral patterns: Many MASLD patients benefit from counseling addressing emotional eating and lifestyle factors
Frequently Asked Questions (FAQs)
Q1: Can diet alone cure MASLD, or do I need medication?
A: For many patients, particularly those with early-stage disease, dietary modification as the primary intervention can substantially improve or even reverse MASLD. However, progression and individual variation mean some patients may ultimately require pharmacological support. The key is implementing dietary changes promptly—earlier intervention yields better outcomes. Discuss with your hepatologist whether your specific situation warrants medication alongside dietary management.
Q2: What about intermittent fasting or keto diets for MASLD?
A: The research shows intermittent fasting can support weight loss and metabolic improvement, though data specific to MASLD is limited and adherence challenges are common. Ketogenic diets show mixed evidence—while rapid weight loss may benefit some patients, the high saturated fat content concerns many specialists. The Mediterranean diet, with more robust evidence, should form your foundation; intermittent fasting might be considered as an adjunct under professional supervision, but shouldn't replace a fundamentally sound dietary pattern.
Q3: How quickly will I see improvements?
A: Early metabolic improvements (improved fasting glucose, insulin levels, and lipid profiles) may appear within weeks of dietary changes. Liver fat reduction typically becomes evident on imaging within 2-3 months of sustained dietary improvement. More substantial improvements in fibrosis markers may take 6-12 months or longer. Patience combined with consistency yields the best results.
Q4: Are supplements necessary if I'm following a good diet?
A: Whole foods should form the foundation of your nutritional intake. However, depending on your specific micronutrient status and dietary restrictions, targeted supplementation may be beneficial—particularly vitamin D, vitamin E, or choline, if you're unable to obtain adequate amounts from food. Testing specific micronutrient levels through your healthcare provider can guide supplementation decisions, preventing unnecessary supplementation.
Q5: I love alcohol—do I need to eliminate it completely?
A: While MASLD differs from alcohol-associated fatty liver disease (ALD), alcohol still impacts metabolic function and liver health. Current guidance suggests limiting alcohol significantly: moderate consumption (up to 1-2 drinks daily for women, 2-3 for men) might be acceptable for some with well-controlled MASLD, though abstinence is safest. Discuss your individual alcohol use with your healthcare provider—some patients benefit from complete elimination.
Q6: What if I have food allergies or cultural dietary restrictions?
A: The Mediterranean diet can be successfully adapted to nearly all dietary restrictions and cultural traditions. Work with a registered dietitian familiar with both MASLD and your specific dietary needs to identify culturally congruent alternatives that maintain the pattern's therapeutic benefits.
Key Takeaways: Your MASLD Dietary Action Plan
Unlike many chronic diseases, MASLD offers a powerful therapeutic entry point: nutrition.
The 2024 international expert consensus positions dietary modification as first-line therapy—often before pharmacologic escalation. This marks a paradigm shift. Diet is no longer supportive advice; it is core treatment. Emerging 2024–2025 evidence confirms that specific dietary patterns can directly reduce hepatic fat, improve insulin sensitivity, attenuate oxidative stress, and even reverse early fibrosis when meaningful weight loss is achieved.
The Mediterranean Pattern: The Strongest Evidence Base
Across diverse populations, the Mediterranean diet consistently outperforms other dietary strategies in reducing liver fat and improving metabolic markers. Its benefits extend beyond calorie control.
Key components include:
Extra-virgin olive oil (rich in monounsaturated fats and polyphenols)
Fatty fish (omega-3 fatty acids for anti-inflammatory action)
Legumes and whole grains (high in soluble fiber)
Nuts and seeds (antioxidant density)
Vegetables and berries (micronutrients and polyphenols)
Fermented dairy (gut microbiome support)
This pattern simultaneously reduces oxidative stress, enhances insulin signaling, supports lipid export, and promotes a healthier gut-liver axis.
Most importantly, it is sustainable. Long-term adherence determines histologic improvement—not short-term dietary intensity.
The Fructose Metabolic Trap
One of the most actionable insights in MASLD management is the impact of fructose.
Unlike glucose, fructose is primarily metabolized in the liver, where it drives de novo lipogenesis (DNL). Excess intake—especially from sugar-sweetened beverages—increases hepatic triglyceride synthesis, depletes ATP, and promotes mitochondrial dysfunction.
The simplest intervention: eliminate liquid sugar.
Removing sodas, sweetened juices, and high-fructose drinks rapidly reduces hepatic fat flux and metabolic stress. In MASLD, beverage quality is as critical as macronutrient composition.
Fiber as a Metabolic Filter
Not all carbohydrates are metabolically equivalent. High-viscosity soluble fiber—found in oats, lentils, beans, and certain fruits—slows gastric emptying, reduces postprandial glucose spikes, and improves insulin sensitivity.
Fiber also influences bile acid metabolism, compelling the liver to use internal cholesterol stores, thereby improving lipid profiles. Through modulation of the gut microbiome, fiber reduces inflammatory signaling along the gut-liver axis.
In MASLD, fiber functions as a metabolic buffer, preventing postprandial overload.
The Choline Connection
An underappreciated nutrient in MASLD is choline.
Choline is required for the synthesis of phosphatidylcholine, essential for VLDL assembly and secretion. Without adequate choline, hepatocytes cannot efficiently export triglycerides, leading to intrahepatic fat accumulation—even in calorie-restricted states.
Dietary sources include:
Eggs (especially yolks)
Fish and shellfish
Legumes
Cruciferous vegetables
Ensuring adequate choline intake supports proper lipid transport and hepatic recovery.
Coffee: A Hepatoprotective Signal
Few dietary exposures show as consistent a protective signal as coffee.
Bioactive compounds—caffeine, paraxanthine, and chlorogenic acid—modulate TGF-β signaling and reduce hepatic stellate cell activation, limiting fibrosis progression. Observational data link 3–4 cups daily with lower risk of advanced liver scarring.
When consumed without excess sugar or cream, coffee functions as a natural anti-fibrotic adjunct.
The 10% Rule: Weight Loss for Fibrosis Reversal
While nutrient quality matters, weight loss remains the strongest determinant of disease reversal.
5% weight loss → reduction in hepatic steatosis
≥10% weight loss → improvement in fibrosis and MASH
Gradual reduction (0.5–1 kg per week) promotes sustainable metabolic adaptation. Rapid, unsustainable dieting undermines long-term benefit.
The threshold is clear: 10% represents metabolic reset territory.
Personalization and Sustainability
The international consensus emphasizes precision nutrition. Cultural adaptation, behavioral support, and professional guidance from a registered dietitian improve adherence and outcomes.
The “best” diet is one that is:
Metabolically effective
Culturally adaptable
Psychologically sustainable
Consistency—rather than perfection—determines long-term success.
From Lifestyle Advice to Foundational Therapy
MASLD is fundamentally a metabolic disease expressed in the liver. Its treatment must therefore correct metabolic dysfunction at the source.
Evidence from 2024–2025 is unequivocal:
Adopt a Mediterranean-style pattern
Eliminate fructose-laden beverages
Ensure adequate fiber and choline
Prioritize polyphenols and omega-3 fatty acids
Achieve and sustain ≥10% weight loss
Pharmacologic therapies may complement care in selected patients, but without nutritional correction, long-term reversal remains unlikely.
In MASLD management, food is regulatory input. It influences gene expression, mitochondrial function, lipid export, and inflammatory signaling. It determines whether the liver accumulates fat—or restores metabolic balance.
Author's note:
The content synthesizes current international research, expert consensus, and peer-reviewed clinical studies to provide evidence-based guidance on managing metabolic dysfunction-associated steatotic liver disease (MASLD) through dietary strategies. Recommendations focus on whole-food, nutrient-rich dietary patterns, emphasizing the Mediterranean diet, targeted micronutrient optimization, and sustainable, personalized lifestyle interventions. While the information presented is grounded in rigorous scientific evidence, it is educational and informational in nature and is not a substitute for individualized medical advice. Readers are strongly encouraged to consult their hepatologist, registered dietitian, or healthcare provider to develop a personalized MASLD management plan tailored to their metabolic profile, comorbidities, and lifestyle. The author advocates a practical, patient-centered approach, recognizing that consistent, evidence-based dietary changes are among the most effective interventions for reversing liver fat, improving insulin sensitivity, and supporting long-term metabolic health.
Medical Disclaimer
The information in this article, including the research findings, is for educational purposes only and does not constitute medical advice, diagnosis, or treatment.
Related Articles
Metabolic Plasticity: Epigenetic Adaptations to Calorie Restriction | DR T S DIDWAL
References
Lamba, S., & Bhavana, S. (2025). Optimising dietary interventions for MASLD: A nutritional perspective on liver health. International Journal for Multidisciplinary Research (IJFMR), 7(3), 1–15. https://doi.org/10.36948/ijfmr.2025.v07i03.46465
Pickett-Blakely, O. (2024). MASLD and diet: Revolutionizing care with tailored nutritional strategies [Conference or educational presentation]. American Society for Nutrition. https://nutrition.org/wp-content/uploads/2024/06/Octavia_ASN2024_MASLDandDiet.pdf
Reytor-González, C., Simancas-Racines, D., Campuzano-Donoso, M., Castano Jimenez, J., Román-Galeano, N. M., Sarno, G., & Frias-Toral, E. (2025). Harnessing nutrition to combat MASLD: A comprehensive guide to food-based therapeutic strategies. Food and Agricultural Immunology, 36(1). https://doi.org/10.1080/09540105.2025.2496499
Zeng, X. F., Varady, K. A., Wang, X. D., Targher, G., Byrne, C. D., Tayyem, R., Latella, G., Bergheim, I., Valenzuela, R., George, J., Newberry, C., Zheng, J. S., George, E. S., Spearman, C. W., Kontogianni, M. D., & Zheng, M. H. (2024). The role of dietary modification in the prevention and management of metabolic dysfunction-associated fatty liver disease: An international multidisciplinary expert consensus. Metabolism: Clinical and Experimental, 161, 156028. https://doi.org/10.1016/j.metabol.2024.156028