Sarcopenia vs. Osteoporosis: Key Differences for Bone & Muscle Health
Don't let aging steal your strength. Get the facts on preventing sarcopenia and osteoporosis with optimal nutrition, resistance training, and early diagnosis (DXA, SARC-F).
SARCOPENIA
DR T S DIDWAL MD
11/3/20259 min read
Sarcopenia vs. Osteoporosis: Understanding the Key Differences for Better Health
As our global population ages, two silent conditions are emerging as major health concerns: sarcopenia and osteoporosis. While both affect older adults and can significantly impact quality of life, they target different body systems and require distinct approaches to prevention and treatment. Understanding the key differences between these conditions is essential for maintaining health and independence in later years.
Clinical Pearls
Muscle and Bone Are Biologically Interconnected:
Muscle contractions provide mechanical loading that stimulates bone formation. Sarcopenia indirectly worsens osteoporosis by reducing bone stress signals—highlighting the need for combined muscle-bone interventions.Hormonal Crosstalk Drives Both Conditions:
Declining levels of estrogen, testosterone, growth hormone, and IGF-1 contribute simultaneously to bone resorption and muscle atrophy, explaining why both disorders often emerge post-menopause or after age 60.Inflammation Accelerates Degeneration:
Elevated cytokines such as IL-6 and TNF-α disrupt both osteoblast and myocyte function, linking chronic low-grade inflammation (“inflammaging”) to the progression of both sarcopenia and osteoporosis.DXA Can Assess Both Bone and Muscle:
While primarily used for bone mineral density (BMD), modern DXA technology can also quantify appendicular lean mass—offering a single, dual-purpose diagnostic tool for both conditions.Resistance Training Is the Most Potent Dual Therapy:
Progressive resistance exercise not only reverses muscle loss but also enhances bone density by increasing mechanical load and anabolic hormone activity—making it the cornerstone of prevention and rehabilitation.
What Is Osteoporosis?
Osteoporosis is a skeletal disorder characterized by reduced bone density and deterioration of bone tissue, making bones fragile and susceptible to fractures. Often called the "silent disease," osteoporosis progresses without symptoms until a fracture occurs—typically in the hip, spine, or wrist.
Key Facts About Osteoporosis:
Definition: Bone mineral density (BMD) more than 2.5 standard deviations below the young adult mean
Global Impact: Over 200 million people worldwide are affected
Primary Risk: Fractures that can lead to disability, loss of independence, and increased mortality
Most Affected: Postmenopausal women and elderly populations
How Osteoporosis Develops
Bone is living tissue that continuously remodels through a balanced process of formation (by osteoblasts) and breakdown (by osteoclasts). Osteoporosis occurs when bone resorption outpaces bone formation, resulting in porous, weakened bones.
The most common form, postmenopausal osteoporosis, develops when declining estrogen levels after menopause accelerate bone loss. Other causes include chronic diseases, certain medications (especially corticosteroids), hormonal disorders, and nutritional deficiencies.
What Is Sarcopenia?
Sarcopenia refers to the progressive, age-related loss of skeletal muscle mass, strength, and function. Coined in 1989, this condition affects physical performance, increases fall risk, and reduces functional independence.
Key Facts About Sarcopenia:
Prevalence: Affects 5-13% of people in their 70s and 11-50% by age 80
Future Impact: Expected to affect over 500 million older adults by 2050
Diagnosis Criteria: Requires low muscle strength, low muscle quantity/quality, and/or low physical performance
Severity Levels: Ranges from probable to confirmed to severe sarcopenia
How Sarcopenia Develops
Sarcopenia results from an imbalance between muscle protein synthesis and breakdown. Multiple factors contribute to this process, including chronic inflammation, hormonal changes (reduced testosterone and growth hormone), mitochondrial dysfunction, oxidative stress, and altered neuromuscular signaling.
As we age, increased inflammatory cytokines and decreased anabolic hormones disrupt muscle homeostasis, leading to progressive muscle tissue loss.
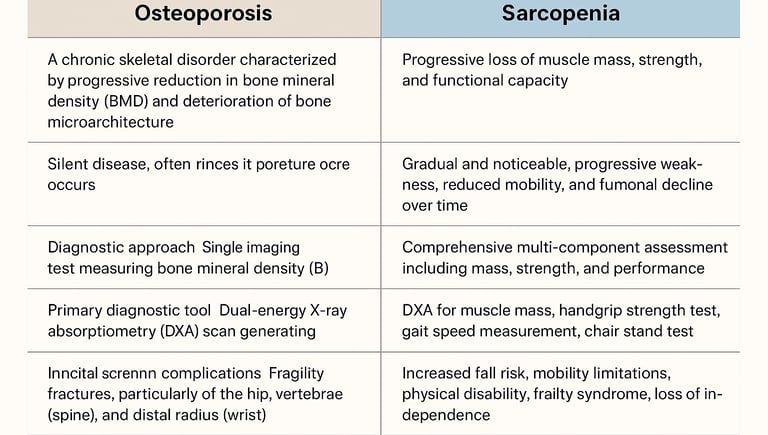
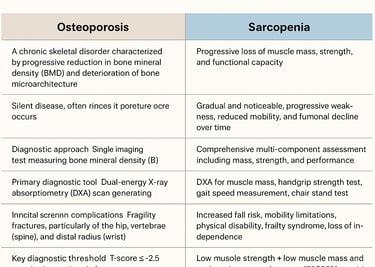
The Critical Differences: Sarcopenia vs. Osteoporosis
While osteoporosis and sarcopenia share several risk factors and often coexist, they are fundamentally different conditions affecting distinct body systems. Understanding these differences is crucial for accurate diagnosis and appropriate treatment.
Osteoporosis is a chronic skeletal disorder characterized by a progressive reduction in bone mineral density (BMD) and deterioration of bone microarchitecture. This leads to increased bone fragility and a higher risk of fractures, particularly in the hip, spine, and wrist. Often called the “silent disease,” osteoporosis typically progresses without symptoms and is usually diagnosed only after a fracture occurs. The primary diagnostic approach involves a dual-energy X-ray absorptiometry (DXA) scan, which measures BMD and generates a T-score. A T-score of –2.5 or lower compared to the young adult mean confirms osteoporosis. Screening can be initiated using the FRAX® tool, which estimates fracture risk based on clinical factors such as age, gender, prior fractures, and steroid use. Osteoporosis is most prevalent among postmenopausal women and older adults, with complications including chronic pain, deformity, loss of independence, and increased mortality after fractures.
Sarcopenia, on the other hand, is a progressive condition affecting the skeletal muscular system, marked by the gradual loss of muscle mass, strength, and functional capacity. Unlike osteoporosis, sarcopenia’s progression is often noticeable, manifesting as weakness, slower walking speed, difficulty climbing stairs, and reduced mobility over time. Diagnosis requires a multi-component assessment evaluating muscle mass, muscle strength, and physical performance. Key diagnostic tools include DXA for measuring muscle mass, handgrip strength tests, gait speed assessment, and chair stand tests. The SARC-F questionnaire is commonly used for initial screening to identify individuals at risk. According to the EWGSOP2 criteria, sarcopenia is confirmed when both low muscle strength and low muscle mass and/or performance are present. Major complications include increased fall risk, mobility limitations, physical disability, frailty, and loss of independence, emphasizing the importance of early detection and targeted resistance training interventions.
The Dangerous Connection: When Both Conditions Coexist
Osteosarcopenia, the coexistence of osteopenia/osteoporosis and sarcopenia, has emerged as a critical clinical entity with substantially greater adverse effects on skeletal integrity than either condition alone. Despite its clinical significance, this dual diagnosis lacks a universally accepted definition, creating substantial challenges for healthcare practitioners and researchers.
A comprehensive systematic review encompassing over 64,000 individuals revealed that osteosarcopenia affects approximately 18% of older adults globally, with devastating consequences: a 54% increased risk of falls, doubled fracture risk, and 75% higher mortality rates. However, the prevalence and predictive value of osteosarcopenia vary considerably depending on the diagnostic criteria employed—a reflection of the broader heterogeneity plaguing current definitions.
This inconsistency complicates epidemiological data interpretation and hinders clinical translation. Experts emphasize the urgent need for a standardized, consensus-based definition, potentially termed "osteodynapenia," that incorporates both muscle strength assessments and bone mineral density measurements. Without prospective validation as an independent fracture risk factor, osteosarcopenia risks remaining a theoretical construct rather than evolving into a practical clinical tool. Establishing standardized diagnostic criteria is essential to enable early identification, targeted interventions, and improved outcomes for the growing population of older adults facing this dual skeletal threat.
Geographic Variations in Risk:
European populations: 4.37 times higher osteoporosis risk with sarcopenia
Asian populations: 2.66 times higher risk
American populations: 2.32 times higher risk
Gender differences: Males with sarcopenia show 4.74 times higher osteoporosis risk compared to 3.46 times in females
Shared Risk Factors
Both conditions share common underlying mechanisms:
Hormonal Changes: Declining estrogen and testosterone levels affect both bone density and muscle mass
Chronic Inflammation: Inflammatory cytokines like IL-6 and TNF-α contribute to both bone loss and muscle degradation
Physical Inactivity: Sedentary lifestyle reduces mechanical loading on bones and muscle stimulation
Nutritional Deficiencies: Inadequate calcium, vitamin D, and protein intake affects both systems
Aging: The primary non-modifiable risk factor for both conditions
The Vicious Cycle
When osteoporosis and sarcopenia coexist, they create a destructive feedback loop:
Muscle loss reduces mechanical loading on bones, accelerating bone density loss
Weakened bones increase fracture risk
Fractures lead to immobilization and reduced physical activity
Inactivity causes further muscle loss
The cycle continues, compounding functional decline
Diagnosis: How Each Condition Is Identified
Diagnosing Osteoporosis
Primary Method: Dual-energy X-ray absorptiometry (DXA) scan generates a T-score comparing your BMD to healthy young adults
Assessment Includes:
Medical history review
Physical examination for height loss or spinal curvature
BMD measurement at the hip, spine, or forearm
Laboratory tests (calcium, vitamin D, parathyroid hormone)
FRAX® tool for fracture risk prediction
Diagnosing Sarcopenia
Comprehensive Assessment includes multiple components:
Screening: SARC-F questionnaire to identify at-risk individuals
Muscle Mass Measurement:
DXA for appendicular lean mass
BIA (bioelectrical impedance analysis)
MRI or CT for detailed assessment
Muscle Strength Testing:
Grip strength measurement
Chair stand test
Physical Performance Evaluation:
Gait speed test
Timed up-and-go (TUG) test
6-minute walk test
Short physical performance battery (SPPB)
Treatment and Management: Distinct Yet Complementary Approaches
Managing Osteoporosis
Pharmacological Interventions:
Bisphosphonates (prevent bone breakdown)
Selective estrogen receptor modulators (SERMs)
Denosumab (reduces bone resorption)
Teriparatide (promotes bone formation)
Lifestyle Modifications:
Weight-bearing exercises (walking, jogging, dancing)
Calcium supplementation (1,000-1,200 mg daily)
Vitamin D supplementation (800-1,000 IU daily)
Smoking cessation
Moderate alcohol consumption
Managing Sarcopenia
Primary Interventions:
Resistance Training: Progressive strength training is the cornerstone of sarcopenia management. Exercises with weights or resistance bands promote muscle protein synthesis and enhance strength.
Nutritional Optimization:
Adequate protein intake (1.0-1.2 g/kg body weight daily)
High-quality protein sources distributed throughout the day
Vitamin D supplementation for muscle function
Multidisciplinary Approach: Collaboration among physicians, physical therapists, and dietitians optimizes treatment outcomes.
Integrated Management Strategy
Since these conditions often coexist, an integrated approach addresses both simultaneously:
Exercise Programs: Combine resistance training (for muscle) with weight-bearing activities (for bone)
Comprehensive Nutrition: Ensure adequate calcium, vitamin D, and protein intake
Fall Prevention: Environmental modifications, balance training, vision assessment, and medication review
Regular Monitoring: Track both bone density and muscle function over time
Prevention: Your Action Plan for Healthy Aging
Start Early, Stay Consistent
The best time to prevent osteoporosis and sarcopenia is before they develop. Here's your comprehensive prevention strategy:
Physical Activity:
Engage in regular weight-bearing exercise (30 minutes, most days)
Include resistance training 2-3 times weekly
Practice balance exercises like tai chi or yoga
Nutrition:
Consume calcium-rich foods (dairy, leafy greens, fortified products)
Ensure adequate vitamin D through sunlight and diet
Eat protein with every meal (lean meats, fish, legumes, dairy)
Maintain a balanced, nutrient-dense diet
Lifestyle Factors:
Avoid smoking
Limit alcohol consumption
Maintain healthy body weight
Get regular health screenings
Fall Prevention:
Remove home hazards (loose rugs, clutter)
Install adequate lighting
Use assistive devices if needed
Have regular vision checks
The Impact on Quality of Life
Both osteoporosis and sarcopenia significantly affect health and well-being, but in different ways:
Osteoporosis Consequences:
Severe pain from fractures
Loss of height and spinal deformity
Disability and functional limitations
Increased dependency on others
Higher risk of subsequent fractures
Increased mortality (especially after hip fractures)
Sarcopenia Consequences:
Difficulty performing daily activities
Reduced mobility and independence
Increased vulnerability to falls
Development of frailty
Higher hospitalization rates
Decreased quality of life
Combined Impact: When both conditions coexist, the effects multiply. The combination creates greater functional limitations, higher fall and fracture risk, and accelerated decline in independence.
Who's at Highest Risk?
Osteoporosis Risk Factors
Non-Modifiable:
Age (especially over 50)
Female gender
Family history
Menopause
Ethnicity (higher in Caucasian and Asian populations)
Modifiable:
Low calcium and vitamin D intake
Sedentary lifestyle
Smoking
Excessive alcohol use
Long-term corticosteroid use
Low body weight
Sarcopenia Risk Factors
Primary Risk Factors:
Advanced age (especially over 60)
Physical inactivity
Inadequate protein intake
Chronic diseases (diabetes, cardiovascular disease)
Certain medications (glucocorticoids)
Hormonal imbalances
Population Variations: Community-dwelling individuals show higher susceptibility to combined osteoporosis-sarcopenia (3.70 times higher risk) compared to inpatient and outpatient populations.
Future Directions: Hope on the Horizon
Research continues to advance our understanding and treatment of both conditions:
Diagnostic Innovations:
High-resolution imaging for detailed bone microarchitecture assessment
Advanced MRI techniques for muscle quality evaluation
Biomarker development for early detection
Emerging Therapies:
Targeted bone-forming and muscle-building agents
Regenerative medicine approaches (stem cell therapy)
Precision interventions based on genetic profiling
Personalized Medicine: Future treatments will be tailored to individual risk profiles, genetic characteristics, and specific needs.
Frequently Asked Questions (FAQs)
1. Can you have both sarcopenia and osteoporosis at the same time?
Yes. Many older adults experience both conditions simultaneously—a condition sometimes referred to as osteosarcopenia. The combination greatly increases fall and fracture risk and requires integrated treatment.
2. What are the early warning signs of sarcopenia?
Early symptoms include loss of muscle strength, slower walking speed, difficulty climbing stairs, or problems rising from a chair. These are subtle but important indicators of declining muscle function.
3. Is osteoporosis painful before a fracture occurs?
No. Osteoporosis is known as a “silent disease” because it causes no pain or symptoms until a bone breaks. Regular bone density screening (DXA scan) after age 50 is crucial for early detection.
4. What type of exercise helps prevent both conditions?
A combination of resistance training (for muscle) and weight-bearing activities like walking, stair climbing, or dancing (for bone) is most effective. Add balance training such as tai chi to reduce fall risk.
5. How much protein and vitamin D do older adults need?
Most experts recommend 1.0–1.2 g of protein per kg of body weight daily and 800–1,000 IU of vitamin D per day to support both muscle and bone health. Blood levels should be monitored by your healthcare provider.
6. Are these conditions reversible?
While complete reversal may not always be possible, both conditions are highly manageable. Regular exercise, optimal nutrition, and medical therapies can significantly restore function and prevent complications.
7. Who should get screened for sarcopenia and osteoporosis?
Adults over 50—especially postmenopausal women, men with low testosterone, or anyone with chronic disease, frailty, or a history of fractures—should discuss screening with their doctor.
Key Takeaways:
Osteoporosis weakens bones; sarcopenia weakens muscles—both increase fall and fracture risk
Having one condition significantly increases your risk for developing the other
Prevention is possible through exercise, proper nutrition, and healthy lifestyle choices
Early detection and intervention are crucial for maintaining independence and quality of life
Integrated care approaches that address both conditions simultaneously yield the best outcomes
Don't wait for symptoms to appear—osteoporosis is silent until fracture occurs, and sarcopenia develops gradually. Talk to your healthcare provider about screening, especially if you're over 50 or have risk factors. With proper assessment, prevention strategies, and treatment when needed, you can maintain strong bones and muscles well into your later years.
Take action today: Schedule a bone density test, assess your protein intake, start resistance training, and ensure you're getting adequate calcium and vitamin D. Your future self will thank you for the investment in musculoskeletal health you make now.
This information is for educational purposes only and should not replace professional medical advice. Always consult with your healthcare provider for personalized recommendations based on your individual health status and risk factors.
Related Articles
Sarcopenia: The Complete Guide to Age-Related Muscle Loss and How to Fight It | DR T S DIDWAL
Citations
Jin, S., Zheng, F., Liu, H., Liu, L., & Yu, J. (2025). The correlation between sarcopenia and osteoporosis in the elderly: a systematic review and meta-analysis. Frontiers in Medicine, 12, 1603879. https://doi.org/10.3389/fmed.2025.1603879
Cacciatore, S., Prokopidis, K. & Schlögl, M. Osteoporosis and sarcopenia: two sides of the same coin. Eur Geriatr Med 16, 1749–1752 (2025). https://doi.org/10.1007/s41999-025-01275-z
Chen, S., Xu, X., Gong, H., Chen, R., Guan, L., Yan, X., Zhou, L., Yang, Y., Wang, J., Zhou, J., Zou, C., & Huang, P. (2024). Global epidemiological features and impact of osteosarcopenia: A comprehensive meta-analysis and systematic review. Journal of cachexia, sarcopenia and muscle, 15(1), 8–20. https://doi.org/10.1002/jcsm.13392
Das, C., Das, P. P., & Kambhampati, S. B. S. (2023). Sarcopenia and Osteoporosis. Indian journal of orthopaedics, 57(Suppl 1), 33–41. https://doi.org/10.1007/s43465-023-01022-1
Cruz-Jentoft, A. J., Bahat, G., Bauer, J., Boirie, Y., Bruyère, O., Cederholm, T., Cooper, C., Landi, F., Rolland, Y., Sayer, A. A., Schneider, S. M., Sieber, C. C., Topinkova, E., Vandewoude, M., Visser, M., Zamboni, M., & Writing Group for the European Working Group on Sarcopenia in Older People 2 (EWGSOP2), and the Extended Group for EWGSOP2 (2019). Sarcopenia: revised European consensus on definition and diagnosis. Age and ageing, 48(1), 16–31. https://doi.org/10.1093/ageing/afy169