Why Your Waistline Matters More Than Your Weight for Heart Health
Explore the latest research on WWI (Weight-Adjusted Waist Index). Learn how this metric predicts cardiometabolic multimorbidity, all-cause mortality, and kidney health in hypertensive patients more effectively than traditional anthropometrics.
HEART
Dr. T.S. Didwal, M.D.(Internal Medicine)
1/10/202612 min read
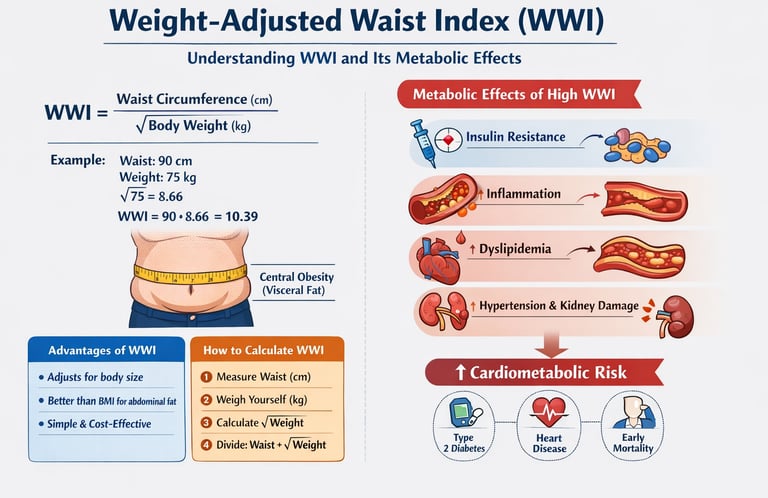
For decades, Body Mass Index (BMI) has been the most widely used tool to assess obesity and health risk. However, growing scientific evidence shows that BMI often fails to capture what truly matters for long-term health—central (abdominal) obesity and visceral fat accumulation. This is where the Weight-Adjusted Waist Index (WWI) emerges as a powerful and clinically relevant metric.
WWI combines waist circumference and body weight into a single, weight-normalized index that more accurately reflects visceral adiposity, the metabolically active fat strongly linked to insulin resistance, type 2 diabetes, hypertension, and cardiovascular disease (Liu et al., 2024). Unlike BMI, WWI is less influenced by muscle mass and better identifies individuals with normal weight but high cardiometabolic risk, a phenotype often missed in routine screening.
Recent large population studies demonstrate that higher WWI values are consistently associated with chronic inflammation, dyslipidemia, kidney damage, and increased all-cause and cardiovascular mortality, particularly in people with hypertension and older adults (Kunutsor et al., 2025; Yu et al., 2025). Because WWI relies on simple measurements—a tape and a scale—it offers a cost-effective, accessible tool for both clinical practice and population health screening.
In an era of precision medicine, WWI represents a meaningful step forward in assessing metabolic health beyond BMI.
Let's dive into the latest science and discover why healthcare professionals are increasingly turning to this innovative metric.
Clinical pearls
1. The "Hidden Risk" Pearl: Normal Weight Obesity
You can have a "healthy" BMI and still be at high metabolic risk. This is often called Metabolically Obese Normal Weight (MONW). WWI is the superior tool here because it "sees" through a normal weight to identify if your waist circumference is disproportionately high for your frame. If your WWI is creeping up while your scale stays the same, it’s a sign that muscle is being replaced by visceral fat.
2. The "Square Root" Logic: Why the Math Matters
The formula for WWI uses the square root of your weight ($\sqrt{kg}$) to neutralize the influence of body mass. In clinical terms, this means the metric focuses on fat distribution rather than just heaviness.
Patient Takeaway: Think of BMI as measuring your "quantity" of body, while WWI measures the "quality" of your body composition.
3. The Visceral Fat "Furnace"
Not all fat is just stored energy; visceral fat (the kind WWI measures) acts like an active endocrine organ. It pumps out inflammatory cytokines directly into your portal vein, heading straight to your liver. This is why a high WWI is a "smoking gun" for insulin resistance and fatty liver disease, even before your blood sugar levels start to rise on a lab test.
4. The Muscle-Preservation Advantage
As we age, we often lose muscle mass (sarcopenia) while gaining abdominal fat. Because BMI only looks at total weight, it might stay stable or even drop, giving a false sense of security. WWI captures this dangerous "crossover" by highlighting the increasing waistline even as total weight decreases. For older adults, a rising WWI is a more accurate predictor of multimorbidity than the scale alone.
5. The "Tape Measure" over the "Lab Test"
While we often wait for blood work to show high triglycerides or low HDL, WWI offers a real-time clinical marker you can track at home. Research shows that WWI correlates so strongly with "metabolic syndrome" that it can often predict cardiovascular events years before they manifest in standard blood panels. It is essentially a "low-tech" tool providing "high-tech" predictive power.
WWI (Weight-Adjusted Waist Index): The Body Composition Metric You Need to Know
What Exactly Is the Weight-Adjusted Waist Index?
The Weight-Adjusted Waist Index is calculated by dividing your waist circumference (in centimeters) by the square root of your body weight (in kilograms). This simple formula creates a ratio that better reflects abdominal adiposity—the dangerous fat stored around your vital organs.
Formula: WWI = Waist Circumference (cm) / √Body Weight (kg)
What makes WWI special? It's weight-independent, meaning it adjusts for your overall body size. This makes it superior to waist circumference alone and potentially more accurate than BMI for assessing cardiometabolic risk.
The Game-Changing Research: Five Studies That Changed Everything
Study 1: WWI as a Practical Predictor for Multiple Health Outcomes
Liu et al. (2024) conducted a comprehensive investigation that examined WWI's ability to predict diabetes, cardiovascular disease (CVD), and non-accidental mortality risk. This groundbreaking study, published in Nutrition, Metabolism, and Cardiovascular Diseases, analyzed substantial population data to establish WWI's clinical utility.
Key Findings:
WWI demonstrated strong predictive value for type 2 diabetes mellitus development
Higher WWI values correlated with increased cardiovascular disease risk
The metric successfully predicted all-cause mortality independent of other risk factors
WWI outperformed traditional anthropometric measurements in risk stratification
Clinical Significance: The researchers emphasized that WWI's practical nature makes it ideal for primary care settings and population health screening. Unlike complex imaging techniques or expensive biomarkers, WWI requires only a measuring tape and a scale—tools available in virtually any healthcare setting.
Key Takeaway: WWI isn't just another measurement—it's a cost-effective, accessible tool that can help identify at-risk individuals before serious complications develop (Liu et al., 2024).
Study 2: WWI and Cardiometabolic Multimorbidity in Older Adults
Kunutsor et al. (2025) took the research further by examining WWI's relationship with cardiometabolic multimorbidity—the presence of multiple metabolic conditions simultaneously—in older adults. Their study, published in GeroScience, utilized data from the prestigious English Longitudinal Study of Ageing (ELSA).
Key Findings:
Elevated WWI showed strong associations with cardiometabolic multimorbidity in aging populations
The relationship remained significant even after adjusting for confounding variables like age, sex, and lifestyle factors
WWI proved particularly valuable in identifying high-risk older adults who might benefit from targeted interventions
The metric helped predict the clustering of metabolic conditions including diabetes, hypertension, and dyslipidemia
Why This Matters for Aging Populations: As we age, our body composition changes dramatically, often with increased visceral fat accumulation. Traditional metrics may not capture these changes accurately. WWI's ability to identify cardiometabolic risk in older adults makes it an invaluable tool for geriatric assessment and preventive care.
Key Takeaway: For older adults, WWI offers a sensitive marker of metabolic health that can guide early intervention strategies and help prevent the cascade of multiple chronic conditions (Kunutsor et al., 2025).
Study 3: WWI in Hypertensive Patients with Kidney Complications
Yang et al. (2025) explored WWI's application in a specific, high-risk population: hypertensive patients with albuminuria (protein in the urine, indicating kidney damage). Published in Renal Failure, this study analyzed data from the National Health and Nutrition Examination Survey (NHANES) 2005-2020, encompassing 15 years of comprehensive health data.
Key Findings:
WWI showed significant associations with albuminuria severity in hypertensive patients
The study also examined the Cardiometabolic Index (CMI), comparing its predictive value with WWI
Higher WWI values correlated with increased kidney damage markers
Both WWI and CMI demonstrated utility in identifying patients at risk for cardiovascular-renal complications
The metrics helped stratify risk for progression to chronic kidney disease (CKD)
The Hypertension-Kidney-Heart Connection: This research highlights a critical reality: hypertension, obesity, and kidney disease are deeply interconnected. WWI serves as a bridge measurement that captures the metabolic dysfunction driving all three conditions.
Key Takeaway: For individuals with high blood pressure, WWI provides crucial insight into kidney health and cardiovascular risk, enabling more personalized treatment approaches (Yang et al., 2025).
Study 4 & 5: WWI Predicts Mortality in Hypertensive Populations
Two remarkably similar studies—Zheng et al. (2025) and Yu et al. (2025)—both published in Frontiers in Cardiovascular Medicine, examined WWI's ability to predict all-cause mortality and cardiovascular mortality specifically in individuals with hypertension.
Key Findings from Both Studies:
WWI demonstrated robust predictive power for death from all causes in hypertensive patients
Cardiovascular mortality risk increased proportionally with higher WWI values
The relationship followed a dose-response pattern—higher WWI meant progressively higher risk
WWI remained predictive even after controlling for other cardiovascular risk factors
The metric successfully identified high-risk hypertensive patients who needed aggressive management
Understanding the Mortality Connection: Why does WWI predict death so effectively? The answer lies in what it measures: central adiposity. Fat around your midsection isn't just cosmetic—it's metabolically active tissue that releases inflammatory molecules, disrupts insulin signaling, and promotes atherosclerosis (arterial plaque buildup).
Key Takeaway: For anyone with hypertension, WWI offers a powerful prognostic tool that can guide treatment intensity and lifestyle modification urgency (Zheng et al., 2025; Yu et al., 2025).
Why WWI Outperforms Traditional Measurements
The Limitations of BMI
Body Mass Index has served as the standard obesity metric for decades, but it has serious flaws:
Can't distinguish between muscle mass and fat mass
Doesn't account for fat distribution
May misclassify muscular individuals as overweight
Doesn't reflect visceral adiposity specifically
The Problem with Waist Circumference Alone
While waist circumference better reflects abdominal obesity, it doesn't account for overall body size. A 100cm waist means something very different on a 150-pound person versus a 250-pound person.
WWI's Advantages
Weight-Adjusted Waist Index combines the best of both worlds:
Normalized for body weight, providing fair comparison across different body sizes
Reflects central obesity more accurately than BMI
Simple to calculate and measure
Strong evidence for predicting metabolic syndrome, cardiovascular events, and mortality
Applicable across diverse populations and age groups
The Science Behind WWI: Why It Works
Understanding Visceral Fat
Not all fat is created equal. Subcutaneous fat (under the skin) is relatively benign, but visceral fat (around organs) is metabolically dangerous. This internal fat:
Releases inflammatory cytokines
Disrupts glucose metabolism
Contributes to insulin resistance
Promotes dyslipidemia (unhealthy cholesterol levels)
Increases blood pressure
WWI correlates strongly with visceral fat, making it an excellent surrogate marker for this dangerous fat depot.
The Cardiometabolic Disease Cascade
Insulin Resistance → Type 2 Diabetes
Dyslipidemia → Atherosclerosis
Inflammation → Endothelial Dysfunction
Metabolic Syndrome → Cardiovascular Disease
Kidney Damage → Cardiovascular-Renal Syndrome
WWI captures your position along this dangerous cascade.
Practical Applications: How to Use WWI
Calculating Your WWI
Step 1: Measure your waist circumference at the narrowest point (usually just above the belly button), exhaling normally. Record in centimeters.
Step 2: Weigh yourself and record your weight in kilograms.
Step 3: Calculate the square root of your weight.
Step 4: Divide your waist circumference by this number.
Example:
Waist: 90 cm
Weight: 75 kg
√75 = 8.66
WWI = 90 ÷ 8.66 = 10.39
Interpreting Your Results
Lower WWI values indicate healthier body composition
Higher WWI values suggest increased cardiometabolic risk
Your healthcare provider can help interpret your results in context with other risk factors
Tracking WWI changes over time provides valuable feedback on lifestyle interventions
Who Should Monitor WWI?
Individuals with obesity or overweight
People with hypertension
Those diagnosed with prediabetes or diabetes
Older adults at risk for multimorbidity
Anyone with family history of cardiovascular disease
Patients with chronic kidney disease
Clinical Implications for Healthcare Providers
The convergence of evidence from these five studies suggests several important clinical applications:
Risk Stratification
WWI enables more accurate risk stratification than traditional metrics. Patients with elevated WWI but normal BMI may require closer monitoring and earlier intervention.
Treatment Monitoring
Weight loss interventions should aim to reduce WWI, not just overall weight. This ensures fat loss comes from the dangerous abdominal region.
Patient Motivation
WWI provides tangible feedback that can motivate lifestyle changes. Unlike BMI, which moves slowly, WWI can show meaningful improvement relatively quickly with targeted abdominal fat reduction.
Population Health Screening
The cost-effectiveness and simplicity of WWI make it ideal for large-scale screening programs aimed at identifying at-risk populations before disease develops.
Lifestyle Strategies to Improve Your WWI
Targeted Nutrition Approaches
While you can't spot-reduce fat, certain dietary patterns preferentially reduce visceral adiposity:
Mediterranean diet rich in healthy fats, vegetables, and whole grains
Reduced refined carbohydrates and added sugars
Adequate protein intake to preserve lean muscle mass
Fiber-rich foods that improve glucose control and reduce inflammation
Limited alcohol consumption, which promotes abdominal fat storage
Exercise Recommendations
Research shows specific activities effectively target central obesity:
High-intensity interval training (HIIT) for metabolic benefits
Resistance training to build muscle and improve insulin sensitivity
Aerobic exercise for cardiovascular health and fat oxidation
Core strengthening for functional fitness
Aim for at least 150 minutes of moderate activity weekly
Stress Management
Chronic stress elevates cortisol, which promotes visceral fat accumulation. Incorporate:
Mindfulness meditation or similar relaxation techniques
Adequate sleep (7-9 hours nightly)
Stress-reduction practices like yoga or tai chi
Social connections and support networks
Medical Management
For high-risk individuals, medical interventions may include:
Blood pressure medications
Diabetes medications that promote weight loss
Lipid-lowering therapies
In select cases, bariatric surgery consideration
Key Takeaways: What You Need to Remember
✓ WWI is a superior metric for assessing cardiometabolic risk compared to traditional measurements like BMI
✓ Multiple 2024-2025 studies consistently demonstrate WWI's predictive power for diabetes, cardiovascular disease, and mortality
✓ WWI is particularly valuable for older adults and those with hypertension, capturing risk that other metrics miss
✓ The measurement is simple and practical, requiring only a measuring tape and scale—no expensive tests needed
✓ Higher WWI values correlate with dangerous visceral fat and increased risk of cardiometabolic multimorbidity
✓ Lifestyle interventions targeting abdominal obesity can improve WWI and reduce disease risk
✓ Healthcare providers should consider incorporating WWI into routine assessments, especially for at-risk populations
Frequently Asked Questions
Q: Is WWI better than BMI for everyone?
A: WWI appears superior for assessing cardiometabolic risk, but BMI still has value in certain contexts. WWI specifically targets central adiposity, making it more relevant for metabolic disease prediction. Your healthcare provider can determine which measurements are most appropriate for your situation.
Q: How often should I measure my WWI?
A: For general monitoring, every 3-6 months is reasonable. If you're actively trying to lose weight or manage a chronic condition, monthly measurements can provide helpful feedback on your progress.
Q: Can WWI predict disease in people with normal weight?
A: Yes! This is one of WWI's major advantages. People with normal BMI but elevated WWI (indicating central obesity) still face increased cardiometabolic risk. This condition, sometimes called metabolically obese normal weight (MONW), is well-captured by WWI.
Q: What's a "good" WWI score?
A: Research is still establishing universal cutoffs, but generally, lower values indicate less central adiposity and lower risk. Your healthcare provider can interpret your WWI in the context of your other risk factors and overall health profile.
Q: Can medications affect my WWI?
A: Some medications can influence body composition and fat distribution. Steroids, certain psychiatric medications, and some diabetes drugs affect weight and fat storage patterns. Discuss medication effects with your healthcare provider.
Q: Does WWI apply to children and adolescents?
A: Most research has focused on adults. Pediatric applications of WWI are still being investigated, as children have different growth patterns and body composition changes during development.
Q: How quickly can I improve my WWI?
A: Meaningful improvements typically require consistent lifestyle changes over 2-3 months. Crash diets aren't recommended—sustainable, moderate caloric restriction combined with exercise produces the best long-term results for reducing visceral fat.
Q: Should I focus on WWI or waist circumference?
A: Both provide valuable information. Waist circumference alone is simpler but doesn't account for body size. WWI provides a normalized value that's more comparable across individuals of different sizes and more predictive of metabolic risk.
Take Action: Your Next Steps
Armed with this knowledge about Weight-Adjusted Waist Index, you're now better equipped to understand and manage your cardiometabolic health. Here's what to do next:
1. Calculate Your Baseline WWI
Grab a measuring tape and scale today. Calculate your starting WWI and record it somewhere you'll remember. This baseline measurement will help you track your progress over time.
2. Schedule a Healthcare Visit
Discuss WWI with your healthcare provider, especially if you have risk factors like hypertension, diabetes, or family history of cardiovascular disease. They can interpret your WWI alongside other clinical information and help develop a personalized prevention or management plan.
3. Implement Evidence-Based Lifestyle Changes
Don't wait for perfect—start with small, sustainable changes:
Add one more serving of vegetables daily
Take a 20-minute walk after dinner
Reduce sugary beverage consumption
Improve your sleep schedule
4. Monitor Your Progress
Remeasure your WWI every 1-3 months. Celebrate improvements and use setbacks as learning opportunities to refine your approach.
5. Stay Informed
Medical science evolves rapidly. Follow reputable health organizations and discuss new research with your healthcare team. The studies reviewed here represent cutting-edge evidence, but more research continues to emerge.
6. Spread the Word
Share this information with family and friends who might benefit. Cardiometabolic diseases are leading causes of death globally, but they're largely preventable with early identification and intervention.
Author’s Note
As a physician and clinical researcher, I have spent years observing how traditional measures such as BMI often fail to capture the true metabolic risk hidden beneath the surface. Many of my own patients have presented with “normal” BMI yet displayed significant visceral adiposity, insulin resistance, hypertension, and early cardiometabolic complications. These cases reinforced a simple truth: what matters most is not how much you weigh, but where you carry that weight.
The Weight-Adjusted Waist Index (WWI) represents an important advancement in our understanding of metabolic health. Its ability to identify central adiposity—without being distorted by overall body size or muscle mass—makes it a valuable addition to modern clinical assessment. The emerging evidence from large, high-quality studies between 2024 and 2025 demonstrates not just statistical significance, but meaningful clinical utility.
My intention with this article is to translate that growing body of research into clear, actionable insights for both healthcare professionals and individuals seeking better control over their metabolic health. Early detection of central obesity can prevent years of suffering, reduce healthcare costs, and—most importantly—save lives.
I encourage readers to use WWI as a complementary tool, not a standalone diagnostic, and to discuss their numbers with qualified healthcare providers. Scientific understanding continues to evolve, but one principle
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Individual circumstances vary, and treatment decisions should always be made in consultation with qualified healthcare professionals.
Related Articles
Lipoprotein(a): The Genetic Key to Cardiovascular Disease Risk | DR T S DIDWAL
Vitamin D Deficiency and Sarcopenia: The Critical Connection | DR T S DIDWAL
How to Prevent Sarcopenia: Fight Age-Related Muscle Loss and Stay Strong | DR T S DIDWAL
Who Gets Sarcopenia? Key Risk Factors & High-Risk Groups Explained | DR T S DIDWAL
Sarcopenia: The Complete Guide to Age-Related Muscle Loss and How to Fight It | DR T S DIDWAL
Best Exercises for Sarcopenia: Strength Training Guide for Older Adults | DR T S DIDWAL
References
Kunutsor, S. K., Jae, S. Y., & Laukkanen, J. A. (2025). Association between weight-adjusted waist index and cardiometabolic multimorbidity in older adults: Findings from the English Longitudinal Study of Ageing. GeroScience, 47, 6429–6438. https://doi.org/10.1007/s11357-025-01829-w
Liu, S., Yu, J., Wang, L., Zhang, X., Wang, F., & Zhu, Y. (2024). Weight-adjusted waist index as a practical predictor for diabetes, cardiovascular disease, and non-accidental mortality risk. Nutrition, Metabolism, and Cardiovascular Diseases, 34(11), 2498–2510. https://doi.org/10.1016/j.numecd.2024.06.012
Yang, Y., Huang, J., Wu, J., Li, X., Wang, Y., Chen, H., … Zhou, Z. (2025). Application value of weight-adjusted waist circumference index and cardiometabolic index in hypertensive patients with albuminuria: Results from the National Health and Nutrition Examination Survey 2005–2020. Renal Failure, 47(1). https://doi.org/10.1080/0886022X.2025.2506813
Yu, Z., Nie, Z., Zhang, Y., & Sun, T. (2025). The weight-adjusted-waist index predicts all-cause and cardiovascular mortality in hypertension. Frontiers in Cardiovascular Medicine, 12. https://doi.org/10.3389/fcvm.2025.1501551
Zheng, Y., Nie, Z., Zhang, Y., & Sun, T. (2025). The weight-adjusted-waist index predicts all-cause and cardiovascular mortality in hypertension. Frontiers in Cardiovascular Medicine, 12, 1501551. https://doi.org/10.3389/fcvm.2025.1501551