Carb Counting vs. Low-Carb Diets: Which Controls Blood Sugar Better
Does managing diabetes mean giving up carbs? Science says no. Learn the evidence-based benefits of carbohydrate counting for glucose stability and quality of life.
DIABETESNUTRITION
Dr. T.S. Didwal, M.D.(Internal Medicine)
1/15/202612 min read
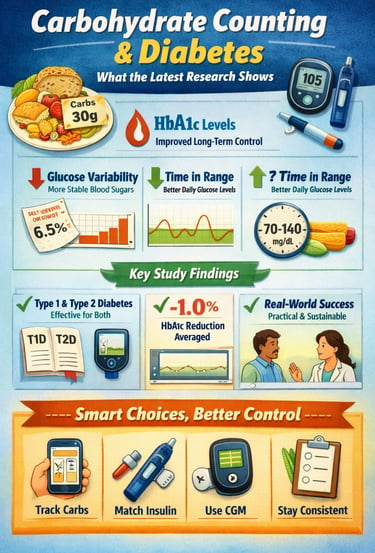
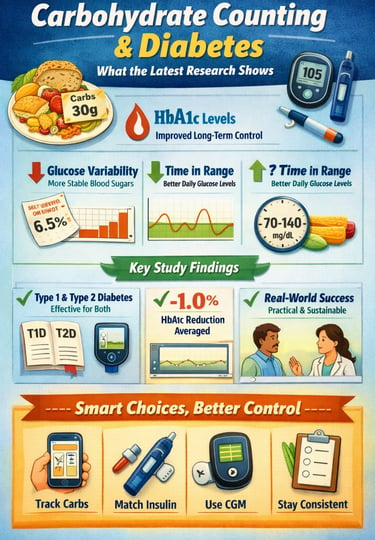
What if managing diabetes could become simpler, more predictable, and more personalized—just by understanding how much carbohydrate is on your plate? In recent years, carbohydrate counting has emerged as one of the most powerful tools for optimizing blood glucose control in both type 1 and type 2 diabetes. Unlike restrictive diets that eliminate entire food groups, carbohydrate counting focuses on awareness and precision. It helps you understand how different foods impact your post-meal glucose response, empowering you to make informed decisions at every meal (Sakane et al., 2025).
The latest studies reveal that individuals who consistently track their carbohydrate intake achieve significantly better HbA1c levels, reduced glucose variability, and improved time-in-range metrics (Cai et al., 2025; Ibrahim et al., 2023). This approach is especially beneficial for people using insulin therapy—allowing them to more accurately match insulin doses to carbohydrate content and avoid dangerous highs and lows. Evidence also shows that even without insulin adjustments, simply being mindful of carbohydrate quantity leads to more stable daily glucose patterns (Al-Mssallem et al., 2020).
In an era where diabetes technology is evolving rapidly, from continuous glucose monitors to smart insulin pumps, carbohydrate counting remains a foundational skill. It bridges advanced science with everyday eating habits, placing control back into the hands of the person living with diabetes.
Clinical pearls
1. Prioritize "Time in Range" Over Just HbA1c
While HbA1c provides a 3-month average, it can hide dangerous "highs" and "lows." Recent research emphasizes Time in Range (TIR)—the percentage of the day your glucose stays between 70–180 mg/dL. Aiming for a higher TIR reduces the risk of long-term complications more effectively than focusing on an average number alone.
2. The "Mindfulness Effect" Trumps Rigid Restriction
Clinical data suggests that the act of tracking carbohydrates is often more impactful than the total amount of carbs consumed. Being intentional and aware of what is on your plate creates a "feedback loop" that naturally improves glucose stability, even if you aren't on a strictly "low-carb" diet.
3. Pair Carbs with "Buffers" to Flatten the Spike
To manage postprandial glucose (the spike after eating), think about the "company" your carbs keep. Pairing carbohydrates with fiber, healthy fats, or protein slows down gastric emptying. This ensures glucose enters the bloodstream as a steady stream rather than a flood.
4. Precision Dosing Requires Accurate Quantification
For those using insulin or GLP-1 agonists, carb counting isn't just about nutrition; it’s about pharmacology. Accurate counting allows you to match your "insulin-to-carb ratio" precisely. Even a 15-gram error (the equivalent of one slice of bread) can lead to significant glucose variability over time.
5. Utilize the "Second Meal Effect"
Research shows that the composition of your breakfast can influence your blood sugar response for the rest of the day. Consuming a breakfast with low-glycemic-index carbs and high fiber can improve your insulin sensitivity during lunch and dinner, a phenomenon known as the "second meal effect."
Understanding Carbohydrate Counting: A Foundation for Diabetes Management
Carbohydrate counting is a meal planning tool that helps people with diabetes understand how different foods impact their blood glucose levels. Rather than eliminating carbohydrates entirely, this approach teaches you to monitor and track your intake of dietary carbohydrates, which are the primary macronutrient affecting postprandial glucose (blood sugar after meals).
The concept is straightforward: different carbohydrate-containing foods affect blood sugar differently, and by quantifying your intake, you can better predict and manage your glucose response. This is particularly important for people using insulin therapy or glucagon-like peptide-1 (GLP-1) agonists, as it allows for more precise medication dosing.
What the Latest Research Tells Us
Recent studies have provided compelling evidence about the effectiveness of carbohydrate counting across different diabetes populations. Let's explore the key findings from current research.
Comprehensive Evidence from 2025 Systematic Review
Sakane, Domichi, and Suganuma (2025) conducted a systematic review and meta-analysis examining the efficacy of carbohydrate counting in both type 1 and type 2 diabetes mellitus. This comprehensive analysis combined data from multiple studies to provide a broad overview of the intervention's effectiveness.
Key Takeaway: This systematic review demonstrates that carbohydrate counting interventions show measurable benefits in glycemic control for both diabetes types. The meta-analysis suggests that structured education in carbohydrate calculation leads to improvements in HbA1c levels (a marker of long-term blood sugar control) and helps reduce the variability in glucose monitoring outcomes.
Evidence-Based Nutrition Options for Type 2 Diabetes
The Journal of Clinical Endocrinology & Metabolism recently featured research by Baskin and Karp (2025) that examined evidence-based nutrition approaches for type 2 diabetes management. This work explored the spectrum of dietary interventions available to clinicians and patients.
Key Takeaway: Among the various nutrition strategies evaluated, carbohydrate counting stands as one of four primary evidence-based options for managing type 2 diabetes. The research highlights that when combined with other lifestyle modifications and appropriate pharmacotherapy, carbohydrate-controlled diets show significant promise for improving metabolic outcomes and reducing cardiovascular risk factors in people with type 2 diabetes.
Real-World Barriers: What Dietitians Are Telling Us
Dimitriades and Pillay (2022) conducted important research examining how dietitians actually implement carbohydrate counting in clinical practice. They explored training gaps and real-world barriers that prevent wider adoption of this valuable tool.
Key Takeaway: While carbohydrate counting is effective, successful implementation faces significant challenges. These include time constraints in clinical settings, inadequate training in carbohydrate quantification methods, patient complexity, and varying levels of patient motivation. The study emphasizes that proper dietitian training and patient education are essential for maximizing the benefits of this approach. Healthcare providers need robust support systems to effectively teach and monitor carbohydrate counting in their patients with type 1 diabetes.
Clinical Impact: Practical Results in Diabetes Management
Ibrahim, Shahat, Amer, and Aljohani (2023) published a comprehensive review in Cureus examining the practical impact of carbohydrate counting on managing diabetic patients. This research synthesized evidence about real-world outcomes.
Key Takeaway: The evidence demonstrates that carbohydrate counting significantly improves several important markers of diabetes control, including HbA1c reduction, better blood glucose stability, decreased hyperglycemic episodes (dangerously high blood sugar), and improved quality of life. The intervention appears particularly effective when combined with continuous glucose monitoring (CGM) technology and personalized education. Importantly, this approach works across different age groups and diabetes durations, making it a versatile option for many patients.
Dietary Intake and Type 2 Diabetes Control
Al-Mssallem, Al-Qarni, and Al-Jamaan (2020) conducted a cross-sectional study examining the relationship between dietary carbohydrate intake levels and diabetes control in type 2 diabetes patients.
Key Takeaway: This research reveals important patterns about how daily carbohydrate consumption impacts glycemic outcomes. Patients who actively monitored and moderately controlled their carbohydrate intake demonstrated superior blood glucose management compared to those without structured tracking. The study suggests that the specific amount of carbohydrates consumed matters less than having an intentional, tracked approach. This finding underscores the value of awareness—simply being mindful of carbohydrate content in meals can significantly improve metabolic control.
Carbohydrate Intake and Glucose Variability in Type 1 Diabetes
Cai, Li, Xiong, Zhang, He, and Su (2025) investigated associations between daily dietary carbohydrate intake and time in range (TIR) in adults with type 1 diabetes. Time in range is a crucial modern metric for assessing how often people maintain healthy glucose levels throughout the day.
Key Takeaway: This recent research demonstrates that tailored carbohydrate intake strategies directly improve TIR metrics in type 1 diabetes management. Adults who carefully matched their carbohydrate consumption to their insulin dosing achieved significantly better glycemic stability and spent more time within their target blood glucose range. The study suggests that personalized carbohydrate targets, determined through ongoing glucose monitoring and adjusted based on individual response patterns, yield the best outcomes. This finding is particularly relevant in the era of continuous glucose monitors and insulin pump therapy, where real-time data allows for precise carbohydrate-to-insulin ratios.
How to Get Started with Carbohydrate Counting
Understanding the research is one thing; applying it to your daily life is another. Here's a practical approach:
Step 1: Learn the Basics - Work with a registered dietitian or certified diabetes educator to understand what counts as a carbohydrate. This includes starches, fruits, milk products, and sugary foods, but also vegetables and legumes.
Step 2: Identify Portion Sizes - Use food labels, portion guides, or apps to determine the carbohydrate content of your meals. One exchange typically equals 15 grams of carbohydrates.
Step 3: Track and Adjust - Monitor how different carbohydrate quantities affect your blood sugar levels. Using a blood glucose meter or continuous glucose monitor helps identify your personal patterns.
Step 4: Use Your Data - Share your carbohydrate tracking records with your healthcare team. This information helps optimize your medication dosing and overall diabetes management strategy.
Step 5: Practice Consistency - Over time, carbohydrate estimation becomes easier. Most people develop the ability to quickly estimate carbohydrate content at a glance.
Carbohydrate Counting vs Glycemic Index
While Carbohydrate Counting focuses on the total amount of glucose entering the system, the Glycemic Index (GI) determines the speed at which that glucose arrives. Integrating both is the "gold standard" for minimizing glycemic variability.
The "Volume" vs. "Velocity" Framework
Carb Quantity (The Volume): This is the total number of grams you consume. It dictates the peak height of your blood sugar. If you eat 60g of carbs, your body must process 60g of sugar, regardless of the source. This is the primary metric for calculating insulin-to-carb ratios.
Carb Quality (The Velocity): This is where the Glycemic Index comes in. It measures how quickly a carbohydrate-containing food raises blood glucose.
High-GI foods (e.g., white bread, sugary cereals) cause a sharp, rapid "spike."
Low-GI foods (e.g., lentils, oats, non-starchy vegetables) result in a slower, sustained "roll."
Why the Distinction Matters Clinically
Even if two meals have the exact same Carb Quantity, their clinical impact can be vastly different. A meal with high quantity but low quality (low GI) is much easier for the body—and insulin—to manage because it prevents the "glucose roller coaster."
Recent research suggests that focusing on quality (fiber-rich, complex carbs) improves satiety and insulin sensitivity, making the "quantity" part of the equation easier to maintain over time.
Why a Carbohydrate Food Table Matters
A quick reference table of common foods and their approximate carbohydrate content can dramatically simplify the carbohydrate-counting process. While apps and food labels are useful, many daily meals—especially home-cooked or culturally specific dishes—do not come with precise nutritional information. Having a small, easy-to-remember list helps patients estimate portions more confidently and reduces guesswork during meals.
For beginners, this table serves as a practical starting point: a visual cue that improves accuracy and consistency. For more experienced individuals, it works as a mental checklist to prevent undercounting or overcounting carbohydrates. The goal isn’t perfection—it’s awareness. Even approximate tracking has been shown to improve blood glucose stability and enhance time-in-range outcomes.
Common Foods and Their Approximate Carbohydrate Content
Cooked rice — 1 cup = 45 g carbohydrates
Chapati/Roti (wheat) — 1 medium = 15–18 g carbohydrates
Apple — 1 medium = 25 g carbohydrates
Banana — 1 medium = 27 g carbohydrates
Potato (boiled) — 1 medium = 30 g carbohydrates
Milk — 1 cup = 12 g carbohydrates
Lentils (cooked) — 1 cup = 40 g carbohydrates
Bread — 1 slice = 15 g carbohydrates
Pasta (cooked) — 1 cup = 43 g carbohydrates
Key Takeaways: What You Should Know About Carbohydrate Counting
Carbohydrate counting is evidence-based: Multiple recent studies confirm its effectiveness for both type 1 and type 2 diabetes management.
It works across different populations: Whether you use insulin, oral medications, or lifestyle modifications alone, carbohydrate counting can enhance your glycemic control.
Training matters: Proper education from qualified healthcare providers significantly improves success rates. Don't hesitate to ask for dietitian referrals if needed.
Individual response varies: Your personal carbohydrate tolerance may differ from others. Working with your healthcare team to find your optimal carbohydrate targets is essential.
Technology enhances results: Continuous glucose monitoring and carbohydrate counting apps can make this strategy more manageable and effective.
Consistency beats perfection: You don't need to be perfect. Regular, intentional carbohydrate monitoring produces measurable improvements in diabetes outcomes.
Frequently Asked Questions
Q: Is carbohydrate counting the same as a "low-carb diet"?
A: No. Carbohydrate counting focuses on knowing and tracking your carbohydrate intake rather than eliminating carbs. You maintain a balanced diet while being intentional about portion sizes and carbohydrate distribution throughout your meals.
Q: Can I do carbohydrate counting without a continuous glucose monitor?
A: Absolutely. While CGM technology provides helpful feedback, traditional blood glucose meters work well with carbohydrate counting. The key is regular monitoring and recording your results alongside your carbohydrate intake.
Q: How long does it take to see results from carbohydrate counting?
A: Many people notice improvements in blood sugar stability within days to weeks. Measurable changes in HbA1c (which reflects 3-month average glucose) typically appear within 3 months of consistent practice.
Q: What if I don't have access to a dietitian?
A: Many resources exist, including diabetes educator webinars, hospital-based diabetes education programs, and reputable online platforms. Ask your doctor for referrals. Some insurance plans cover dietitian consultations for diabetes management.
Q: Do I need to count carbohydrates for non-starchy vegetables?
A: Most non-starchy vegetables contain minimal carbohydrates and don't significantly impact blood glucose. Traditionally, they're counted as "free" foods. However, starchy vegetables like potatoes and corn do require carbohydrate counting.
Q: Can children use carbohydrate counting?
A: Yes. In fact, carbohydrate counting is increasingly taught to children with type 1 diabetes, helping them develop healthy eating habits and understand their disease. Age-appropriate education is key.
Semantic Insights: The Complete Picture of Diabetes Nutrition
The research consistently shows that nutritional management of diabetes isn't one-size-fits-all. Carbohydrate counting, alongside considerations of glycemic index, fiber content, and nutrient density, forms a comprehensive approach to metabolic health. Terms like postprandial glucose response, insulin sensitivity, and glucose variability are central to understanding why carbohydrate awareness matters so profoundly.
Modern diabetes care recognizes that blood glucose management depends on multiple factors—medication, physical activity, stress, sleep, and food choices. Carbohydrate counting specifically addresses the nutritional component with scientific precision. When combined with glucose monitoring technology and lifestyle modification, it represents a practical bridge between laboratory science and real-world living with diabetes.
Your Next Steps: Taking Action
The evidence is clear: carbohydrate counting works for diabetes management. The research spanning 2020 to 2025 consistently demonstrates improvements in HbA1c levels, glucose stability, and quality of life.
Here's what to do:
Talk to your healthcare provider about incorporating carbohydrate counting into your diabetes management plan. Share these research findings if helpful.
Request a referral to a registered dietitian who specializes in diabetes. A personalized approach, grounded in your specific situation, yields the best results.
Start small with one meal per day, tracking your carbohydrate intake and noting how you feel and what your glucose readings show.
Use available tools—apps, food labels, portion guides—to make carbohydrate estimation manageable.
Be patient with yourself. Developing new skills takes time, but the investment pays dividends in better health outcomes and greater confidence in managing your diabetes.
Managing diabetes successfully means being an active participant in your care. Understanding how dietary carbohydrates affect your blood glucose levels empowers you to make choices that support your health. The research backs it up, and thousands of people living with diabetes benefit from this approach every day.
Your diabetes management journey is uniquely yours. Armed with evidence-based strategies like carbohydrate counting and support from your healthcare team, you're well-positioned to thrive.
Author’s Note
As a clinician and researcher deeply involved in diabetes care, my goal in writing this article is to bridge the gap between scientific evidence and practical daily living. Carbohydrate counting is not merely a dietary technique—it is a structured, data-driven approach that empowers people with diabetes to understand and influence their own metabolic health. The studies cited in this article, ranging from meta-analyses to clinical practice evaluations, reflect the growing consensus in the scientific community: carbohydrate awareness improves glycemic control, enhances time in range, and supports better long-term outcomes.
Yet evidence alone is not enough. Implementing carbohydrate counting requires education, support, and consistency. Many patients face barriers such as limited access to trained dietitians, varying food literacy, or the complexity of calculating carbohydrate portions in culturally diverse meals. This article aims to provide clarity, practical tools, and confidence for both patients and healthcare professionals seeking an evidence-based foundation for diabetes management.
My hope is that this information empowers you to take a more active role in your diabetes care, ask informed questions, and collaborate closely with your healthcare team. With the right knowledge, technology, and support, meaningful control of diabetes is not only possible—it is achievable and sustainable
.Disclaimer: This article is for informational purposes only and does not constitute medical advice. Individual circumstances vary, and treatment decisions should always be made in consultation with qualified healthcare professionals.
Related Articles
Feed Your Gut, Fuel Your Health: Diet, Microbiota, and Systemic Health | DR T S DIDWAL
What’s New in the 2025 Blood Pressure Guidelines? A Complete Scientific Breakdown | DR T S DIDWAL
Low-Fat vs. Low-Carb: Which Diet is Best for Weight Loss? | DR T S DIDWAL
5 Steps to Reverse Metabolic Syndrome: Diet, Habit, & Lifestyle Plan | DR T S DIDWAL
The Role of Cholesterol in Health and Disease: Beyond the "Bad" Label | DR T S DIDWAL
Lowering Cholesterol with Food: 4 Phases of Dietary Dyslipidemia Treatment | DR T S DIDWAL
High Triglyceride Levels: 5 New Facts to Help You Lower Your Risk | DR T S DIDWAL
The Best Dietary Fat Balance for Insulin Sensitivity, Inflammation, and Longevity | DR T S DIDWA
References
Baskin, R. G., & Karp, K. A. (2025). Navigating the spectrum of 4 evidence-based nutrition options for type 2 diabetes management. The Journal of Clinical Endocrinology & Metabolism, 110(Supplement_2), S112–S117. https://doi.org/10.1210/clinem/dgae646
Cai, Y., Li, X., Xiong, X., Zhang, L., He, J., & Su, H. (2025). Associations between daily dietary carbohydrate intake and TIR in adults with type 1 diabetes. Frontiers in Nutrition, 12, 1638849. https://doi.org/10.3389/fnut.2025.1638849
Dimitriades, M. E., & Pillay, K. (2022). Carbohydrate counting in type 1 diabetes mellitus: Dietitians' perceptions, training and barriers to use. South African Journal of Clinical Nutrition, 35(3), 94–99. https://doi.org/10.1080/16070658.2021.1979764
Ibrahim, H., Shahat, E. A., Amer, L. A., & Aljohani, A. K. (2023). The impact of using carbohydrate counting on managing diabetic patients: A review. Cureus, 15(11), e48998. https://doi.org/10.7759/cureus.48998
Al-Mssallem, M. Q., Al-Qarni, A. A., & Al-Jamaan, M. (2020). Dietary carbohydrate intake in patients with type 2 diabetes mellitus and diabetes control: A cross-sectional study. Food & Nutrition Research, 64, 4751. Sakane, N., Domichi, M., & Suganuma, A. (2025). Efficacy of carbohydrate counting in people with type 1 and type 2 diabetes mellitus: A systematic review and meta-analysis. Diabetology International, 16(3), 546–558.V https://doi.org/10.1007/s13340-025-00810-4
Sakane, N., Domichi, M., & Suganuma, A. (2025). Efficacy of carbohydrate counting in people with type 1 and type 2 diabetes mellitus: A systematic review and meta-analysis. Diabetology International, 16(3), 546–558. https://doi.org/10.1007/s13340-025-00810-4