10 Warning Signs of Sarcopenia: How to Recognize Early Muscle Loss and Prevent Weakness
Learn the 10 early symptoms of sarcopenia—age-related muscle loss that affects strength, balance, and independence. Discover how to spot warning signs like fatigue, slower walking, and weakness early, and what steps can help you stay strong and active.
SARCOPENIA
DR T S DIDWAL MD
11/3/202514 min read
From Silent Decline to Functional Red Flags
Sarcopenia doesn't announce itself with dramatic symptoms. Instead, it creeps into your life disguised as "just getting old." You might blame fatigue on poor sleep, attribute weakness to lack of exercise, or dismiss slower movement as an inevitable part of aging. But sarcopenia is not inevitable—it's a progressive skeletal muscle disorder affecting 10-16% of the global elderly population, characterized by deteriorating muscle function and mass that increases your risk of falls, fractures, disability, and mortality.
The insidious nature of sarcopenia makes early recognition critical. By the time most people seek medical attention, they've already progressed from mild muscle loss to functional impairment. Understanding the warning signs allows for early intervention, when lifestyle modifications and targeted treatments are most effective.
This chapter focuses on the 10 most critical symptoms of sarcopenia—functional red flags that signal your muscles are weakening before the condition progresses to severe sarcopenia. These aren't subtle laboratory findings; they're real-world changes that affect your independence, safety, and quality of life.
Self-screening is your first line of defense. The European Working Group on Sarcopenia in Older People (EWGSOP2) recommends a structured diagnostic approach based on three pillars: muscle strength, muscle mass, and physical performance. The symptoms below map directly to these diagnostic criteria, helping you recognize when professional assessment becomes necessary.
This document discusses sarcopenia, a progressive skeletal muscle disorder characterized by the deterioration of muscle function and mass, affecting 10–16% of the global elderly population. This condition increases the risk of falls, fractures, disability, and mortality. Because sarcopenia often masks itself as "just getting old," early recognition of functional red flags is critical for effective intervention, which includes lifestyle changes and targeted treatments.
The European Working Group on Sarcopenia in Older People (EWGSOP2) recommends a structured diagnostic approach focused on three pillars: muscle strength, muscle mass, and physical performance (Cruz-Jentoft et al., 2019). The 10 warning signs below map directly to these criteria.
The 10 Warning Signs of Muscle Loss
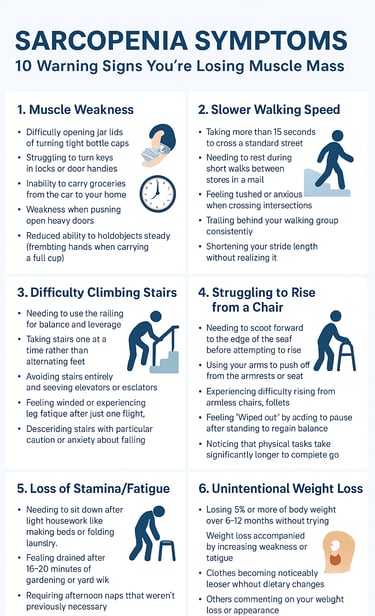
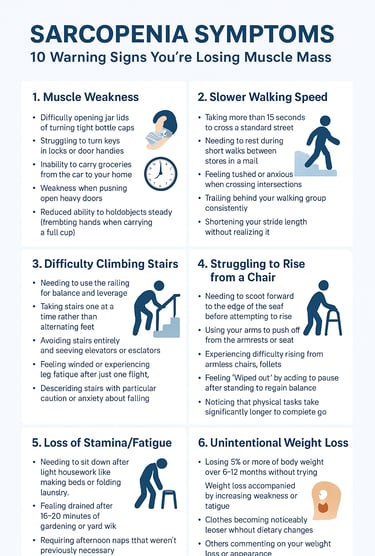
Warning Sign #1: Muscle Weakness
Functional Explanation:
Muscle weakness is the hallmark symptom of sarcopenia and the most reliable indicator according to EWGSOP2 guidelines. This isn't about feeling tired—it's about losing the physical capacity to perform tasks that were once effortless.
Common manifestations include:
Difficulty opening jar lids or turning tight bottle caps
Struggling to turn keys in locks or door handles
Inability to carry grocery bags from the car to your home
Weakness when pushing open heavy doors
Reduced ability to hold objects steady (trembling hands when carrying a full cup)
Why It Matters:
The EWGSOP2 identifies reduced muscle strength as the primary characteristic of sarcopenia, recommending it be assessed first in the diagnostic pathway. Grip strength, measured with a handheld dynamometer, serves as a simple proxy for overall muscle function. When grip strength falls below specific thresholds (typically <27 kg for men and <16 kg for women), sarcopenia should be suspected.
Muscle weakness reflects not just muscle mass loss but also deterioration in muscle quality, neuromuscular function, and the shift from fast-twitch (type II) to slow-twitch (type I) muscle fibers that occurs with aging.
Connection to Diagnosis: Sets up the Grip Strength Test, a cornerstone of sarcopenia screening that takes less than 5 minutes to perform.
Warning Sign #2: Slower Walking Speed
Functional Explanation:
You might notice you're the last one to reach the other side of a crosswalk, struggling to beat the pedestrian signal. Friends and family members naturally slow their pace to walk beside you. What once felt like a comfortable stride now requires conscious effort and concentration.
Specific examples include:
Taking more than 15 seconds to cross a standard street
Needing to rest during short walks between stores in a mall
Feeling rushed or anxious when crossing intersections
Trailing behind your walking group consistently
Shortening your stride length without realizing it
Why It Matters:
Gait speed is one of the most powerful predictors of adverse health outcomes in older adults, including hospitalization, disability, and mortality. A walking speed below 0.8 m/s (approximately 2.6 feet per second) is considered a critical threshold for poor physical performance in sarcopenia assessment.
Slow walking speed reflects multiple physiological impairments: reduced leg muscle strength, poor balance, decreased cardiovascular endurance, and compromised neuromuscular coordination. It's a functional integration of muscle weakness, making it an excellent screening tool.
Connection to Diagnosis: Directly ties to the gait speed criterion (≤0.8 m/s cutoff) measured in the Short Physical Performance Battery (SPPB) and used in sarcopenia severity staging.
Warning Sign #3: Difficulty Climbing Stairs
Functional Explanation:
Stairs become your nemesis. You find yourself gripping the railing tightly, pulling yourself up rather than pushing with your legs. You might pause halfway up a single flight to catch your breath or feel your thighs burning with exertion that seems disproportionate to the task.
Common experiences include:
Needing to use the railing for balance and leverage (when you never did before)
Taking stairs one at a time rather than alternating feet
Avoiding stairs entirely and seeking elevators or escalators
Feeling winded or experiencing leg fatigue after just one flight
Descending stairs with particular caution or anxiety about falling
Why It Matters:
Stair climbing requires significant lower extremity strength, balance, and coordination. It demands more muscle power than walking on level ground—your quadriceps, hamstrings, and gluteal muscles must generate force against gravity while maintaining stability. The inability to climb stairs efficiently indicates significant functional impairment and increased fall risk.
Research shows that difficulty with stair climbing strongly correlates with reduced type II (fast-twitch) muscle fiber capacity, which is preferentially lost in sarcopenia. These fibers are essential for generating the quick, powerful contractions needed for activities requiring strength and speed.
Connection to Diagnosis: Sets up timed stair climb tests and the SPPB (Short Physical Performance Battery), which includes a balance component that predicts stair-climbing ability.
Warning Sign #4: Struggling to Rise from a Chair
Functional Explanation:
Getting up from a seated position requires no thought—until it does. Suddenly, you find yourself rocking forward to build momentum, pushing off the armrests with both hands, or even needing multiple attempts to stand from low or soft chairs like sofas, car seats, or restaurant booths.
Specific scenarios include:
Needing to scoot forward to the edge of the seat before attempting to rise
Using your arms to push off from the armrests or seat
Experiencing difficulty rising from armless chairs, toilets, or low sofas
Feeling unsteady or needing to pause after standing to regain balance
Avoiding certain seating because you know you'll struggle to get up
Why It Matters:
The sit-to-stand movement is one of the most fundamental activities of daily living and a critical marker of functional independence. It requires coordinated activation of hip, knee, and ankle extensors, along with core stability. When these muscles weaken, independence erodes rapidly.
The 5-Time Chair Stand Test, where you rise from a chair five times without using your arms, is a validated assessment tool for lower limb strength. Taking longer than 15 seconds to complete this test indicates significant muscle weakness and predicts higher risk of disability and falls.
Connection to Diagnosis: Directly sets up the 5-Time Chair Stand Test, a core component of the SPPB and a recommended muscle strength assessment in EWGSOP2 guidelines.
Warning Sign #5: Loss of Stamina/Fatigue
Functional Explanation:
Activities that once filled your day—gardening, housework, grocery shopping, playing with grandchildren—now leave you exhausted. You need frequent rest breaks during previously manageable tasks. The fatigue feels disproportionate to the effort expended, and recovery takes longer than it used to.
Examples of abnormal fatigue include:
Needing to sit down after light housework like making beds or folding laundry
Feeling drained after 15-20 minutes of gardening or yard work
Requiring afternoon naps that weren't previously necessary
Feeling "wiped out" by activities like grocery shopping or preparing meals
Noticing that physical tasks take significantly longer to complete than before
Why It Matters:
Muscle tissue is metabolically active and contains mitochondria—the cellular powerhouses that generate energy. Sarcopenia involves mitochondrial dysfunction and reduced oxidative capacity, which impairs your muscles' ability to efficiently produce ATP (energy). This results in premature fatigue and reduced endurance.
Additionally, sarcopenia is associated with chronic low-grade inflammation (elevated cytokines like IL-6 and TNF-α), which contributes to systemic fatigue. The combination of reduced muscle mass, impaired energy metabolism, and inflammation creates a vicious cycle of declining stamina and activity avoidance.
Connection to Future Chapters: Sets up deep dives into mitochondrial dysfunction, chronic inflammation, anabolic resistance, and the metabolic consequences of muscle loss.
Warning Sign #6: Frequent Stumbling or Falls
Functional Explanation:
You catch your toe on rugs, miss curbs you used to navigate automatically, or lose your balance when reaching for objects. Perhaps you've had a close call—or an actual fall—that shook your confidence. You might avoid certain activities or environments because you no longer trust your balance.
Concerning patterns include:
Tripping over minor obstacles (thresholds, cords, uneven pavement)
Experiencing near-falls when turning quickly or changing direction
Losing balance when reaching overhead or bending down
Feeling unsteady on uneven surfaces like grass or gravel
Falling or nearly falling when getting up at night
Having had one or more actual falls in the past year
Why It Matters:
Falls are the most serious consequence of sarcopenia, representing the intersection of muscle weakness, poor balance, and slowed reaction time. In people over 65, falls are the leading cause of injury-related deaths and the primary reason for admission to assisted living facilities.
Sarcopenia impairs the rapid muscle contractions needed for protective responses when balance is threatened. Weakened leg muscles cannot generate the quick corrective steps needed to prevent a fall. Once a fall occurs, weak muscles also increase the risk of fractures, particularly hip fractures, which have devastating consequences for independence and mortality.
Connection to Future Chapters: This warning sign directly connects to chapters on balance training, fall prevention strategies, and the importance of resistance exercise for maintaining postural stability.
Warning Sign #7: Visible Muscle Shrinkage
Functional Explanation:
You notice your arms look thinner, your legs seem less defined, or your clothes fit differently—looser around the arms and legs. Rings might fit more loosely, or you notice more prominent bones at your wrists, ankles, or shoulders. These visual changes often prompt people to finally seek medical evaluation.
Observable changes include:
Noticeably thinner upper arms or forearms
Loss of calf muscle bulk (calf circumference <33 cm in women or <34 cm in men is concerning)
Visible reduction in thigh muscle mass
More prominent bony landmarks (collarbones, shoulder blades, ribs)
Clothing that once fit well now hangs loosely on the limbs
Watches, rings, or bracelets becoming looser
Why It Matters:
While functional symptoms like weakness appear first, visible muscle loss indicates more advanced sarcopenia. By the time muscle wasting becomes obvious, you may have already lost significant muscle mass—possibly 10-20% or more below your peak.
The EWGSOP2 defines sarcopenia as confirmed when both low muscle strength AND low muscle mass are present. Visual assessment isn't sufficient for diagnosis, but it should prompt formal body composition testing using DEXA (dual-energy X-ray absorptiometry), BIA (bioelectrical impedance analysis), or CT/MRI imaging.
Connection to Diagnosis: Sets up Chapter 6 on body composition assessment, including DEXA scans (Appendicular Skeletal Muscle Index <7.0 kg/m² for men, <6.0 kg/m² for women), BIA measurements, and clinical tools like calf circumference measurement.
Warning Sign #8: Unintentional Weight Loss
Functional Explanation:
The scale shows declining numbers despite no deliberate changes to your diet or activity level. This weight loss isn't gradual aging-related change—it's accelerated, unintended, and often accompanied by weakness rather than improved mobility.
Key characteristics of concerning weight loss:
Losing 5% or more of body weight over 6-12 months without trying
Weight loss accompanied by increasing weakness or fatigue
Clothes becoming noticeably looser without dietary changes
Others commenting on your weight loss or appearance
Loss of appetite or early satiety that contributes to reduced intake
Why It Matters:
Unintentional weight loss in older adults is a red flag for multiple conditions, but when accompanied by muscle weakness, it strongly suggests sarcopenia or its more severe form, cachexia. The distinction is critical:
Sarcopenia: Primary loss of muscle mass and function, potentially with stable or even increased fat mass (sarcopenic obesity)
Cachexia: Severe muscle wasting accompanied by systemic inflammation, often associated with cancer, heart failure, or chronic kidney disease
Unintentional weight loss accelerates muscle protein breakdown, impairs recovery from illness, and predicts poor outcomes including increased mortality risk. It requires immediate medical evaluation to identify underlying causes and initiate nutritional and therapeutic interventions.
Connection to Future Chapters: This symptom sets up the critical distinction between sarcopenia and cachexia, introduces protein requirements (1.2-1.5 g/kg/day for older adults), and connects to chapters on nutritional management and anabolic resistance.
Warning Sign #9: Reduced Resilience
Functional Explanation:
After a bout of flu, a minor surgery, or even a few days of bed rest due to injury, you notice it takes weeks—not days—to regain your previous strength and function. You might feel like you never quite get back to your baseline, with each illness or injury leaving you slightly weaker than before.
Examples of reduced resilience:
Taking 2-3 weeks to feel "normal" after a simple cold or flu
Experiencing prolonged weakness after hospitalization or surgery
Losing significant function after bed rest (difficulty walking after being bedridden for a week)
Needing extensive physical therapy after injuries that younger people recover from quickly
Noticing a cumulative decline—never quite returning to pre-illness function
Why It Matters:
Muscle resilience refers to your ability to maintain or quickly recover muscle mass and function after acute stressors. In sarcopenia, this resilience is dramatically impaired due to:
Anabolic resistance: Muscles become less responsive to protein intake and resistance exercise stimuli
Increased protein breakdown: Illness and inactivity trigger accelerated muscle catabolism
Impaired satellite cell function: Age-related decline in muscle stem cells slows repair and regeneration
Chronic inflammation: Elevated inflammatory cytokines interfere with muscle protein synthesis
This reduced resilience creates a downward spiral: each illness or period of inactivity causes disproportionate muscle loss, which increases vulnerability to the next stressor. Breaking this cycle requires proactive intervention, including adequate protein intake, early mobilization, and resistance exercise.
Connection to Future Chapters: Sets up chapters on acute illness management, protein requirements during stress/illness (up to 2.0 g/kg/day), bed rest protocols, and the critical importance of early mobilization during hospitalization.
Warning Sign #10: Difficulty Lifting Objects
Functional Explanation:
Objects that were once easy to lift—grandchildren, grocery bags, heavy pots, laundry baskets—now feel impossibly heavy. You might ask for help with tasks you once performed independently, or you avoid these activities altogether because they're too challenging or make you feel unsafe.
Specific functional losses include:
Inability to lift grandchildren or small pets
Struggling to lift a full laundry basket or move it from washer to dryer
Difficulty lifting heavy pots, cast iron pans, or large serving dishes
Trouble lifting suitcases or bags into car trunks or overhead compartments
Needing assistance to move furniture or carry heavy packages
Avoid cooking certain meals that require lifting heavy cookware
Why It Matters:
Lifting capacity reflects muscle power—the combination of strength and speed. It requires rapid recruitment of muscle fibers to generate force quickly. Power declines even faster than strength with aging, dropping by 3-4% per year after age 60, compared to 1-2% for strength alone.
The loss of lifting ability is a highly functional example of declining type II (fast-twitch) muscle fiber capacity. These fibers are preferentially lost in sarcopenia, reducing your ability to generate explosive force. This impacts not just lifting but also catching yourself during a near-fall, pushing off from a chair quickly, or any activity requiring rapid muscle contraction.
Loss of lifting capacity also represents a psychological threshold—a visible reminder of declining independence that often motivates people to finally seek help. It's a powerful motivator for intervention, as resistance training can significantly restore power even in advanced age.
Connection to Future Chapters: Sets up discussions of muscle power versus strength, type II fiber preservation, resistance training protocols emphasizing explosive movements, and the importance of functional training that mimics real-world lifting tasks.
When Multiple Warning Signs Appear Together
Sarcopenia rarely announces itself with a single symptom. Instead, you might notice a cluster of changes occurring over months or years. The presence of multiple warning signs significantly increases the likelihood of sarcopenia and the urgency of seeking assessment.
Risk stratification based on warning signs:
1 warning sign: Increased awareness and proactive monitoring recommended
2-3 warning signs: High suspicion for sarcopenia; clinical screening strongly recommended
4+ warning signs: Probable sarcopenia; immediate comprehensive assessment required
Falls + 2 other signs: Emergency red flag; indicates severe functional impairment
The interconnected nature of these symptoms reflects sarcopenia's multi-system impact. Muscle weakness leads to reduced activity, which accelerates further muscle loss. Fatigue reduces protein intake and exercise participation. Falls create fear and avoidance, further limiting physical activity. Each symptom amplifies the others, creating a downward spiral of declining function.
Breaking the cycle requires intervention at multiple levels:
Medical assessment to rule out treatable causes
Nutritional optimization with adequate protein intake
Progressive resistance training to rebuild strength
Balance and gait training to reduce fall risk
Treatment of underlying conditions (vitamin D deficiency, hormonal imbalances, chronic diseases)
Why These Symptoms Are Often Dismissed
Despite their significance, sarcopenia symptoms are frequently normalized or attributed to "just aging." Several factors contribute to this dangerous dismissal:
Cultural normalization of decline: Society expects older adults to become weaker and slower. This expectation becomes self-fulfilling, with both patients and healthcare providers failing to recognize treatable muscle loss.
Gradual onset: Unlike acute injuries, sarcopenia develops slowly over years. The insidious progression allows for psychological adaptation, with people unconsciously adjusting their activities and expectations to match declining capacity.
Lack of awareness: Many people—including some healthcare providers—have never heard the term "sarcopenia" and don't recognize it as a distinct medical condition with evidence-based treatments.
Fear of diagnosis: Some older adults avoid seeking help because they fear being told "nothing can be done" or being prescribed medications they don't want. They don't realize that sarcopenia responds exceptionally well to non-pharmaceutical interventions like resistance training and nutrition optimization.
Overlap with other conditions: Sarcopenia symptoms often coexist with arthritis, cardiovascular disease, diabetes, and other age-related conditions, making it difficult to isolate muscle-specific problems.
The cost of dismissal is steep. Untreated sarcopenia progresses to severe functional impairment, disability, loss of independence, increased healthcare utilization, and significantly elevated mortality risk. Early recognition and intervention can reverse or dramatically slow this progression.
Conclusion: When to Seek Professional Assessment
If you recognize two or more of these warning signs in yourself or a loved one, don't wait. These symptoms are not inevitable consequences of aging—they're clinical indicators of a diagnosable and treatable condition.
Your next critical steps:
Document your symptoms: Note which warning signs you're experiencing, when they started, and how they've progressed. Specific examples help healthcare providers understand the functional impact.
Complete a self-screening tool: The SARC-F questionnaire is a validated 5-question screening tool you can complete in under 2 minutes. A score ≥4 indicates high sarcopenia risk and warrants clinical assessment.
Schedule a comprehensive evaluation: Request specific sarcopenia assessment including grip strength measurement, gait speed testing, and muscle mass evaluation (ideally DEXA scan or BIA).
Don't accept "it's just aging" as an answer: Sarcopenia is a specific muscle disorder, not normal aging. Effective interventions exist, including resistance training, protein optimization, vitamin D supplementation, and treatment of underlying conditions.
The diagnostic pathway ahead:
The EWGSOP2 recommends a structured, three-step approach:
Find: Screen for sarcopenia using simple tools (SARC-F questionnaire, calf circumference)
Assess: Measure muscle strength (grip strength, chair stand test)
Confirm: Quantify muscle mass (DEXA, BIA, CT, or MRI)
Severity: Evaluate physical performance (gait speed, SPPB)
Early intervention is transformative. Studies consistently show that even individuals in their 80s and 90s can achieve significant strength gains (20-100% increases) with just 8-12 weeks of resistance training. Combining exercise with adequate protein intake (1.2-1.5 g/kg/day) and vitamin D optimization can restore function, reduce fall risk, and preserve independence.
Moving Forward: From Recognition to Action
Sarcopenia—age-related loss of muscle strength and mass—is not just a normal part of aging. It’s a serious but treatable condition that can affect your independence, balance, and quality of life. Recognizing the early warning signs is the key to stopping it before it causes lasting harm.
Be alert to changes like increasing muscle weakness, slower walking speed, difficulty climbing stairs or rising from a chair, frequent tiredness, and unintentional weight loss. You may also notice that everyday tasks—like carrying groceries, lifting objects, or keeping up with others while walking—feel harder than they used to. These are not simply signs of “getting older”; they may indicate that your muscles are losing strength.
If you experience two or more of these symptoms, talk to your doctor about sarcopenia screening. Tests such as grip strength, gait speed, and body composition (DEXA or BIA) can detect early muscle decline. The good news is that sarcopenia can be improved with the right approach—regular resistance exercise, sufficient protein intake, vitamin D, and staying physically active.
By identifying these 10 warning signs early, you can protect your strength, reduce fall risk, and maintain independence as you age. Awareness is the first step toward action—and recovery.
Key Takeaways
✓ Sarcopenia affects 10-16% of older adults globally but often goes unrecognized because symptoms are dismissed as "normal aging"
✓ The 10 warning signs map directly to diagnostic criteria for strength, mass, and physical performance
✓ Muscle weakness (Warning Sign #1) is the primary characteristic and should trigger immediate screening
✓ Falls combined with any other warning signs represent a medical emergency requiring urgent assessment
✓ Recognition of ≥2 warning signs warrants formal clinical evaluation including grip strength, gait speed, and muscle mass measurement
✓ Early intervention with resistance training, protein optimization, and targeted treatments can dramatically reverse functional decline
✓ Don't wait for severe symptoms—the earlier sarcopenia is diagnosed, the more effectively it can be treated
This information is for educational purposes only and should not replace professional medical advice. Always consult with your healthcare provider for personalized recommendations based on your individual health status and risk factors.
Related Articles
Sarcopenia vs. Osteoporosis: Key Differences for Bone & Muscle Health | DR T S DIDWAL
Sarcopenia: The Complete Guide to Age-Related Muscle Loss and How to Fight It | DR T S DIDWAL
Citations
Mao, X., Lv, K., Qi, W. et al. Research progress on sarcopenia in the musculoskeletal system. Bone Res 13, 78 (2025). https://doi.org/10.1038/s41413-025-00455-8
Chung, J. Y., Kim, S. G., Kim, S. H., & Park, C. H. (2025). Sarcopenia: how to determine and manage. Knee surgery & related research, 37(1), 12. https://doi.org/10.1186/s43019-025-00265-6
Cruz-Jentoft, A. J., Bahat, G., Bauer, J., Boirie, Y., Bruyère, O., Cederholm, T., Cooper, C., Landi, F., Rolland, Y., Sayer, A. A., Schneider, S. M., Sieber, C. C., Topinkova, E., Vandewoude, M., Visser, M., Zamboni, M., & Writing Group for the European Working Group on Sarcopenia in Older People 2 (EWGSOP2), and the Extended Group for EWGSOP2 (2019). Sarcopenia: revised European consensus on definition and diagnosis. Age and ageing, 48(1), 16–31. https://doi.org/10.1093/ageing/afy169