Sarcopenia: The Complete Guide to Age-Related Muscle Loss and How to Fight It
Sarcopenia isn’t inevitable. Learn how resistance training, high-protein meals, and Vitamin D can help you build strength and independence as you age.
SARCOPENIA
DR T S DIDWAL MD
11/2/202514 min read
Sarcopenia is often mistakenly dismissed as a natural, unavoidable part of getting older. However, this progressive condition—the age-related loss of skeletal muscle mass, strength, and function—is now recognized as a distinct disease (ICD-10 code M62.84). Far from being inevitable, sarcopenia can be significantly slowed, mitigated, and often reversed with targeted, evidence-based interventions.
This comprehensive guide serves as your essential resource for understanding sarcopenia, from its root causes and modern diagnostic criteria to the most effective strategies for prevention and treatment, empowering you to maintain strength, independence, and a high quality of life well into your later years.
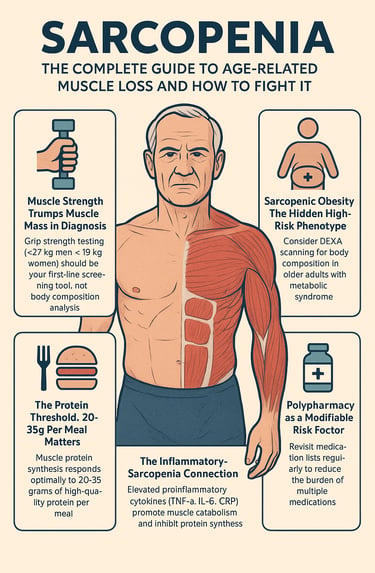
Clinical Pearls:
1. Muscle Strength Trumps Muscle Mass in Diagnosis.
The EWGSOP2 2019 revision fundamentally shifted sarcopenia diagnosis by prioritizing low muscle strength as the primary criterion for "probable sarcopenia," with muscle quantity measurements only needed for confirmation. This reflects mounting evidence that strength, rather than mass alone, better predicts functional decline and adverse outcomes. Clinically, this means grip strength testing (<27 kg men, <16 kg women) should be your first-line screening tool, not body composition analysis.
2. Sarcopenic Obesity: The Hidden High-Risk Phenotype
Patients with sarcopenic obesity—simultaneous low muscle mass and elevated body fat, particularly visceral adiposity—face disproportionately worse outcomes than those with either condition alone, including dramatically elevated 10-year mortality risk. This phenotype is easily missed on routine examination since BMI may appear normal or only moderately elevated. Consider DEXA scanning for body composition in older adults with metabolic syndrome, even if they don't appear overtly obese.
3. The Protein Threshold: 20-35g Per Meal Matters
The PROT-AGE study group's recommendation of 1.0-1.2 g/kg daily protein intake isn't the full story—distribution matters equally. Muscle protein synthesis responds optimally to 20-35 grams of high-quality protein per meal, with leucine-rich sources (whey protein, lean meats) being particularly effective. A patient consuming 90g of protein daily, but concentrated in one meal, will have inferior outcomes compared to someone spreading similar intake across three meals. This has immediate practical implications for meal planning in older adults.
4. The Inflammatory-Sarcopenia Connection
Elevated proinflammatory cytokines (TNF-α, IL-6, CRP) don't just correlate with sarcopenia—they directly cause muscle wasting by promoting myofibrillar protein breakdown and inhibiting synthesis. This explains why sarcopenia accelerates in chronic inflammatory conditions (COPD, RA, CKD) and why patients with these comorbidities need more aggressive preventive strategies. Consider sarcopenia screening as routine in any patient with chronic inflammatory disease, regardless of age.
5. Polypharmacy as a Modifiable Risk Factor
Recent systematic reviews demonstrate that polypharmacy (≥5 medications) is associated with a 65% increased sarcopenia prevalence (OR 1.65). The mechanism likely involves multiple pathways: reduced appetite, altered nutrient absorption, medication-induced fatigue limiting activity, and direct muscle-toxic effects of certain drugs. Deprescribing studies in sarcopenic patients show improved functional outcomes and discharge-to-home rates. Regular medication reviews with explicit consideration of sarcopenia risk should be standard practice in older adults.
Defining the Silent Epidemic: What is Sarcopenia?
The term "sarcopenia" is derived from the Greek words sarx (flesh) and penia (loss or poverty), literally translating to the "poverty of flesh." First proposed by Dr Irwin Rosenberg in 1989, the definition of this condition has evolved to emphasize not just the loss of muscle tissue, but the critical decline in its functionality.
The Dual Mechanism of Muscle Decline
Sarcopenia is characterised by a significant decrease in both the number and size of muscle fibers. This dual mechanism leads to:
Fewer Fibers Overall: A degeneration of motor neurons and neuromuscular junctions (neurodegeneration) leads to the progressive denervation and subsequent loss of muscle fibers, particularly the fast-twitch (Type II) fibers essential for strength and power.
Shrinking of Remaining Fibers: The fibers that remain undergo atrophy, or shrinking, due to a reduced capacity for protein synthesis and increased rates of muscle protein breakdown.
Sarcopenia vs. Related Conditions
Understanding sarcopenia requires distinguishing it from two similar, but distinct, conditions:
Sarcopenia, frailty, and cachexia are distinct but related conditions characterized by muscle decline. Sarcopenia is defined as the loss of muscle mass and function primarily due to age, although this process is accelerated by lifestyle factors and disease. Frailty, a broader syndrome, is a clinical state of increased vulnerability resulting from multi-system impairment, typically diagnosed by the presence of at least three factors: unintentional weight loss, exhaustion, muscle weakness, slow walking speed, and low physical activity. Finally, Cachexia is a severe form of muscle and weight loss that is specifically driven by underlying chronic diseases like cancer or heart failure, and is distinguished by high levels of disease-associated inflammation and profound metabolic disturbances.
Epidemiology: How Common is Sarcopenia?
Sarcopenia is a growing public health concern, directly linked to increased falls, hospitalizations, frailty, and mortality.
Prevalence: After the age of 30, adults begin to lose muscle mass at a rate of approximately 3–5% per decade. This process accelerates between the ages of 65 and 80.
Older Adults: The prevalence is estimated to affect 5–13% of adults aged 60 and older.
Advanced Age: For individuals over 80, the prevalence dramatically increases, ranging from 11% to 50%.
The increasing clarity of diagnostic criteria from groups like the European Working Group on Sarcopenia in Older People (EWGSOP) and the Asian Working Group for Sarcopenia (AWGS) is crucial for accurately tracking and treating this widespread condition.
The Root Causes: Why Muscle Mass Declines
Sarcopenia is a multifactorial condition driven by a complex interplay of age-related biological changes and modifiable lifestyle factors.
Biological & Hormonal Drivers
Hormonal Decline: The aging process naturally reduces levels of anabolic hormones—those responsible for building and maintaining muscle tissue.
Testosterone, Growth Hormone (GH), and IGF-1 (Insulin-like Growth Factor 1) levels all decline with age, impairing muscle protein synthesis and regeneration capacity.
Estrogen decline post-menopause in women also contributes to impaired muscle performance.
Neurological Changes (Neurodegeneration): Age-related neurodegeneration causes a loss of motor neurons, especially those that supply fast-twitch (Type II) muscle fibers. This disruption in communication between the brain and the muscle (the neuromuscular junction) leads to the eventual death and atrophy of the affected muscle fibers.
Chronic Inflammation: Older adults often exhibit a state of chronic, low-grade systemic inflammation, sometimes called "inflammaging." Elevated levels of pro-inflammatory cytokines, such as TNF-alpha and IL-6, directly promote muscle protein breakdown (catabolism) and inhibit synthesis.
Satellite Cell Dysfunction: Satellite cells are skeletal muscle-specific stem cells critical for muscle repair and regeneration. With age, the number and proliferative capacity of these cells decline, impairing the muscle's ability to recover from damage and maintain mass.
Lifestyle & Nutritional Factors
Physical Inactivity: This is arguably the most modifiable risk factor. Sedentary behavior is a powerful accelerator of muscle loss. The muscular system requires consistent challenge (stress) to stimulate maintenance and growth signals. Lack of activity removes this critical stimulus, favoring atrophy.
Inadequate Protein Intake: Many older adults fail to consume enough high-quality protein to meet the elevated needs of aging muscle. Older muscle is less responsive to lower amounts of protein, a phenomenon known as "anabolic resistance."
Vitamin D Deficiency: Vitamin D is crucial for muscle function, binding to receptors on muscle fibers and influencing their size and strength. Deficiency is highly prevalent in older adults and is independently linked to loss of muscle mass and reduced strength.
The Dual Threat: Sarcopenic Obesity
An increasingly common and dangerous condition is sarcopenic obesity—the co-existence of low muscle mass and high body fat, especially visceral fat. This combination significantly increases the risk for metabolic syndrome, functional disability, and mortality, as the pro-inflammatory environment of excess fat accelerates muscle breakdown.
Sarcopenia diagnosis has been standardised by major consensus groups (EWGSOP2 and AWGS) using a three-pronged framework: low muscle strength, low muscle quantity (mass), and poor physical performance.
The EWGSOP2 recommends a four-step Find-Assess-Confirm-Severity (F-A-C-S) diagnostic pathway:
1. Find (Case-Finding)
The initial step screens for risk using simple tools or clinical suspicion.
SARC-F Questionnaire: A quick, five-question self-assessment (Strength, Assistance with walking, Rising from a chair, Climbing stairs, Falls). A score of 4 or higher suggests probable sarcopenia and warrants further assessment.
Calf Circumference: The AWGS recommends this for early case-finding, with cutoffs of <34 cm for men and <33 cm for women.
2. Assess (Muscle Strength)
Muscle strength is considered the most reliable functional measure and the primary diagnostic criterion for Probable Sarcopenia.
Handgrip Strength: Measured with a dynamometer. Cutoffs for concern: <27 kg for men and <16 \kg for women (EWGSOP2).
Five-Time Chair Stand Test: Measures lower body strength and power. Taking >15 seconds to complete five rises from a chair suggests impaired strength.
3. Confirm (Muscle Quantity/Quality)
If muscle strength is low, sarcopenia is Confirmed by measuring muscle quantity or quality.
DEXA Scan (Dual-Energy X-ray Absorptiometry): The gold standard for measuring Appendicular Lean Mass (ALM)—the muscle mass in the arms and legs. It provides highly accurate baseline measurements and is essential for monitoring treatment efficacy.
Sarcopenia is confirmed if Low Strength AND Low ALM/height (e.g., <7.0 kg/m} for men, <5.5 kg/m} for women, per EWGSOP2).
Bioelectrical Impedance Analysis (BIA): A more portable and less expensive alternative to DEXA for estimating muscle mass.
CT/MRI: Used primarily in research settings; provides highly detailed measurements of muscle area and quality (fat infiltration).
4. Severity (Physical Performance)
If both strength and quantity are low, the condition is classified as Severe Sarcopenia based on poor physical performance.
Gait Speed: The most common measure. A walking speed of 0.8 meters per second indicates severe sarcopenia and a high risk of falls and adverse outcomes.
Short Physical Performance Battery (SPPB): A score of 8 points (out of 12) on this battery of tests (gait speed, balance, chair stands) indicates poor performance.
Treatment and Prevention: Your Action Plan
Sarcopenia is not a one-way street. The most potent medicine is a combination of targeted exercise and optimized nutrition.
Exercise: The Foundation of Muscle Health
Resistance Training is the single most critical intervention for both preventing and treating sarcopenia. It stimulates muscle protein synthesis and promotes anabolic signaling (Akt/mTOR pathway), directly combating muscle loss and improving function.
The key principle is Progressive Overload—gradually increasing the challenge (weight, reps, sets) over time to continually stimulate muscle adaptation and growth.
Resistance training for sarcopenia is typically structured across three progressive levels. The Beginner Program, recommended for 2–3 sessions per week, focuses on mastering basic movement patterns using bodyweight or light weights, to build foundational strength and stability through exercises like chair-assisted squats, wall push-ups, and supported single-leg stands. The Intermediate Program, performed 3 sessions per week, introduces light-to-moderate weights and compound movements, aiming to increase muscle size (hypertrophy) and functional strength with exercises such as weighted squats, dumbbell rows, lunges, and overhead presses. Finally, the Advanced Program, completed 3–4 sessions per week, focuses on heavy, compound movements (and should involve consulting a professional) to maximize absolute strength and muscle mass, utilizing exercises like barbell squats, Romanian deadlifts, bench press, and pull-ups or lat pulldowns.
Balance and Aerobic Exercise: While resistance training builds muscle, aerobic activities (like walking) improve cardiorespiratory health, and balance exercises (like single-leg stands) are crucial for reducing the risk of falls, a primary consequence of sarcopenia.
Nutrition: Fueling the Anabolic Engine
Muscle protein synthesis requires a consistent supply of amino acids, particularly the branched-chain amino acid leucine. Older adults require a higher protein intake to overcome anabolic resistance.
Optimizing nutrition is crucial for fighting sarcopenia, with a focus on protein intake and Vitamin D levels. Older adults should target a higher protein intake of 1.0 \to 1.2 grams of protein per kilogram of body weight daily (exceeding the standard 0.8 \text g/kg) to effectively optimize muscle protein synthesis (MPS) signals. Furthermore, the timing of intake is key; aim to distribute the protein evenly throughout the day, ensuring 20 to 35 grams of high-quality protein at each major meal to maximise MPS around the clock. Excellent sources of this high-quality protein, which provide complete amino acid profiles, include lean meats, fish (like salmon), eggs, dairy products (such as Greek yoghurt and cottage cheese), and whey protein supplements. Finally, it's vital to maintain adequate Vitamin D levels, often requiring supplementation of $800 \text{–} 2000 \text{ IU/day}$, as Vitamin D directly supports muscle fiber size and function.
Sample Daily Goal (for a 75 kg adult, targeting 1.2 g/kg)
Total daily protein: 90 grams
Breakfast: 25 g e.g., Greek yoghurt & eggs)
Lunch: 30 g (e.g., Grilled chicken or fish)
Dinner: 35 g(e.g., Lean steak or salmon)
Conclusion: Your Path to Stronger Aging
Sarcopenia is a formidable opponent in the journey of aging, contributing to frailty, loss of independence, and increased mortality. Yet, the science is clear: it is highly modifiable.
The strategies outlined in this guide—from the precision tracking of a DEXA scan to the consistent application of progressive resistance training and optimised protein nutrition—provide a proven, actionable blueprint for maintaining and rebuilding muscle health.
Don't wait for symptoms to become severe. Whether you are seeking prevention or actively managing muscle loss, the time to challenge and fuel your body is now. Taking action early is the most powerful determinant of a stronger, more independent future.
Frequently Asked Questions
Q1: At what age should I start worrying about sarcopenia?
A: While sarcopenia primarily affects those over 60, muscle loss actually begins around age 30, with approximately 3-5% loss per decade initially. The process accelerates significantly between the ages of 65-80. The key is that prevention should start much earlier than most people think—ideally in your 40s and 50s. If you're over 30 and sedentary, you're already experiencing gradual muscle loss. If you're over 60, screening becomes important even if you feel fine, since sarcopenia often develops silently before functional symptoms appear. Think of it like heart disease prevention—the earlier you start, the better your outcomes.
Q2: Can sarcopenia be reversed, or just slowed down?
A: Great news—sarcopenia can often be partially reversed, not just slowed. Multiple studies demonstrate that progressive resistance training can increase both muscle mass and strength even in people over 80 with confirmed sarcopenia. When combined with adequate protein intake (1.0-1.2 g/kg daily), many patients see measurable improvements in muscle quantity, grip strength, and functional performance within 3-6 months. However, complete reversal to youthful muscle mass isn't realistic. The goal is meaningful improvement in strength, function, and independence. The earlier you intervene, the better your potential for recovery.
Q3: I'm vegetarian/vegan—can I still prevent or treat sarcopenia without eating meat?
A: Absolutely. While animal proteins are "complete" proteins containing all essential amino acids, plant-based diets can effectively prevent and treat sarcopenia with proper planning. Focus on combining complementary proteins (beans with rice, hummus with whole grain bread) and emphasize high-quality plant proteins like legumes, quinoa, tofu, tempeh, nuts, and seeds. You may need to consume slightly more total protein since plant proteins are sometimes less efficiently absorbed. Consider supplementing with pea or soy protein powder, both of which have shown effectiveness in sarcopenia studies. Ensure adequate vitamin D and B12 intake, as deficiencies are more common in plant-based diets and can worsen muscle health.
Q4: How is sarcopenia different from just "getting old and weak"?
A: This is a crucial distinction. While some muscle changes occur with normal aging, sarcopenia is a diagnosable disease (ICD-10 code M62.84) with specific criteria, serious health consequences, and evidence-based treatments. Normal aging might mean slightly reduced strength, but sarcopenia means losing independence—struggling to rise from chairs, increased fall risk, higher mortality rates, and complications after surgery. The difference is between "I'm not as strong as I used to be" and "I can't safely live independently." Importantly, sarcopenia isn't inevitable—with proper intervention, many people maintain excellent muscle function into their 80s and beyond.
Q5: Will taking protein supplements alone help my sarcopenia?
A: Protein supplements help, but they're not a standalone solution. Research shows that nutritional supplementation with whey protein, leucine, and vitamin D increases muscle mass in sarcopenia patients. However, when combined with exercise, the results are dramatically better—improving not just mass but also strength and physical function. Without resistance training, your body has limited stimulus to build muscle even with adequate protein. Think of protein as building materials and exercise as the blueprint and construction crew. You need both. If you're struggling to meet protein targets through food alone (common in older adults with reduced appetite), supplements can be valuable, but pair them with at least twice-weekly strength training.
Q6: My doctor said my DEXA scan shows low muscle mass, but I feel fine—should I be concerned?
A: Yes, this warrants attention even without symptoms. DEXA can detect low muscle mass years before functional decline becomes apparent—this is actually the ideal time to intervene. You're in the "probable" or "confirmed" sarcopenia stage but haven't progressed to "severe" with physical performance impairment. Starting resistance training and optimizing protein intake now can prevent you from ever experiencing the disabling symptoms. It's similar to finding high cholesterol before you've had a heart attack—the absence of symptoms doesn't mean absence of risk. Consider this an opportunity for prevention rather than waiting for treatment to become necessary.
Q7: I have knee osteoarthritis—is it safe to do resistance training, and will it help or hurt?
A: Resistance training is not only safe for most people with knee osteoarthritis but can actually help both conditions. Research shows sarcopenia and osteoarthritis commonly coexist, with sarcopenia potentially contributing to osteoarthritis development through altered muscle composition. Appropriate strengthening exercises improve the muscle support around your knee joint, potentially slowing osteoarthritis progression. However, you need a tailored approach—start with low-impact exercises, avoid high-impact activities that stress the joint, and work with a physical therapist to design a program that builds muscle without aggravating your arthritis. Studies show resistance training improves both sarcopenia and osteoarthritis outcomes when done correctly. If you're considering knee replacement, managing sarcopenia beforehand significantly improves surgical outcomes and reduces complication rates.
A Message of Hope: Your Path Forward
If you're reading this because you're concerned about muscle loss, weakness, or maintaining your independence as you age, take heart—you're already taking the most important first step, which is awareness.
Here's what I want you to understand: Sarcopenia is not a life sentence. Unlike many age-related conditions, this is one where your daily actions truly matter. The person who starts resistance training at 70 can be stronger and more functional than someone a decade younger who remains sedentary. That's remarkable when you think about it—you have real control here.
Yes, the science can feel overwhelming with its talk of cytokines, protein synthesis, and diagnostic criteria. But the practical message is beautifully simple: Move your muscles against resistance regularly, feed them well with adequate protein throughout the day, and monitor your progress. These aren't complicated interventions requiring expensive treatments or invasive procedures. They're fundamental lifestyle choices that yield powerful results.
If you're struggling with weakness, difficulty climbing stairs, or finding daily tasks harder than they used to be, please don't dismiss it as inevitable aging. Talk to your doctor. Get tested. A simple grip strength measurement and a DEXA scan can tell you exactly where you stand and, more importantly, help you track your improvement over time.
And if you're younger—in your 40s, 50s, or early 60s—and thinking this doesn't apply to you yet, remember that preventing sarcopenia is far easier than reversing it. The strength training you do today is an investment in your independence 20 and 30 years from now.
You have the power to age strong. Start today, stay consistent, and watch yourself prove that the number of candles on your birthday cake doesn't have to dictate your strength, vitality, or independence.
This information is for educational purposes only and should not replace professional medical advice. Always consult with your healthcare provider for personalized recommendations based on your individual health status and risk factors.
Related Articles
Prevent Sarcopenia & Osteoporosis: Your Guide to Strong Bones & Muscles | DR T S DIDWAL
Sarcopenia Diet Plan: What to Eat to Maintain Muscle Mass After 50 | DR T S DIDWAL
How to Prevent Sarcopenia: Fight Age-Related Muscle Loss and Stay Strong | DR T S DIDWAL
Who Gets Sarcopenia? Key Risk Factors & High-Risk Groups Explained | DR T S DIDWAL
Best Exercises for Sarcopenia: Strength Training Guide for Older Adults | DR T S DIDWAL
Citations
Chung, J. Y., Kim, S. G., Kim, S. H., & Park, C. H. (2025). Sarcopenia: how to determine and manage. Knee surgery & related research, 37(1), 12. https://doi.org/10.1186/s43019-025-00265-6
Chen, L. K., Woo, J., Assantachai, P., Auyeung, T. W., Chou, M. Y., Iijima, K., Jang, H. C., Kang, L., Kim, M., Kim, S., Kojima, T., Kuzuya, M., Lee, J. S. W., Lee, S. Y., Lee, W. J., Lee, Y., Liang, C. K., Lim, J. Y., Lim, W. S., Peng, L. N., … Arai, H. (2020). Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. Journal of the American Medical Directors Association, 21(3), 300–307.e2. https://doi.org/10.1016/j.jamda.2019.12.012
Cruz-Jentoft, A. J., Bahat, G., Bauer, J., Boirie, Y., Bruyère, O., Cederholm, T., Cooper, C., Landi, F., Rolland, Y., Sayer, A. A., Schneider, S. M., Sieber, C. C., Topinkova, E., Vandewoude, M., Visser, M., Zamboni, M., & Writing Group for the European Working Group on Sarcopenia in Older People 2 (EWGSOP2), and the Extended Group for EWGSOP2 (2019). Sarcopenia: revised European consensus on definition and diagnosis. Age and ageing, 48(1), 16–31. https://doi.org/10.1093/ageing/afy169
Bauer, J., Biolo, G., Cederholm, T., Cesari, M., Cruz-Jentoft, A. J., Morley, J. E., Phillips, S., Sieber, C., Stehle, P., Teta, D., Visvanathan, R., Volpi, E., & Boirie, Y. (2013). Evidence-based recommendations for optimal dietary protein intake in older people: a position paper from the PROT-AGE Study Group. Journal of the American Medical Directors Association, 14(8), 542–559. https://doi.org/10.1016/j.jamda.2013.05.021
ICD-10 Code for Sarcopenia- M62.84- codify by AAPC. (n.d.). https://www.aapc.com/codes/icd-10-codes/M62.84