Is Meat Actually Bad for Your Heart? Evidence from Latest Nutrition Science
Think you know the truth about meat and heart health? Explore new 2025 nutrition evidence that challenges diet myths and reveals the heart-healthy balance that really matters.
NUTRITION
Dr. T.S. Didwal, M.D.(Internal Medicine)
1/1/202617 min read
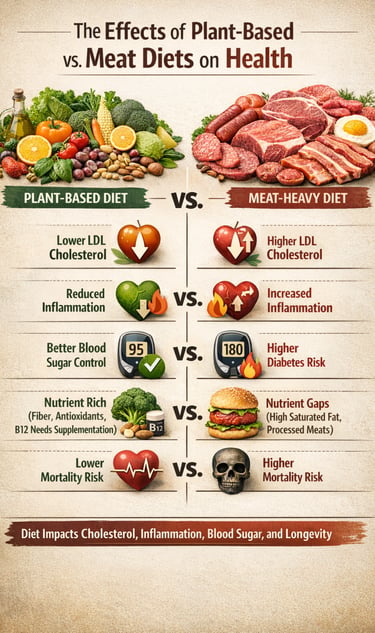
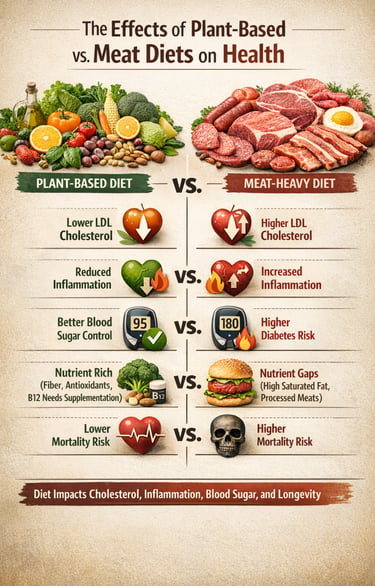
Heart disease remains the leading cause of death worldwide, and diet is one of the most modifiable factors influencing cardiovascular risk (Ma et al., 2025). For decades, meat consumption has been at the center of a heated debate, with conflicting claims about its impact on cholesterol, inflammation, and long-term heart health. Recent 2025 evidence suggests the truth is more nuanced than blanket recommendations for or against meat. While some studies link frequent intake of processed meats to elevated LDL cholesterol and higher markers of systemic inflammation, moderate consumption of lean, unprocessed meats appears compatible with a heart-healthy diet (Kadire & Desai, 2024; Fernández-Rodríguez et al., 2025). Simultaneously, plant-based dietary patterns—rich in vegetables, legumes, whole grains, and nuts—consistently demonstrate favorable effects on lipid profiles, oxidative stress, and inflammatory biomarkers (Austin et al., 2025; Chakole et al., 2025). Understanding the balance of protein sources, nutrient quality, and portion size is crucial for optimizing cardiovascular outcomes. This evidence-based exploration will guide you through the latest findings on meat, plant-based alternatives, and diet quality, helping you make informed decisions to protect your heart, improve metabolic markers, and reduce your long-term risk of cardiovascular disease.
This comprehensive guide examines six major studies published in 2025, exploring everything from plant-based meat alternatives to the real-world nutritional outcomes of different dietary patterns. Let's dive into what science actually says about your plate.
Clinical pearls .
1. Aim for a 1:2 Protein Ratio
One of the most significant findings in 2025 is the "Heart-Healthy Ratio." While the average person consumes about 1 part plant protein to 3 parts animal protein, researchers found a tipping point for heart protection.
The Pearl: You don't have to go 100% vegan to see major benefits. Shifting your ratio to at least 1:2 (one gram of plant protein for every two grams of animal protein) can lower your risk of heart disease by nearly 20%. Think of it as "crowding out" meat rather than "cutting it out."
2. The "Processing Paradox" of Meat Substitutes
2025 research confirms that plant-based meat alternatives (PBMAs) like burgers and sausages can lower your "bad" LDL cholesterol, but they aren't a free pass for heart health.
The Pearl: Many meat substitutes are "salt traps." While they are better for your cholesterol than a beef burger, the high sodium content can strain your blood pressure. When choosing these, look for the "Low Sodium" label and treat them as a transition tool, not a health food staple.
3. "Plant-Rich" is More Powerful Than "Plant-Only"
A major 2025 meta-analysis shifted the terminology from "plant-based" to "plant-rich." This reflects the fact that a diet filled with diverse plants—even if it includes some fish or lean meat—often outperforms a strict vegan diet that relies on refined grains.
The Pearl: Focus on plant diversity. Aim for 30 different types of plants per week (including spices, nuts, and seeds). This variety feeds a more diverse gut microbiome, which acts as an internal pharmacy, producing anti-inflammatory compounds that protect your arteries.
4. The B12 and Bone Health Check
New long-term data from 2025 warns that while plant-based eaters have lower heart risk, they may face a higher risk of bone fractures if they aren't careful.
The Pearl: If you choose a strictly plant-based path, Vitamin B12 and Calcium are non-negotiable. Without B12, you risk nerve damage and fatigue; without intentional calcium and Vitamin D, bone density can drop. If you aren't eating dairy or eggs, ensure you are using fortified milks or a high-quality supplement.
5. Prioritize "Heme-Free" Days
Recent studies show that the "Heme Iron" found in red meat can promote oxidative stress—a fancy way of saying it causes internal "rusting" in your blood vessels.
The Pearl: You don't need to quit steak forever, but practicing "Heme-Free" days (where your protein comes only from beans, lentils, or tofu) gives your body a break from this oxidative load. This is why the Mediterranean diet—which limits red meat to a few times a month—remains the gold standard for longevity.
6. Inflammation is the "Invisible Scoreboard"
2025 research highlights that the real benefit of plant-heavy diets isn't just lower weight—it's lower systemic inflammation, measured by a marker called hs-CRP.
The Pearl: If you feel sluggish or have joint aches after heavy meat-based meals, it may be a sign of diet-induced inflammation. Moving toward plant-based proteins acts like an "anti-inflammatory cooling system" for your body. The goal of your diet should be to keep your "internal fire" (inflammation) low, which you can track through simple blood tests with your doctor.
Understanding the Current Landscape: Why Diet Matters More Than Ever
Cardiovascular disease remains the leading cause of death globally, and diet plays a crucial role in either preventing or promoting heart-related conditions. With the rise of plant-based eating patterns and innovative meat substitutes, consumers face more choices—and confusion—than ever before.
The studies we'll explore today address critical questions:
Do plant-based meat alternatives actually improve heart health?
Is meat consumption as dangerous as some headlines suggest?
What nutritional deficiencies might vegetarians face?
How do different dietary patterns affect inflammation and cholesterol?
Let's examine the evidence systematically.
Study #1: Plant-Based Meat Alternatives Show Promising Heart Health Benefits
The Research Breakthrough
Fernández-Rodríguez et al. (2025) conducted a comprehensive systematic review and meta-analysis examining how plant-based meat alternatives (PBMAs) affect cardiometabolic health markers. Published in The American Journal of Clinical Nutrition, this study represents one of the most thorough examinations of meat substitutes to date.
Key Findings
The researchers analyzed multiple randomized controlled trials and observational studies, focusing on how replacing traditional meat with plant-based alternatives affects:
LDL cholesterol levels (the "bad" cholesterol)
Blood pressure measurements
Body weight and BMI
Blood sugar control
Inflammatory markers
The results were encouraging. Participants who substituted conventional meat with plant-based meat products showed statistically significant improvements in several cardiovascular risk factors. Specifically, LDL cholesterol decreased, suggesting a potential protective effect against atherosclerosis and coronary heart disease.
What This Means for You
If you're considering incorporating meat alternatives like Beyond Meat, Impossible Foods, or similar products into your diet, this research suggests potential cardiovascular benefits. However, the authors emphasize that not all plant-based products are created equal—some contain high levels of sodium and processed ingredients that may offset some benefits.
Key Takeaway: Plant-based meat alternatives may support heart health by improving cholesterol profiles, but whole food plant sources remain the gold standard (Fernández-Rodríguez et al., 2025).
Study #2: Protein Source Doesn't Determine Mortality Risk
Challenging Common Assumptions
In a significant analysis that challenges popular narratives, Papanikolaou et al. (2025) examined data from NHANES III (National Health and Nutrition Examination Survey) to investigate whether animal protein versus plant protein intake affects mortality rates from all causes, cardiovascular disease, or cancer.
The Surprising Results
Published in Applied Physiology, Nutrition, and Metabolism, this population-level study found something unexpected: neither animal nor plant protein usual intakes were adversely associated with mortality risk from any cause examined.
This means that when researchers tracked thousands of Americans over time, they found that:
Total protein intake (regardless of source) wasn't linked to increased death rates
Animal protein consumption didn't increase cardiovascular mortality
Plant protein intake didn't show superior protection against cancer deaths
The quality of overall dietary pattern appeared more important than protein source alone
Understanding the Nuance
This doesn't mean protein source is irrelevant. Rather, it suggests that within the context of a balanced diet, moderate consumption of both animal and plant proteins can coexist without adverse mortality outcomes. The study controlled for numerous confounding variables including age, smoking status, physical activity, and overall caloric intake.
Key Takeaway: Moderate protein consumption from diverse sources—both animal and plant—can be part of a healthy dietary pattern without increasing mortality risk (Papanikolaou et al., 2025).
Study #3: Frequent Non-Vegetarian Food Consumption and Health Impacts
Examining Heavy Meat Consumption
Kadire and Desai (2024) took a different approach, investigating what happens when non-vegetarian food consumption becomes particularly frequent. Their research, published in the International Journal for Multidisciplinary Research, focused on adult health outcomes associated with regular meat eating.
Important Findings
The study identified several concerns with excessive meat consumption, particularly when non-vegetarian foods dominate the diet:
Increased saturated fat intake leading to elevated cholesterol
Higher consumption of processed meats linked to inflammatory responses
Potential accumulation of heme iron, which may promote oxidative stress
Association with higher rates of metabolic syndrome components
However, the researchers distinguished between moderate meat consumption and excessive intake. The negative health associations were primarily observed in individuals consuming non-vegetarian foods multiple times daily, particularly when choosing processed meats like bacon, sausages, and deli meats over unprocessed options.
This research underscores an important principle in nutrition: frequency and quantity matter. Occasional meat consumption as part of a varied diet differs significantly from heavy, daily reliance on animal products, especially processed varieties.
Key Takeaway: Frequent consumption of non-vegetarian foods, particularly processed meats, may negatively impact adult health markers, but occasional moderate intake may not pose the same risks (Kadire & Desai, 2024).
Study #4: Nutritional Adequacy of Plant-Based Diets in Australia
Austin et al. (2025) conducted a crucial investigation published in the European Journal of Clinical Nutrition, comparing the nutritional adequacy of Australians following plant-based diets versus those consuming regular meat-eating diets. This study addressed a critical question: Do vegetarians and vegans meet their nutritional needs?
The Nutritional Reality Check
The researchers assessed dietary intakes of essential nutrients and found mixed results:
Nutrients Higher in Plant-Based Diets:
Dietary fiber (significantly higher)
Folate and other B-vitamins (except B12)
Vitamin C and antioxidants
Magnesium and potassium
Nutrients of Concern in Plant-Based Diets:
Vitamin B12 (critically low in many vegans)
Iron (adequate total intake but lower bioavailability)
Zinc (borderline adequacy)
Omega-3 fatty acids (EPA and DHA specifically)
Calcium (particularly in those avoiding dairy)
Protein (adequate quantity but questions about quality)
The Supplementation Question
The study found that many individuals following strict plant-based diets required dietary supplements to achieve nutritional adequacy, particularly for vitamin B12, which is found naturally almost exclusively in animal products. Without supplementation, vegans showed concerning deficiency rates.
Key Takeaway: Plant-based diets can be nutritionally adequate but require careful planning and often supplementation, particularly for vitamin B12, iron, and omega-3 fatty acids (Austin et al., 2025).
Study #5: Vegetarian vs. Non-Vegetarian Diets and Cardiovascular Biomarkers
Chakole et al. (2025) provided direct comparative data in their study published in the Journal of Pharmacy and Bioallied Sciences. They measured specific cardiovascular biomarkers in adults following vegetarian versus non-vegetarian diets, focusing on hs-CRP levels (high-sensitivity C-reactive protein, an inflammation marker) and lipid profiles.
The Inflammation and Cholesterol Connection
The research revealed interesting patterns:
Vegetarian Diet Advantages:
Lower hs-CRP levels, indicating reduced systemic inflammation
More favorable HDL to LDL cholesterol ratios
Lower triglyceride levels in many participants
Reduced markers of oxidative stress
Non-Vegetarian Diet Observations:
Higher total cholesterol on average
Elevated inflammatory markers in frequent meat consumers
Variable outcomes depending on meat type and preparation methods
Better vitamin B12 status and iron stores
Importantly, the researchers noted that diet quality within each category varied tremendously. A vegetarian consuming primarily refined carbohydrates and fried foods showed worse biomarkers than a meat-eater emphasizing lean proteins, vegetables, and whole grains.
Key Takeaway: Vegetarian diets may offer advantages for inflammation and lipid profiles, but diet quality and whole food choices matter more than simply avoiding meat (Chakole et al., 2025).
Study #6: Global Burden of Diet-Related Chronic Diseases
Ma et al. (2025) took the widest lens possible, examining trends in chronic disease burden attributable to diet-related risk factors from 1990 to 2021, with projections through 2030. Published in Frontiers in Nutrition, this population-based study provides crucial context for understanding how dietary patterns affect global health.
The researchers identified several concerning patterns:
Rising Disease Burden:
Cardiovascular diseases remain the leading diet-related cause of death and disability
Type 2 diabetes rates continue climbing, strongly linked to dietary patterns
Certain cancers show associations with specific dietary risk factors
Obesity-related conditions accelerate in middle- and low-income countries
Key Dietary Risk Factors Identified:
High sodium intake (from processed foods and added salt)
Low whole grain consumption
Insufficient fruit and vegetable intake
Excessive red and processed meat consumption
High sugar-sweetened beverage intake
Low legume and nut consumption
If current dietary trends continue without intervention, the researchers project that diet-related chronic disease burden will increase substantially by 2030, particularly in regions undergoing nutrition transitions where traditional diets give way to Western-style eating patterns high in processed foods and animal products.
Key Takeaway: Global disease burden from diet-related risk factors continues rising, driven primarily by excessive processed food consumption, inadequate plant food intake, and imbalanced macronutrient ratios rather than any single food source (Ma et al., 2025).
Synthesizing the Science: What Does It All Mean?
After examining these six comprehensive studies, several themes emerge:
Context and Quality Trump Categories
Whether you choose plant-based eating, omnivorous diets, or something in between matters less than the overall quality of your dietary pattern. A vegetarian eating primarily processed foods may fare worse than a thoughtful omnivore emphasizing whole foods.
Plant-Based Meat Alternatives Show Promise
Meat substitutes can offer cardiovascular benefits, particularly for those unable or unwilling to increase whole plant food consumption. However, they shouldn't replace whole food plant sources as your primary protein.
Moderation Is Key for Meat Consumption
The evidence suggests that moderate meat intake as part of a balanced diet doesn't necessarily increase mortality risk, but frequent, excessive consumption—particularly of processed meats—does pose health concerns.
Plant-Based Diets Require Planning
While vegetarian and vegan diets can be healthfully adequate, they require careful attention to potentially deficient nutrients, particularly vitamin B12, iron, zinc, and omega-3 fatty acids.
Inflammation and Cholesterol Matter
Cardiovascular biomarkers like hs-CRP and LDL cholesterol consistently show favorable changes with increased plant food consumption and decreased processed meat intake.
Global Dietary Patterns Need Improvement
Regardless of whether populations eat meat or not, the global disease burden from poor dietary choices continues rising, driven largely by processed food consumption and inadequate whole plant food intake.
Practical Recommendations: Building Your Optimal Diet
For Everyone:
Prioritize Whole Foods: Whether plant or animal-based, choose minimally processed options. Fresh vegetables, whole grains, legumes, nuts, seeds, and fresh meats should form your dietary foundation.
Increase Plant Food Diversity: Aim for at least 5-7 servings of varied fruits and vegetables daily, regardless of whether you eat meat.
Limit Processed Meats: Reduce bacon, sausages, deli meats, and other heavily processed animal products.
Watch Sodium Intake: Both traditional processed foods and some plant-based meat alternatives can be surprisingly high in salt.
Balance Omega-3 Fatty Acids: Include fatty fish, walnuts, flaxseeds, or algae-based supplements for essential EPA and DHA.
For Plant-Based Eaters:
Supplement Vitamin B12: This is non-negotiable for vegans and advisable for vegetarians. Aim for 2.4 mcg daily through fortified foods or supplements.
Optimize Iron Absorption: Consume iron-rich plant foods (legumes, dark leafy greens, fortified grains) with vitamin C sources to enhance absorption.
Include Complete Protein Sources: Combine legumes with whole grains, or choose quinoa, soy products, hemp seeds, or other complete protein sources.
Consider Zinc and Iodine: Use iodized salt moderately and include zinc-rich seeds and nuts or consider supplementation.
Get Regular Blood Work: Monitor vitamin B12, iron status, and vitamin D levels annually.
For Meat Eaters:
Choose Lean, Unprocessed Options: Prioritize poultry, fish, and unprocessed red meat over processed varieties.
Practice Portion Control: Consider meat as a complement rather than the centerpiece of every meal. Aim for 3-4 ounce servings.
Increase Vegetable Ratios: Fill half your plate with non-starchy vegetables at each meal.
Vary Your Protein Sources: Include legumes, nuts, and plant-based meals several times weekly.
Choose Healthy Cooking Methods: Opt for grilling, baking, steaming, or sautéing over frying or charring.
Understanding Biomarkers: What Should You Monitor?
Based on the research reviewed, consider tracking these cardiovascular health markers:
Essential Biomarkers:
Lipid Profile:
Total cholesterol (target: <200 mg/dL)
LDL cholesterol (target: <100 mg/dL)
HDL cholesterol (target: >40 mg/dL men, >50 mg/dL women)
Triglycerides (target: <150 mg/dL)
Inflammatory Markers:
hs-CRP (high-sensitivity C-reactive protein; target: <1.0 mg/L)
Metabolic Indicators:
Fasting glucose (target: 70-99 mg/dL)
HbA1c (target: <5.7%)
Blood pressure (target: <120/80 mmHg)
Nutritional Status (especially for plant-based eaters):
Vitamin B12 (target: >200 pg/mL)
Ferritin (iron stores)
Vitamin D
Omega-3 Index (if available)
Common Myths Debunked by Current Research
Myth 1: "You Must Avoid All Meat for Heart Health"
Reality: The research shows that moderate, unprocessed meat consumption within a balanced dietary pattern isn't associated with increased mortality risk. The problems arise with excessive intake and heavily processed meats (Papanikolaou et al., 2025).
Myth 2: "Plant-Based Automatically Means Healthy"
Reality: Dietary quality matters more than categories. A diet high in refined plant foods (white bread, sugary snacks, french fries) won't deliver cardiovascular benefits simply because it's plant-based (Austin et al., 2025; Chakole et al., 2025).
Myth 3: "Protein Source Doesn't Matter"
Reality: While protein amount from different sources may not affect mortality, the bioavailability of other nutrients, fat content, and processing methods associated with different protein sources significantly impact overall health outcomes (Fernández-Rodríguez et al., 2025).
Myth 4: "Plant-Based Diets Are Automatically Nutritionally Complete"
Reality: Careful planning and often supplementation are necessary to ensure nutritional adequacy on strict plant-based diets, particularly for vitamin B12, iron, and omega-3 fatty acids (Austin et al., 2025).
Frequently Asked Questions (FAQs)
Q1: Should I completely eliminate meat from my diet for better heart health?
A: Not necessarily. The research suggests that moderate consumption of unprocessed meats within a balanced diet rich in plant foods doesn't appear to increase mortality risk. However, reducing processed meat and increasing plant food diversity consistently shows cardiovascular benefits (Fernández-Rodríguez et al., 2025; Papanikolaou et al., 2025).
Q2: Are plant-based meat alternatives healthier than regular meat?
A: It depends on the specific products and your overall dietary pattern. Plant-based meat alternatives show promise for improving cholesterol levels and may reduce cardiovascular risk factors. However, some contain high sodium and processed ingredients. Whole plant foods like legumes, nuts, and seeds generally offer superior nutritional profiles (Fernández-Rodríguez et al., 2025).
Q3: What supplements do I need on a plant-based diet?
A: At minimum, vegans should supplement vitamin B12 (2.4 mcg daily). Many also benefit from vitamin D, omega-3 fatty acids (algae-based EPA/DHA), and potentially iron and zinc depending on individual needs and blood test results (Austin et al., 2025).
Q4: How much meat is considered "moderate" consumption?
A: While studies don't define exact amounts uniformly, general guidelines suggest limiting red meat to 1-2 servings per week (3-4 ounces per serving) and choosing poultry or fish more frequently if consuming animal products regularly. Daily meat consumption, especially of processed varieties, appears problematic (Kadire & Desai, 2024).
Q5: Can I get enough protein on a plant-based diet?
A: Yes, protein adequacy is achievable through varied plant sources including legumes, whole grains, nuts, seeds, and soy products. However, attention to amino acid complementarity and total intake is important, especially for athletes or older adults with higher protein needs (Austin et al., 2025).
Q6: Which diet is best for reducing inflammation?
A: Diets emphasizing whole plant foods while limiting processed meats and refined carbohydrates consistently show lower inflammatory markers like hs-CRP. This can be achieved through vegetarian patterns or thoughtful omnivorous diets emphasizing fish, lean poultry, and abundant plants (Chakole et al., 2025).
Q7: What about cholesterol on plant-based versus meat-containing diets?
A: Plant-based patterns generally show more favorable lipid profiles with lower LDL cholesterol and better HDL to LDL ratios. However, meat-eaters emphasizing lean proteins, fish, and abundant plant foods can also achieve healthy cholesterol levels (Fernández-Rodríguez et al., 2025; Chakole et al., 2025).
Q8: Are these dietary recommendations universal across populations?
A: While principles of whole food emphasis and processed food limitation apply broadly, individual needs vary based on genetics, activity level, age, health status, and cultural context. The studies reviewed included diverse populations but may not capture all variations (Ma et al., 2025).
The Bottom Line: Key Takeaways
After examining the latest research on plant-based diets, meat consumption, and cardiovascular health, several clear conclusions emerge:
Quality Over Category: The quality of your overall dietary pattern matters more than simply whether you eat meat. Whole foods, minimal processing, and nutritional diversity are paramount.
Plant Foods Are Essential: Regardless of whether you consume animal products, increasing vegetables, fruits, whole grains, legumes, nuts, and seeds benefits cardiovascular health.
Processed Meats Pose Risks: Frequent consumption of processed meats shows consistent associations with negative health outcomes. Limiting these should be a priority.
Plant-Based Requires Planning: Vegetarian and vegan diets can be healthful but require attention to vitamin B12, iron, zinc, omega-3s, and overall protein quality.
Moderation Works: Moderate consumption of unprocessed meat within a predominantly plant-based dietary pattern appears compatible with good health for most people.
Individual Variation Exists: Optimal diets may differ based on genetics, health status, preferences, and values. Both thoughtful plant-based and omnivorous patterns can support health.
Global Trends Are Concerning: The rising burden of diet-related chronic diseases demands urgent attention to food quality, processing levels, and plant food adequacy worldwide.
Call to Action: Take Control of Your Cardiovascular Health
Now that you understand what current science reveals about plant-based eating, meat consumption, and heart health, it's time to take action:
Step 1: Assess Your Current Diet
Track your food intake for 3-7 days using a journal or app. Note your consumption of:
Vegetables and fruits (aim for 5+ servings daily)
Whole grains versus refined grains
Processed meats and frequency
Plant-based protein sources
Omega-3 rich foods
Step 2: Set Realistic Goals
Based on the research reviewed, choose 2-3 actionable changes:
Add one extra serving of vegetables to each meal
Replace processed meat with plant-based protein twice weekly
Include fatty fish or plant-based omega-3 sources three times weekly
Choose whole grains instead of refined options
Experiment with plant-based meat alternatives once weekly
Step 3: Get Baseline Biomarkers
Schedule a check-up to measure:
Complete lipid panel (cholesterol and triglycerides)
Fasting glucose and HbA1c
hs-CRP (inflammatory marker)
Vitamin B12 and vitamin D (especially if plant-based)
Blood pressure
Step 4: Implement Gradually
Don't overhaul everything overnight. Make sustainable changes:
Week 1-2: Increase vegetable portions and variety
Week 3-4: Reduce processed meat consumption
Week 5-6: Add plant-based meals several times weekly
Week 7-8: Optimize cooking methods and food quality
Ongoing: Monitor how you feel and adjust accordingly
Step 5: Retest and Refine
After 3-6 months of dietary changes, retest your cardiovascular biomarkers to objectively assess impact. Adjust your approach based on results and how you feel.
Step 6: Stay Informed
Nutrition science evolves constantly. Follow reputable sources:
Subscribe to evidence-based nutrition newsletters
Consult with registered dietitians for personalized guidance
Stay skeptical of extreme claims from any dietary camp
Prioritize peer-reviewed research over anecdotes
Final Thoughts: Your Personalized Path Forward
The 2025 research we've examined reveals a nuanced picture: neither complete meat avoidance nor unrestricted meat consumption represents the optimal path for most people. Instead, the evidence points toward a flexible, quality-focused approach that emphasizes:
Abundance: Vegetables, fruits, whole grains, legumes, nuts, and seeds should dominate your plate.
Moderation: If you choose to eat meat, emphasize unprocessed options in reasonable portions.
Variety: Diverse protein sources—both plant and animal—provide different nutrients and benefits.
Quality: Choose whole foods over processed alternatives whenever possible.
Individuality: Adapt general principles to your unique needs, preferences, and values.
Whether you're drawn to plant-based eating for health, environmental, or ethical reasons, or prefer an omnivorous approach that includes quality animal products, the research suggests both paths can lead to excellent health outcomes when executed thoughtfully.
The key lies not in dogmatic adherence to any single dietary philosophy but in understanding the principles that support cardiovascular health and applying them consistently within a framework that works for your life.
Your heart—and your overall health—will thank you for taking this evidence-based, balanced approach to nutrition.
Here is a polished Author’s Note / Reflective Closing you can place at the end of the article. It is measured, scholarly, and non-defensive, consistent with your tone as a clinician–academic:
A Word on Nutrition Science and Nuance
Nutrition science rarely offers simple answers to complex biological questions. Unlike pharmacology, diet operates through patterns, context, culture, and long-term behaviors that cannot be fully captured by short-term trials or single biomarkers. As a result, scientific debates around meat, plant-based diets, and cardiovascular health often become polarized—sometimes more by ideology than evidence.
The intent of this article was not to advocate for or against any single dietary philosophy, but to present the best available evidence with clinical realism, acknowledging both benefits and limitations. Current data consistently suggest that diet quality, food processing, and overall pattern matter far more than rigid labels such as “vegetarian” or “omnivorous.”
Equally important, what is optimal at a population level may not be identical for every individual. Age, metabolic health, genetics, nutritional status, cultural context, and personal preferences all influence dietary needs. Sound nutrition guidance must therefore be flexible, evidence-based, and patient-centered, rather than absolute.
As nutrition research continues to evolve, readers are encouraged to remain skeptical of extreme claims, prioritize whole and minimally processed foods, and apply scientific findings thoughtfully—ideally in consultation with qualified healthcare professionals.
Progress in nutrition science does not come from choosing sides, but from asking better questions and respecting biological complexity.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Individual circumstances vary, and treatment decisions should always be made in consultation with qualified healthcare professionals.
Related Articles
What’s New in the 2025 Blood Pressure Guidelines? A Complete Scientific Breakdown | DR T S DIDWAL
Low-Fat vs. Low-Carb: Which Diet is Best for Weight Loss? | DR T S DIDWAL
5 Steps to Reverse Metabolic Syndrome: Diet, Habit, & Lifestyle Plan | DR T S DIDWAL
The Role of Cholesterol in Health and Disease: Beyond the "Bad" Label | DR T S DIDWAL
Lowering Cholesterol with Food: 4 Phases of Dietary Dyslipidemia Treatment | DR T S DIDWAL
High Triglyceride Levels: 5 New Facts to Help You Lower Your Risk | DR T S DIDWAL
The Best Dietary Fat Balance for Insulin Sensitivity, Inflammation, and Longevity | DR T S DIDWAL
Feed Your Gut, Fuel Your Health: Diet, Microbiota, and Systemic Health | DR T S DIDWAL
References
Austin, G., Ferguson, J. J. A., Eslick, S., Oldmeadow, C., Wood, L. G., & Garg, M. L. (2025). Dietary intakes and nutritional adequacy of Australians consuming plant-based diets compared to a regular meat-eating diet. European Journal of Clinical Nutrition, 79(9), 876–887. https://doi.org/10.1038/s41430-025-01621-1
Chakole, S., Anjankar, N., Anjankar, A., Narkhede, H., & Mahajan, S. (2025). Influence of vegetarian and nonvegetarian diets on hs-CRP levels, lipid profiles, and cardiovascular health in adults. Journal of Pharmacy and Bioallied Sciences, 17(Suppl. 1), S284–S286. https://doi.org/10.4103/jpbs.jpbs_470_25
Fernández-Rodríguez, R., Bizzozero-Peroni, B., Díaz-Goñi, V., Garrido-Miguel, M., Bertotti, G., Roldán-Ruiz, A., & López-Moreno, M. (2025). Plant-based meat alternatives and cardiometabolic health: A systematic review and meta-analysis. The American Journal of Clinical Nutrition, 121(2), 274–283. https://doi.org/10.1016/j.ajcnut.2024.12.002
Kadire, B., & Desai, P. (2024). Frequent consumption of non-vegetarian food and its impact on adult health. International Journal for Multidisciplinary Research (IJFMR), 6(6), Article 32295. https://doi.org/10.36948/ijfmr.2024.v06i06.32295
Ma, H., Wang, M., Qin, C., Shi, Y., Mandizadza, O. O., Ni, H., & Ji, C. (2025). Trends in the burden of chronic diseases attributable to diet-related risk factors from 1990 to 2021 and the global projections through 2030: A population-based study. Frontiers in Nutrition, 12, 1570321. https://doi.org/10.3389/fnut.2025.1570321
Papanikolaou, Y., Phillips, S. M., & Fulgoni, V. L. (2025). Animal and plant protein usual intakes are not adversely associated with all-cause, cardiovascular disease–, or cancer-related mortality risk: An NHANES III analysis. Applied Physiology, Nutrition, and Metabolism, 50(1). https://doi.org/10.1139/apnm-2023-0594