Why Obesity is a Disease, Not a Lifestyle Choice: Latest Evidence-Based Insights
A comprehensive breakdown of obesity research, exploring genetic, environmental, and physiological drivers of weight and evidence-based treatment options
OBESITY
Dr. T.S. Didwal, M.D.(Internal Medicine)
1/6/202611 min read
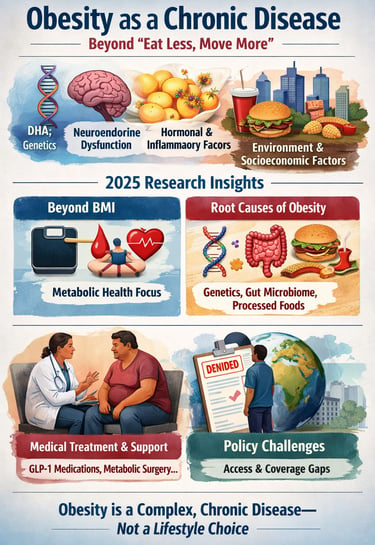
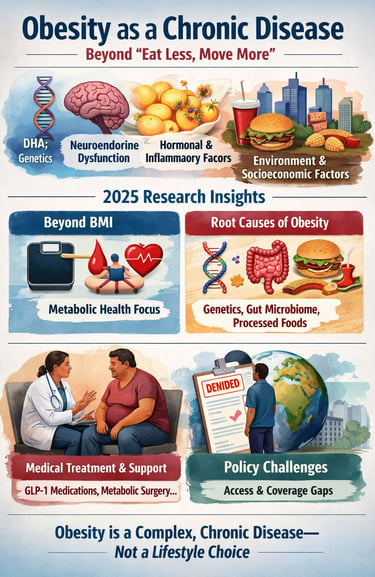
For decades, obesity has been framed as a failure of willpower—summed up by the dismissive advice to “eat less and move more.” Yet mounting scientific evidence makes it clear that this narrative is not only inaccurate but harmful. Obesity is now firmly established as a chronic, relapsing disease, driven by complex interactions between genetics, neuroendocrine regulation, adipose tissue biology, and the modern food and social environment (Shah et al., 2025; Blüher, 2025).
Research published in 2025 has fundamentally reshaped how obesity is understood and treated. Excess adipose tissue functions as an active endocrine organ, altering inflammatory pathways, insulin sensitivity, and cardiovascular risk, while adaptive responses in the brain defend body weight against loss, making long-term weight reduction biologically difficult (Shah et al., 2025). At the same time, reliance on body mass index (BMI) alone has proven inadequate, as individuals with similar BMIs can have vastly different metabolic risks and health outcomes (Cohen et al., 2025).
Importantly, contemporary research also highlights that obesity arises from multifactorial root causes—including genetic susceptibility, epigenetic influences, gut microbiome alterations, and powerful environmental drivers such as ultra-processed foods and socioeconomic stressors (Falahee et al., 2025). Despite this scientific clarity, global health policy and insurance coverage continue to lag behind, limiting access to evidence-based treatments and perpetuating stigma (Chandiwana et al., 2025).
Understanding obesity through a disease-based, compassionate, and evidence-driven lens is no longer optional—it is essential for improving cardiometabolic outcomes and restoring dignity to care.
Clinical pearls
1. Your Fat is an Active "Command Center"
Think of body fat not as a storage closet for extra calories, but as a massive endocrine gland, similar to your thyroid. It constantly pumps out hormones and inflammatory signals. In the disease state of obesity, these signals can become "noisy," leading to insulin resistance and heart strain. Treatment isn't just about shrinking the closet; it’s about calming the chemical signals.
2. The "Thermostat" is Set Too High
The brain (specifically the hypothalamus) acts like a metabolic thermostat. In chronic obesity, this thermostat gets "stuck" at a higher set point. When you lose weight through willpower alone, the brain senses a crisis and triggers metabolic adaptation—slowing your heart rate and increasing hunger hormones to "defend" the higher weight. Modern medications (like GLP-1s) work by helping to reset that internal thermostat.
3. BMI is a Map, Not the Territory
Body Mass Index (BMI) is a crude tool because it cannot distinguish between "marbled" fat inside organs (visceral fat) and healthy muscle. You can have a "normal" BMI but be metabolically at risk, or a higher BMI with excellent heart health. Clinical success in 2025 is measured by metabolic phenotyping: looking at blood sugar, liver health, and physical function rather than just the number on the scale.
4. The "Second Brain" in Your Gut
Your gut microbiome—the trillions of bacteria living in your digestive tract—acts as a metabolic partner. These bacteria help determine how many calories you harvest from food and influence the signals of fullness sent to your brain. Research now shows that shifting the gut environment through fiber and specific treatments can be just as important as the calorie count itself.
5. Movement is Medicine (Even Without Weight Loss)
While exercise is often sold as a weight-loss tool, its greatest clinical value in obesity is cardiometabolic protection. Even if the scale doesn't move a single pound, regular physical activity improves insulin sensitivity and reduces the "sticky" cholesterol that leads to heart disease. In the 2025 framework, we view exercise as a way to "immunize" the heart against the complications of obesity.
Understanding Obesity: More Than Just Numbers on a Scale
What Makes Obesity a Chronic Disease?
The medical community's recognition of obesity as a chronic disease represents a paradigm shift in healthcare. Unlike acute conditions that resolve with short-term treatment, chronic diseases like obesity require ongoing management, similar to diabetes, hypertension, or heart disease.
According to Shah et al. (2025), obesity should be understood as a disease with distinct clinical features and physiological mechanisms rather than a cosmetic concern or personal failing. Their research published in the Methodist DeBakey Cardiovascular Journal emphasizes that obesity involves complex interactions between genetic factors, metabolic processes, hormonal regulation, and environmental influences (Shah et al., 2025).
Key physiological insights include:
Adipose tissue dysfunction: Fat tissue isn't just storage—it's an active endocrine organ that secretes hormones and inflammatory molecules affecting insulin resistance, cardiovascular health, and immune function
Hypothalamic regulation: The brain's control centers for hunger and satiety become dysregulated in obesity, making weight loss maintenance extraordinarily challenging
Metabolic adaptation: The body actively defends against weight loss through hormonal changes that increase hunger and decrease energy expenditure
The Root Causes: A Multifactorial Disease
Falahee et al. (2025) conducted comprehensive research examining why we must acknowledge the root causes of obesity rather than focusing solely on individual behaviors. Published in Med, their study identifies multiple interconnected factors driving the obesity epidemic (Falahee et al., 2025).
Biological root causes include:
Genetic predisposition: Hundreds of genes influence body weight regulation, with some individuals having 40-70% higher genetic risk for obesity
Epigenetic changes: Environmental factors can modify gene expression across generations, potentially explaining rapid increases in obesity rates
Gut microbiome alterations: The trillions of bacteria in our digestive system influence metabolism, inflammation, and weight regulation
Environmental and social determinants encompass:
Food environment: The prevalence of ultra-processed foods, food deserts, and aggressive marketing of calorie-dense products
Built environment: Urban design that discourages physical activity and promotes sedentary lifestyles
Socioeconomic factors: Income inequality, stress, inadequate sleep, and limited access to healthcare resources
Cultural influences: Social norms around eating, body image, and the stigmatization of people with obesity
The researchers emphasize that recognizing these upstream factors is essential for developing effective public health interventions and reducing weight bias in healthcare settings (Falahee et al., 2025).
Beyond BMI: A New Framework for Obesity Treatment
Why Body Mass Index Isn't Enough
Cohen et al. (2025) challenge the over-reliance on Body Mass Index (BMI) as the primary metric for obesity diagnosis and treatment decisions. Their framework, published in The British Journal of Surgery, argues that "obesity is more than a number" and advocates for a comprehensive approach to patient assessment (Cohen et al., 2025).
Limitations of BMI include:
Fails to distinguish between muscle mass and fat mass
Doesn't account for fat distribution patterns (visceral versus subcutaneous fat)
Ignores individual variations in metabolic health and comorbidities
May misclassify metabolically healthy individuals or miss metabolically unhealthy normal-weight people
The comprehensive treatment framework proposed by Cohen et al. (2025) includes:
Metabolic phenotyping: Assessing insulin sensitivity, glucose metabolism, lipid profiles, and inflammatory markers beyond simple weight measurements
Functional assessment: Evaluating how obesity impacts quality of life, physical function, and mental health
Comorbidity evaluation: Identifying obesity-related conditions like type 2 diabetes, cardiovascular disease, sleep apnea, fatty liver disease, and certain cancers
Personalized treatment selection: Matching interventions to individual patient profiles rather than applying one-size-fits-all approaches
This patient-centered approach recognizes that two individuals with identical BMIs may have vastly different health risks and treatment needs (Cohen et al., 2025).
Cardiometabolic Health: The Heart of the Matter
Prioritizing Cardiovascular and Metabolic Outcomes
Singh et al. (2025) provide a comprehensive narrative review examining obesity through the lens of cardiometabolic health. Published in Advances in Therapy, their research emphasizes why cardiovascular risk reduction should be a primary focus of obesity management (Singh et al., 2025).
Cardiometabolic complications of obesity include:
Coronary artery disease: Obesity increases heart attack risk through multiple mechanisms including inflammation, abnormal cholesterol levels, and hypertension
Heart failure: Excess weight places mechanical strain on the heart while metabolic dysfunction impairs cardiac function
Atrial fibrillation: Obesity significantly increases risk of irregular heart rhythms
Metabolic syndrome: A cluster of conditions including elevated blood pressure, blood sugar, abnormal cholesterol, and abdominal obesity that dramatically increase cardiovascular risk
Evolving management strategies highlighted by Singh et al. (2025) include:
Pharmacological interventions: New classes of anti-obesity medications like GLP-1 receptor agonists that not only promote weight loss but also provide cardiovascular protection
Bariatric surgery: Metabolic surgery procedures that can dramatically improve or resolve type 2 diabetes and reduce long-term cardiovascular mortality
Lifestyle medicine: Evidence-based approaches to nutrition, physical activity, stress management, and sleep optimization
Combination therapy: Integrating multiple treatment modalities for synergistic effects
The researchers emphasize that cardiometabolic prioritization means focusing on health improvements beyond weight loss alone, recognizing that even modest weight reduction can produce significant metabolic benefits (Singh et al., 2025).
The Evolution of Obesity Definitions and Understanding
From Lifestyle Issue to Medical Condition
Blüher (2025) provides historical context on how obesity research has evolved, published in Nature Reviews Endocrinology. This perspective piece traces the scientific community's journey from viewing obesity as a simple energy balance problem to understanding it as a complex neuroendocrine disease (Blüher, 2025).
Historical milestones in obesity research:
1940s-1960s: Focus on caloric intake and willpower
1970s-1980s: Recognition of genetic components through twin and adoption studies
1990s-2000s: Discovery of leptin and other adipokines revealing fat tissue as an endocrine organ
2010s: Understanding of gut hormones, brain circuits regulating appetite, and metabolic adaptation
2020s: Integration of precision medicine, new pharmacological treatments, and recognition as a chronic disease requiring long-term management
Future directions identified by Blüher (2025) include:
Personalized medicine: Using genetic testing, metabolomics, and other biomarkers to tailor treatments
Novel therapeutics: Development of drugs targeting specific pathways in appetite regulation, energy expenditure, and fat metabolism
Prevention strategies: Early-life interventions addressing childhood obesity and intergenerational effects
Technology integration: Digital health tools, continuous glucose monitoring, and AI-driven treatment optimization
This historical perspective demonstrates that our understanding of obesity continues to deepen, moving away from stigmatizing narratives toward compassionate, science-based medical care (Blüher, 2025).
Global Health Policy: Closing the Recognition Gap
Why Policy Must Catch Up to Science
Perhaps the most urgent message comes from Chandiwana et al. (2025), who argue in The Lancet Global Health that while science has established obesity as a disease, global health policy has failed to keep pace (Chandiwana et al., 2025).
Current policy gaps include:
Healthcare coverage: Many insurance systems don't cover evidence-based obesity treatments including medications or surgery
Prevention funding: Insufficient investment in public health programs addressing obesogenic environments
Regulatory frameworks: Weak policies on food marketing, nutrition labeling, and urban planning
Stigma and discrimination: Lack of legal protections for people with obesity in employment, healthcare, and education
Recommended policy actions by Chandiwana et al. (2025):
Recognize obesity as a disease in legal and regulatory frameworks across all nations
Ensure universal healthcare coverage for comprehensive obesity treatment including lifestyle interventions, pharmacotherapy, and surgical options
Implement prevention policies such as sugar taxes, marketing restrictions on unhealthy foods to children, and incentives for healthy food production
Address social determinants through urban planning that promotes physical activity, food security programs, and education initiatives
Combat weight stigma through anti-discrimination legislation and public awareness campaigns
Increase research funding for obesity prevention, treatment, and understanding health disparities
The authors emphasize that recognizing obesity as a disease isn't just semantics—it's essential for mobilizing resources, reducing stigma, and ensuring people receive the medical care they need (Chandiwana et al., 2025).
Practical Implications: What This Means for Patients and Providers
For Healthcare Professionals
These 2025 studies collectively provide clear guidance for clinical practice:
Adopt comprehensive assessment: Move beyond BMI to evaluate metabolic health markers, comorbidities, functional status, and psychosocial factors. Use tools that capture the full picture of each patient's health.
Embrace evidence-based treatments: Stay current on emerging pharmacological options, surgical techniques, and lifestyle intervention strategies. Recognize that intensive behavioral therapy, medication, and surgery are all legitimate medical treatments.
Address root causes: Consider social determinants of health in treatment planning. Connect patients with resources addressing food insecurity, safe spaces for physical activity, and mental health support.
Practice compassionate care: Use non-stigmatizing language, recognize obesity as a disease rather than a personal failing, and validate patients' experiences with weight loss challenges.
Take a long-term approach: Frame obesity management as ongoing chronic disease care requiring sustained support, similar to managing hypertension or diabetes.
For Patients and Families
Understand it's not your fault: Obesity results from complex biological, environmental, and social factors largely beyond individual control. Self-blame and weight stigma are harmful and counterproductive.
Focus on health, not just weight: Improvements in blood pressure, blood sugar, cholesterol, fitness, sleep quality, and mental wellbeing are valuable outcomes regardless of scale changes.
Seek comprehensive medical care: You deserve access to the full range of evidence-based treatments. Don't settle for providers who offer only generic advice to "eat less and exercise more."
Advocate for yourself: Request referrals to obesity medicine specialists, inquire about anti-obesity medications, and ask about insurance coverage for treatments.
Address contributing factors: Work with healthcare teams to identify and address sleep disorders, stress, medications that promote weight gain, and other factors affecting weight.
Build support systems: Connect with communities that provide non-judgmental support and share experiences navigating obesity management.
Frequently Asked Questions
Is obesity really a disease or just being overweight?
Yes, obesity is recognized as a chronic disease by major medical organizations worldwide. Research from 2025 demonstrates it involves specific physiological dysfunction including altered hormone regulation, metabolic abnormalities, and inflammatory processes—not simply excess weight. Like other chronic diseases, it requires ongoing medical management (Shah et al., 2025).
If obesity is a disease, does that mean I'm not responsible for my health?
Recognizing obesity as a disease doesn't remove personal agency—it acknowledges biological realities that make weight management extraordinarily difficult. You're responsible for working with healthcare providers, following treatment plans, and making health-supporting choices within your circumstances. However, the disease framework means you deserve medical treatment and support rather than judgment.
What's wrong with using BMI to diagnose obesity?
BMI is a screening tool but has significant limitations. It doesn't distinguish muscle from fat, ignores fat distribution patterns, and doesn't capture metabolic health status. Research shows two people with identical BMIs can have vastly different health risks. Comprehensive assessment should include metabolic markers, body composition, comorbidities, and functional status (Cohen et al., 2025).
Are weight loss medications really safe and effective?
Newer anti-obesity medications, particularly GLP-1 receptor agonists, have demonstrated both significant weight loss and cardiovascular benefits in clinical trials. Like all medications, they have potential side effects and aren't appropriate for everyone. They work best when combined with lifestyle modifications and require ongoing use, as obesity is a chronic condition (Singh et al., 2025).
Why isn't obesity treatment covered by my insurance?
Despite scientific evidence establishing obesity as a disease, many insurance systems haven't updated policies accordingly. This represents the policy gap identified by researchers—science has advanced but healthcare coverage hasn't kept pace. Advocacy is needed to change these policies and ensure access to evidence-based treatments (Chandiwana et al., 2025).
Can you be healthy at any size?
Health exists on a continuum and isn't determined by weight alone. Some individuals with higher body weights have excellent metabolic health, while some thin people have metabolic dysfunction. However, research shows obesity increases risk for certain conditions like type 2 diabetes and cardiovascular disease. The focus should be on overall health improvements rather than weight as the sole measure of wellness.
What are the most effective treatments for obesity?
Evidence-based treatments include intensive behavioral therapy (structured programs providing ongoing support), pharmacotherapy (anti-obesity medications), and metabolic surgery (bariatric procedures). Research shows combination approaches are often most effective. The best treatment varies by individual based on metabolic profile, comorbidities, preferences, and treatment history (Cohen et al., 2025; Singh et al., 2025).
How do I find a doctor who understands obesity as a disease?
Look for board-certified obesity medicine specialists or endocrinologists with obesity training. Ask potential providers about their approach—do they offer comprehensive assessment beyond BMI? Do they discuss medication and surgical options? Do they use non-stigmatizing language? Organizations like the Obesity Medicine Association can help locate qualified providers.
Author’s Note
Obesity remains one of the most misunderstood and stigmatized medical conditions worldwide. As a physician, I have witnessed firsthand the physical, emotional, and social burden carried by individuals living with obesity—often compounded by oversimplified advice and delayed access to evidence-based care. This article was written to bridge the gap between rapidly advancing scientific knowledge and everyday clinical practice.
The research highlighted here reflects a growing consensus in modern medicine: obesity is a chronic, biologically driven disease influenced by genetics, neuroendocrine regulation, environment, and social determinants of health. Recognizing obesity as a disease is not about removing personal responsibility, but about replacing blame with understanding, stigma with science, and resignation with effective treatment options.
My goal is to empower patients with knowledge, equip clinicians with updated evidence, and encourage policymakers to align health systems with contemporary obesity science. Compassionate, comprehensive care—rooted in evidence rather than judgment—is essential if we are to improve cardiometabolic outcomes and restore dignity to obesity management.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Individual circumstances vary, and treatment decisions should always be made in consultation with qualified healthcare professionals.
Related Articles
Why Your Body Resists Weight Loss: Understanding the Science of Weight Regain | DR T S DIDWAL
The BMI Paradox: Why "Normal Weight" People Still Get High Blood Pressure | DR T S DIDWAL
Breakthrough Research: Leptin Reduction is Required for Sustained Weight Loss | DR T S DIDWAL
The Metabolic Triad: Why Diabetes, Obesity & CVD Are One Epidemic | DR T S DIDWAL
Obesity 2025: Revolutionary Research Advances in Treatment and Management | DR T S DIDWAL
References
Blüher, M. (2025). The past and future of obesity research. Nature Reviews Endocrinology, 21, 666–667. https://doi.org/10.1038/s41574-025-01172-2
Chandiwana, N., Barquera, S., Baur, L., Buse, K., Halford, J., Halpern, B., Jackson-Morris, A., Mbanya, J. C., Nece, P., & Ralston, J. (2025). Obesity is a disease: Global health policy must catch up. The Lancet Global Health, 13(10), e1659–e1660. https://doi.org/10.1016/S2214-109X(25)00275-X
Cohen, R. V., Prager, G., & Salminen, P. (2025). Obesity is more than a number: A framework for treatment. BJS, 112(5), znaf100. https://doi.org/10.1093/bjs/znaf100
Falahee, B. E., Kim, D. W., & Apovian, C. M. (2025). Recognizing overweight and obesity as chronic diseases and acknowledging root causes. Med, 6(9), 100782. https://doi.org/10.1016/j.medj.2025.100782
Shah, A., Davarci, O., Chaftari, P., & Avenatti, E. (2025). Obesity as a disease: A primer on clinical and physiological insights. Methodist DeBakey Cardiovascular Journal, 21(2), 4–13. https://doi.org/10.14797/mdcvj.1515
Singh, V., Sun, J., Cheng, S., Kwan, A. C., & Velazquez, A. (2025). Obesity as a chronic disease: A narrative review of evolving definitions, management strategies, and cardiometabolic prioritization. Advances in Therapy, 42(11), 5341–5364. https://doi.org/10.1007/s12325-025-03352-y