Leptin vs. Adiponectin: How Your Fat Hormones Control Weight and Metabolic Health
Dive into the latest 2025 research on adipokines. Discover how fat cells act as an endocrine organ and how lifestyle changes can optimize leptin sensitivity and boost protective adiponectin.
METABOLISMOBESITY
Dr. T.S. Didwal, M.D.(Internal Medicine)
1/13/202611 min read
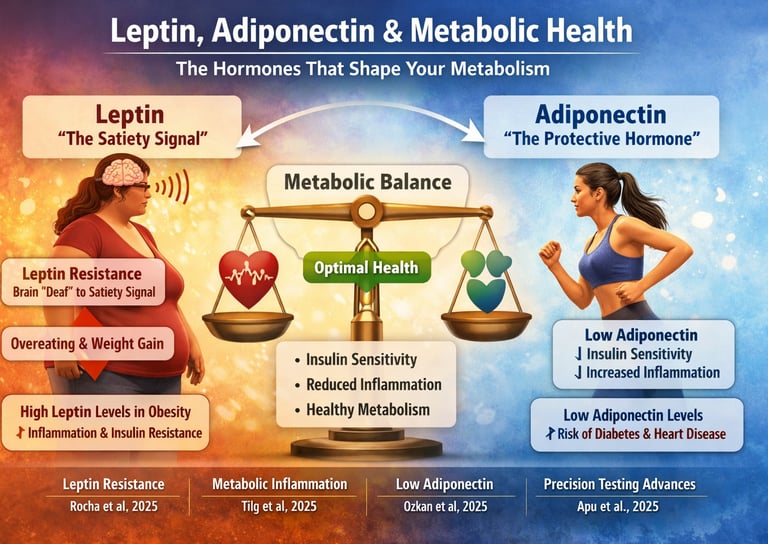
What if your body fat wasn’t just extra storage—but an intelligent communication network sending powerful biochemical messages every second? Modern research now reveals that adipose tissue is an active endocrine organ, constantly releasing hormones that influence appetite, inflammation, insulin sensitivity, and long-term metabolic health (Tilg et al., 2025). Two of the most important messengers—leptin and adiponectin—function like metabolic traffic controllers, determining whether your system flows smoothly or backs up into dysfunction.
Leptin acts as the body’s satiety signal, telling your brain when you’ve had enough to eat. But in obesity, high leptin doesn’t mean better appetite control; it often means leptin resistance, a state where the brain no longer responds to the hormone’s message (Rocha et al., 2025). This breakdown in signaling can drive overeating and ongoing weight gain, even when leptin levels are sky-high.
Adiponectin, on the other hand, protects your metabolism by enhancing insulin sensitivity and reducing inflammation. Yet paradoxically, its levels fall precisely when visceral fat increases—the time when you need it most (Ozkan et al., 2025). Low adiponectin is now recognized as an early warning signal for metabolic syndrome, prediabetes, and cardiovascular disease.
These hormonal shifts aren’t abstract laboratory findings—they’re powerful predictors of your metabolic future. As measurement technologies advance, clinicians can now evaluate these adipokines with increasing precision, allowing for more personalized prevention and treatment strategies (Apu et al., 2025). Understanding these hormones isn’t optional anymore—it’s essential for anyone serious about long-term metabolic health.
Clinical pearls
1. Adipokines as Predictive Biomarkers (Beyond BMI)
Leptin and adiponectin profiles are better predictors of future metabolic health transitions than BMI alone. Two individuals with the same Body Mass Index (BMI) can have dramatically different metabolic risks. Favorable adiponectin levels (the protective hormone) predict sustained metabolic health, while unfavorable profiles (high leptin, likely resistance) predict metabolic deterioration, independent of traditional risk factors.
Pearl: Don't rely solely on BMI; consider adipokine profiling to capture the actual biological status and predict future disease trajectory.
2. The Central Role of Leptin Resistance
In obesity, high leptin levels do not mean the body has enough satiety signaling; it indicates leptin resistance. The brain is effectively "deaf" to the high signal. This is the core metabolic dysfunction driving continued overeating and weight gain.
Pearl: The therapeutic goal for high leptin isn't to lower leptin, but to restore leptin sensitivity through interventions that improve insulin signaling (exercise, quality sleep, stress management).
3. Adiponectin is Your Metabolic Protector
Adiponectin is the "good guy" hormone that promotes insulin sensitivity and reduces chronic inflammation. Paradoxically, levels decrease as visceral fat increases, meaning the people who need its protection the most have the least of it.
Pearl: Prioritize strategies specifically known to boost adiponectin, such as aerobic exercise and anti-inflammatory nutrition. Even modest weight loss (5-10%) can yield a meaningful increase.
4. Metabolic obesity
is an Inflammatory Condition
Obesity-related disease is fundamentally a systemic inflammatory condition driven by dysfunctional adipokine signaling. Adipose tissue acts as an endocrine organ, and its dysregulation (particularly unbalanced leptin/adiponectin) orchestrates chronic low-grade inflammation.
Pearl: Interventions must address the immunometabolic link. Treatments shouldn't just target caloric restriction but should aim to restore healthy adipokine function to resolve the underlying inflammation.
5. Adipokine Levels are Modifiable
Despite genetic influences, lifestyle factors have a substantial impact on adipokine levels, demonstrating that biology is not destiny. Measurable improvements can occur relatively quickly.
Pearl: Patients can achieve measurable improvements in adiponectin within 4-12 weeks of consistent exercise and diet changes. This provides a strong, objective target and a positive feedback mechanism for encouraging sustained lifestyle adherence.
Leptin, Adiponectin, and Metabolic Health: Understanding the Hormones That Shape Your Metabolism
Understanding Leptin: The Satiety Hormone
Think of leptin as your body's appetite control center. This hormone is produced by your adipose tissue (fat cells) and travels to your brain to signal that you're full and satisfied. In theory, the more fat you have, the more leptin you should produce, and the less you should eat. Sounds straightforward, right?
But here's where it gets complicated. Many people with obesity experience what researchers call leptin resistance—a condition where despite high leptin levels, the brain doesn't respond appropriately to the signal. It's like your phone's volume is turned all the way up, but you still can't hear the ringing. This metabolic dysfunction can lead to continued overeating and weight gain, creating a vicious cycle that's difficult to break.
Leptin does more than just regulate appetite, though. This multifunctional hormone also influences energy expenditure, immune function, and reproduction. Recent research has shown that leptin concentrations correlate significantly with body fat percentage, making it a valuable marker for understanding metabolic status.
Understanding Adiponectin: The Protective Hormone
If leptin is the quantity regulator, adiponectin is the quality controller. This hormone, also secreted by fat cells, works like a metabolic protector. Unlike leptin, which increases with more body fat, adiponectin levels actually decrease as body fat percentage increases—particularly visceral fat.
Here's the remarkable part: adiponectin promotes insulin sensitivity, reduces inflammation, and protects against cardiovascular disease. It's the "good guy" hormone that we actually want more of. People with higher adiponectin concentrations tend to have better insulin sensitivity, lower inflammation markers, and reduced risk of metabolic syndrome and type 2 diabetes.
The irony is painful: those who need the most metabolic protection—people with obesity or high visceral fat—tend to have the lowest adiponectin levels. This creates a paradoxical situation where metabolic dysfunction is self-perpetuating.
The Latest Research: What Scientists Are Discovering
Study 1: Leptin, CRP, and Adiponectin in Adolescents
Rocha and colleagues (2025) conducted a comprehensive systematic review and meta-analysis examining how leptin, C-reactive protein (CRP), and adiponectin correlate with body fat percentage in adolescents. This research is particularly significant because it focuses on a critical developmental period.
Key Findings: The study revealed strong correlations between these adipokines and body composition during adolescence. Leptin concentrations showed positive associations with body fat percentage, meaning higher leptin levels correlated with increased adiposity. Meanwhile, adiponectin levels showed the expected inverse relationship—higher levels were associated with lower body fat percentages. The inflammatory marker CRP also correlated with body fat, suggesting a connection between obesity and systemic inflammation.
Why This Matters: These correlations establish that even in young people, metabolic markers like leptin and adiponectin can serve as early indicators of metabolic dysfunction. Early intervention based on these hormone levels might prevent lifelong health problems. Rocha et al. (2025) essentially provided a map for identifying adolescents at risk for future metabolic disease.
Study 2: Adipokines as Masterminds of Metabolic Inflammation
Tilg, Ianiro, Gasbarrini, and colleagues (2025) published a major review in Nature Reviews Immunology positioning adipokines as central regulators of metabolic inflammation. This research shifts our understanding of how obesity and metabolic disease develop.
Key Findings: The authors argue that leptin and adiponectin, along with other adipokines, act as "masterminds" orchestrating immune responses and inflammatory pathways. Importantly, they highlight how adipose tissue isn't just a storage depot—it's an endocrine organ producing numerous signaling molecules that influence systemic health. Dysregulation of these adipokine signals contributes to chronic low-grade inflammation characteristic of obesity and metabolic disease.
Why This Matters: This research reframes obesity from simply being "too much fat" to being a systemic inflammatory condition driven by dysfunctional adipokine signaling. Understanding obesity through an immunometabolic lens opens new therapeutic possibilities. Instead of just targeting weight loss, interventions could aim to restore healthy adipokine production and function. Tilg et al. (2025) demonstrates that metabolic inflammation is the bridge connecting adipokine dysfunction to serious health consequences.
Study 3: Adipokines and Metabolic Health Transitions
Ozkan and colleagues (2025) analyzed longitudinal data from the Atherosclerosis Risk In Communities (ARIC) Study to examine how adipokine levels predict transitions in metabolic health status over time. This large prospective study tracked real-world changes in health outcomes.
Key Findings: The research demonstrated that baseline adipokine profiles—particularly the balance between protective adiponectin and problematic leptin resistance—predicted whether individuals would maintain or lose metabolic health over follow-up periods. Individuals with favorable adiponectin levels were more likely to remain metabolically healthy, while those with unfavorable adipokine profiles experienced metabolic deterioration. The study also revealed that these adipokine markers were predictive independent of traditional risk factors like BMI.
Why This Matters: Ozkan et al. (2025) proved that adipokines aren't just correlates of health—they're predictors of future metabolic status. This suggests that monitoring leptin and adiponectin levels could enable personalized medicine approaches where individuals can receive targeted interventions before serious metabolic dysfunction develops. The research validates using adipokines as key biomarkers in clinical practice.
Study 4: Advanced Measurement of Leptin, Resistin, and Adiponectin
Apu and colleagues (2025) developed innovative multiplex assay methods using immunoaffinity enrichment and targeted mass spectrometry to measure leptin, resistin, and adiponectin with unprecedented precision. This technical advancement is crucial for future research.
Key Findings: The researchers successfully created a sensitive, specific measurement tool that can simultaneously quantify multiple adipokines from small biological samples. The assay demonstrated excellent reproducibility and correlation with clinical outcomes. This technical innovation enables more accurate adipokine profiling in research and potentially in clinical settings.
Why This Matters: Accurate measurement is foundational to personalized medicine. Apu et al. (2025) provides the technical infrastructure for the future of adipokine-based diagnostics. As these measurement techniques become more accessible and affordable, physicians could routinely assess adipokine profiles to guide treatment decisions. This represents a shift from imprecise BMI-based assessments to sophisticated biomarker-driven medicine.
Connecting the Research: The Integrated Picture
When we step back and synthesize these four studies, a cohesive narrative emerges: adipokines are central regulators of metabolic health, they can be measured with increasing precision, they predict future health status, and understanding them is essential for modern medicine.
Leptin serves as a marker of adiposity and energy status, while adiponectin acts as a protective factor promoting metabolic wellness. Their balance—and particularly the maintenance of appropriate adiponectin levels—determines whether someone remains metabolically healthy or progresses toward disease. Importantly, these aren't just markers of what's already happened; they're predictive of future health trajectories.
The research also highlights that metabolic inflammation driven by adipokine dysfunction underlies the obesity-related disease epidemic. This understanding suggests that future interventions should target adipokine restoration and not just caloric restriction.
Practical Implications: What This Means for Your Health
Why Should You Care About Your Adipokine Levels?
Your leptin and adiponectin levels are windows into your metabolic health. Unlike BMI, which simply divides weight by height, these hormones reflect what's actually happening metabolically. Two people with identical BMI could have completely different adipokine profiles and dramatically different disease risks.
Optimizing Your Adipokines
For Leptin: Since leptin resistance is such a common problem, maintaining appropriate leptin signaling requires addressing the underlying factors: regular physical activity (especially resistance training), adequate sleep, stress management, and avoiding processed foods. Interestingly, extreme calorie restriction can backfire by suppressing leptin, which is why sustainable moderate approaches work better.
For Adiponectin: Increasing adiponectin levels is achievable through aerobic exercise, maintaining healthy body composition, consuming anti-inflammatory foods (especially those rich in polyphenols), and managing blood sugar through low glycemic index foods. Weight loss, even modest losses of 5-10%, can meaningfully increase adiponectin production.
Getting Your Levels Tested
As measurement techniques improve—following innovations like those from Apu et al. (2025)—adipokine testing may become more accessible. Currently available through specialized labs, future routine medical assessments may include adipokine profiling alongside cholesterol panels. If you have metabolic risk factors (obesity, prediabetes, metabolic syndrome), discussing adipokine testing with your healthcare provider could provide valuable insights.
Frequently Asked Questions
Q: Can I lower my leptin levels if they're too high?
A: High leptin levels usually indicate leptin resistance rather than true leptin excess. The goal is restoring leptin signaling through improved insulin sensitivity, regular exercise, and quality sleep rather than lowering leptin itself.
Q: How quickly can I improve my adiponectin levels?
A: Studies show measurable improvements in adiponectin concentrations within 4-12 weeks of consistent exercise and modest weight loss. Even without weight loss, regular aerobic activity can increase adiponectin levels.
Q: Is adiponectin more important than leptin?
A: They work complementarily. Leptin signals energy availability, while adiponectin promotes metabolic protection. Both matter, but from a metabolic disease prevention perspective, maintaining adequate adiponectin may be slightly more critical.
Q: Do genetics determine my adipokine levels?
A: Genetics influence baseline adipokine production, but lifestyle factors have enormous impact. Even people genetically predisposed to lower adiponectin can improve through exercise and diet.
Q: Can supplements improve my adipokine profile?
A: Some research suggests certain supplements (curcumin, resveratrol, omega-3s) may modestly improve adiponectin levels, but lifestyle changes provide far more substantial effects.
Key Takeaways
Leptin and adiponectin are critical metabolic hormones produced by fat cells that regulate appetite, energy expenditure, and inflammatory responses
Strong correlations exist between adipokine levels and body fat percentage from adolescence onward, making them valuable metabolic markers
Adipokines function as "masterminds" controlling metabolic inflammation, linking adipokine dysfunction to obesity-related diseases
Baseline adipokine profiles predict future metabolic health transitions, suggesting they should be monitored clinically
Advanced measurement techniques now enable precise adipokine quantification, facilitating personalized medicine approaches
Lifestyle interventions—particularly regular exercise, weight management, and anti-inflammatory nutrition—effectively optimize adipokine levels
Maintaining healthy adiponectin concentrations while avoiding leptin resistance is central to long-term metabolic health
Moving Forward: Your Action Plan
Understanding leptin and adiponectin empowers you to take meaningful action for your health. Here's your practical roadmap:
Immediate Actions (This Week):
Schedule an appointment with your healthcare provider to discuss your metabolic health and whether adipokine testing is appropriate
Commit to 150 minutes of moderate aerobic activity weekly to boost adiponectin production
Prioritize sleep, aiming for 7-9 hours nightly to support leptin signaling
Short-Term Goals (Next 3 Months):
Implement anti-inflammatory eating patterns focusing on whole foods, vegetables, and lean proteins
Reduce processed food intake, which contributes to leptin resistance
Start resistance training 2-3 times weekly to optimize body composition and adipokine balance
Long-Term Vision (6+ Months):
Work toward modest weight loss if needed, knowing that even 5-10% reductions meaningfully improve adiponectin levels
Consider adipokine testing to track your progress objectively
Maintain consistent healthy habits that support optimal metabolic hormone function
Author’s Note
As a clinician and academic deeply engaged in metabolic medicine, my goal in writing this article is to bridge the gap between cutting-edge scientific research and practical, patient-centered understanding. Leptin and adiponectin are often discussed only in advanced endocrinology or research settings, yet their influence on everyday metabolic health is profound. By translating complex hormonal pathways into accessible explanations, I hope to empower both healthcare professionals and the public with knowledge that drives early detection, prevention, and more personalized intervention strategies.
The studies highlighted here—from adolescent adipokine correlations to advanced biomarker measurement technologies—represent a major shift in how we understand metabolic disease. Rather than treating obesity as a simple imbalance of calories, the emerging science underscores the intricate biology of inflammation, hormonal resistance, and endocrine signaling within adipose tissue.
My intention is not only to inform but also to inspire a more nuanced clinical approach: one that moves beyond BMI and embraces adipokine profiling as a powerful tool for predicting metabolic trajectories. As research continues to evolve, I remain committed to presenting evidence-based insights that support actionable, meaningful change in patient care and long-term wellness
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Individual circumstances vary, and treatment decisions should always be made in consultation with qualified healthcare professionals.
Related Articles
How Exercise Reverses Leptin Resistance and Restores Metabolic Health | DR T S DIDWAL
Your Body Fat Is an Endocrine Organ—And Its Hormones Shape Your Heart Health | DR T S DIDWAL
hsCRP Explained: What Inflammation Means for Your Heart | DR T S DIDWAL
What’s New in the 2025 Blood Pressure Guidelines? A Complete Scientific Breakdown | DR T S DIDWAL
Low-Fat vs. Low-Carb: Which Diet is Best for Weight Loss? | DR T S DIDWAL
5 Steps to Reverse Metabolic Syndrome: Diet, Habit, & Lifestyle Plan | DR T S DIDWAL
The Role of Cholesterol in Health and Disease: Beyond the "Bad" Label | DR T S DIDWAL
Lowering Cholesterol with Food: 4 Phases of Dietary Dyslipidemia Treatment | DR T S DIDWAL
The Best Dietary Fat Balance for Insulin Sensitivity, Inflammation, and Longevity | DR T S DIDWAL
References
Apu, J., Yang, X., Lin, T. T., Fillmore, T. L., Gritsenko, M. A., Kelly, S. S., Swensen, A. C., Shi, T., Master, S. R., DeLany, J. P., Goodpaster, B. H., Qian, W. J., & Qu, J. (2025). A multiplex assay of leptin, resistin, and adiponectin by immunoaffinity enrichment and targeted mass spectrometry. Journal of Mass Spectrometry and Advances in the Clinical Lab, 36, 11–18. https://doi.org/10.1016/j.jmsacl.2025.01.003
Ozkan, B., Zhang, S., Echouffo-Tcheugui, J. B., Florido, R., Nambi, V., Michos, E. D., Abushamat, L. A., Matsushita, K., Gerstenblith, G., Blumenthal, R. S., Hoogeveen, R., Ballantyne, C. M., Coresh, J., Selvin, E., & Ndumele, C. E. (2025). Adipokines and transitions in metabolic health over time: The Atherosclerosis Risk In Communities (ARIC) Study. The Journal of Clinical Endocrinology and Metabolism, 110(9), e2939–e2945. https://doi.org/10.1210/clinem/dgae916
Rocha, A. R. F., de Morais, N. S., Azevedo, F. M., Morais, D. C., Pereira, P. F., Peluzio, M. D. C. G., Franceschini, S. D. C. C., & Priore, S. E. (2025). Leptin, CRP, and adiponectin correlate with body fat percentage in adolescents: Systematic review and meta-analysis. Frontiers in Nutrition, 12, 1560080. https://doi.org/10.3389/fnut.2025.1560080
Tilg, H., Ianiro, G., Gasbarrini, A., & colleagues. (2025). Adipokines: Masterminds of metabolic inflammation. Nature Reviews Immunology, 25, 250–265. https://doi.org/10.1038/s41577-024-01103-8