The Cardiometabolic Connection: Why Metabolism Is Now Central to Heart Disease and Diabetes
Latest cardiometabolic research reveals how heart disease, diabetes, obesity, and metabolism are linked. Understand risk factors, insulin resistance, inflammation, and new treatment strategies.
METABOLISMHEART
Dr. T.S. Didwal, M.D.(Internal Medicine)
1/18/202611 min read
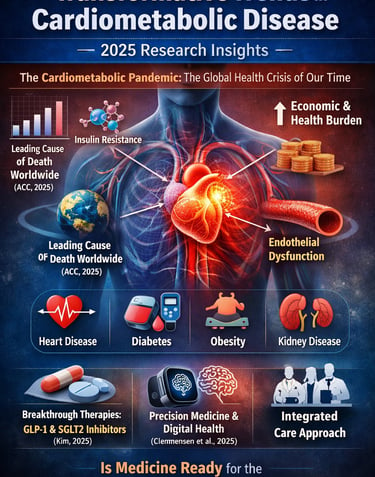
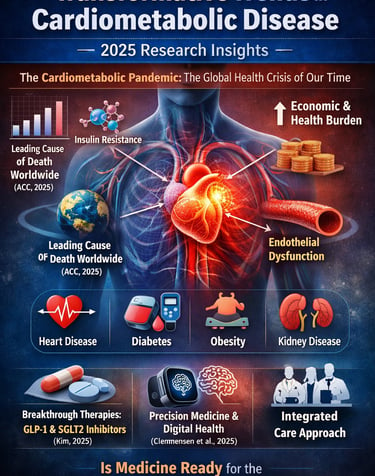
Cardiometabolic disease is no longer a silent threat—it is the defining health crisis of the 21st century. As we enter 2025, researchers warn that the convergence of cardiovascular disease, diabetes, obesity, and metabolic dysfunction has created a global “cardiometabolic pandemic,” one that now surpasses all other causes of mortality worldwide (American College of Cardiology, 2025). What was once viewed as a cluster of separate conditions is now understood as a unified, interconnected pathology driven by insulin resistance, chronic inflammation, and endothelial dysfunction—three mechanisms that amplify one another and dramatically accelerate disease progression (Eroglu et al., 2024).
New evidence reveals that patients with even mild metabolic disturbance—such as insulin resistance or visceral adiposity—face significantly higher risks for heart failure, myocardial infarction, stroke, and chronic kidney disease, even before diabetes is diagnosed (Kim, 2025). This shift in understanding demands a revolution in prevention, diagnosis, and treatment.
Meanwhile, transformative advances in therapeutics, digital health technology, and precision medicine offer unprecedented opportunities to intervene earlier and more effectively than ever before (Clemmensen et al., 2025). From GLP-1 receptor agonists to SGLT2 inhibitors, from AI-enhanced risk stratification to integrated care models, 2025 research paints a hopeful—but urgent—picture of the future of cardiometabolic medicine.
Clinical pearls
1. Think "Systems," Not Just "Organs"
Cardiometabolic syndrome is a unified pathophysiology where insulin resistance, vascular dysfunction, and inflammation form a feedback loop.
Your heart, kidneys, and metabolism are not separate silos—they are an interconnected network. A win for your blood sugar is almost always a win for your heart. Instead of focusing on a single lab number, focus on "Systemic Health," as modern medications (like GLP-1s and SGLT2s) are now designed to protect the entire network simultaneously.
2. Inflammation is the "Invisible Fire"
Chronic cytokine dysregulation and NLRP3 inflammasome activation are the primary drivers linking metabolic stress to arterial plaque rupture.
Think of chronic inflammation as a low-grade "smoldering fire" inside your blood vessels. Even if your cholesterol is normal, high inflammation can still put you at risk. You can "dampen the flames" through a Mediterranean-style diet and quality sleep, which act as natural anti-inflammatories for your vascular system.
3. The "Metabolic Flex" of Mitochondria
Mitochondrial dysfunction in cardiomyocytes (heart cells) reduces ATP production and increases oxidative stress, accelerating heart failure.
Your cells have tiny "power plants" called mitochondria. In cardiometabolic disease, these plants become inefficient. To keep them "flexible" and efficient, focus on Zone 2 exercise (steady, moderate-intensity movement where you can still hold a conversation). This specifically trains your cellular power plants to burn fuel more cleanly.
4. Precision Over Prediction
AI-driven risk stratification and real-time monitoring allow for "Dynamic Phenotyping"—adjusting treatment based on live data rather than static yearly labs.
A once-a-year blood test is just a snapshot; wearable technology provides the "movie" of your health. Use data from smartwatches or continuous monitors to see how your body specifically reacts to stress or a specific meal. This allows your doctor to move from "one size fits all" medicine to a "tailored-to-you" strategy.
5. Early Intervention is the Best "Rescue"
Preventative intervention during the early stages of metabolic dysfunction significantly halts the progression to advanced structural heart disease or renal failure.
It is much easier to maintain a healthy vessel than to repair a damaged one. The 2025 research shows that using newer "multitasking" medications earlier in the diagnosis (rather than waiting for traditional "failure") can change the entire trajectory of your health. Don't wait for a "cardiac event" to start a cardiac-protective regimen.
The Cardiometabolic Pandemic: Current Landscape
Cardiometabolic diseases now represent the leading cause of mortality globally, affecting millions across all demographics. Unlike traditional siloed approaches that treat cardiovascular disease and metabolic disorders separately, modern medicine recognizes these conditions as deeply intertwined pathological processes (Eroglu et al., 2024).
Recent research emphasizes that cardiometabolic syndrome isn't merely the coexistence of multiple conditions—it reflects a unified pathophysiological framework where insulin resistance, inflammatory cascades, and vascular dysfunction create a vicious cycle of deteriorating health.
Key Statistics on Cardiometabolic Disease
The burden of cardiometabolic disease continues to escalate. Contemporary epidemiology demonstrates that individuals with metabolic syndrome face significantly elevated risks for myocardial infarction, stroke, and heart failure progression. The economic impact extends beyond healthcare costs, affecting productivity, quality of life, and long-term mortality outcomes.
Breakthrough Research: What 2025 Reveals
1. Transformative Trends in CV Medicine (American College of Cardiology, 2025)
The American College of Cardiology's comprehensive analysis on transformative trends in cardiovascular medicine for 2025 identifies several paradigm-shifting developments reshaping clinical practice.
This landmark ACC publication synthesizes emerging evidence across multiple domains of cardiovascular innovation, highlighting how novel therapeutics and technological advances are revolutionizing patient outcomes. The research emphasizes the integration of precision medicine principles in managing cardiometabolic disorders (American College of Cardiology, 2025).
Key Takeaways:
Digital health integration and real-time monitoring technologies enable personalized risk stratification
Novel therapeutic classes demonstrate superior efficacy in reducing cardiovascular events while simultaneously improving metabolic parameters
Multi-disciplinary care models combining cardiology with endocrinology yield superior outcomes compared to traditional siloed approaches
Preventive medicine through early intervention in cardiometabolic syndrome stages significantly reduces progression to advanced disease
Clinical Implications: Healthcare systems implementing these transformative trends report improved medication adherence, better control of multiple risk factors, and reduced hospitalizations.
2. Expanding Novel Therapeutics Beyond Heart Failure and Diabetes (Kim, 2025)
Recent research challenges the traditional boundary between heart failure treatment and diabetes management, demonstrating that emerging drug classes originally developed for specific conditions possess unexpected benefits across the cardiometabolic continuum (Kim, 2025).
This groundbreaking work explores how novel therapeutics—particularly newer GLP-1 receptor agonists, SGLT2 inhibitors, and emerging cardioprotective agents—function beyond their primary indications. The analysis reveals that these medications simultaneously improve cardiovascular outcomes, metabolic parameters, and inflammatory markers.
Key Takeaways:
SGLT2 inhibitors and GLP-1 agonists demonstrate cardioprotective properties independent of glycemic control
Cardiometabolic syndrome patients benefit from multi-targeted approaches addressing insulin resistance, inflammation, and vascular dysfunction simultaneously
Novel therapeutics reduce progression to heart failure and dialysis-dependent renal disease
Economic models demonstrate the cost-effectiveness of early intervention with these agents compared to managing advanced complications
Clinical Significance: The expansion of novel therapeutics beyond traditional disease boundaries allows clinicians to select medications that address multiple pathways simultaneously, optimizing outcomes for complex cardiometabolic patients.
3. Shaping the Future of Cardiometabolic Innovation (Clemmensen et al., 2025)
A collaborative investigation in Nature Metabolism presents a forward-looking analysis of cardiometabolic innovation and identifies key opportunities for advancing the field (Clemmensen et al., 2025).
This research synthesizes current knowledge on cardiometabolic disease mechanisms while proposing a research agenda for the next decade. The authors emphasize that true innovation requires integration across multiple disciplines—from molecular biology to population health—creating synergistic advances in cardiometabolic management.
Key Takeaways:
Mechanistic understanding of how metabolic dysfunction drives cardiovascular disease at molecular and cellular levels continues to evolve
Personalized medicine approaches using genetic profiling, biomarker assessment, and lifestyle data enable targeted intervention strategies
Technological innovation—including wearable sensors, artificial intelligence-driven risk prediction, and telemedicine platforms—transforms cardiometabolic disease management
Cross-disciplinary collaboration between cardiologists, endocrinologists, nephrologists, and other specialists optimizes cardiometabolic outcomes
Research Implications: The study identifies that future cardiometabolic innovation depends on breaking down traditional specialty silos and adopting integrated care models that address the full complexity of these interconnected conditions.
4. The Evolving Landscape of Cardiometabolic Diseases (Eroglu, Capone, & Schiattarella, 2024)
A comprehensive review in EBioMedicine examines how our understanding of cardiometabolic disease mechanisms has evolved, particularly regarding the inflammatory and metabolic foundations of cardiovascular dysfunction (Eroglu et al., 2024).
This analysis explores the dynamic pathophysiological landscape of cardiometabolic diseases, emphasizing that traditional risk factor models inadequately capture disease complexity. The authors highlight how chronic inflammation, endothelial dysfunction, and metabolic remodeling interact to drive cardiovascular disease progression in cardiometabolic syndrome patients.
Key Takeaways:
Inflammatory pathways involving cytokine dysregulation and immune cell infiltration contribute significantly to both cardiovascular disease and metabolic disorders
Endothelial dysfunction serves as a critical intersection point where metabolic disturbances translate into vascular pathology
Mitochondrial dysfunction in cardiomyocytes and metabolic tissues contributes to disease progression
Understanding these mechanisms enables development of targeted therapeutics that address root causes rather than just symptoms
Clinical Relevance: Recognising cardiometabolic diseases as fundamentally inflammatory conditions justifies the aggressive management of inflammation through lifestyle modifications, pharmacotherapy, and emerging anti-inflammatory strategies.
5. Emerging Therapeutic Frontiers in Cardiometabolic and Inflammatory Diseases (Ren, Chen, & Wang, 2025)
Recent research in the British Journal of Pharmacology identifies emerging therapeutic frontiers in managing the inflammatory dimension of cardiometabolic disease (Ren et al., 2025).
This work catalogs novel pharmacological targets and emerging drug classes demonstrating promise in preclinical and early clinical studies. The emphasis centers on compounds that simultaneously suppress pathological inflammation while enhancing metabolic and cardiovascular function—addressing the fundamental pathophysiology of cardiometabolic syndrome.
Key Takeaways:
Emerging therapeutics targeting specific inflammatory pathways (such as IL-6, TNF-alpha, and NLRP3 inflammasome) show promise in reducing cardiovascular events
Novel compounds enhancing mitochondrial function and cellular energy metabolism improve both metabolic and cardiac performance
Combination strategies pairing traditional cardiometabolic medications with anti-inflammatory agents demonstrate synergistic benefits
Personalized medicine approaches identifying patients most likely to benefit from specific emerging therapeutics optimize treatment outcomes
Future Directions: The identification of these emerging therapeutic frontiers suggests that next-generation treatments will integrate anti-inflammatory mechanisms with metabolic optimization and cardiovascular protection.
6. Proposing a New Clinical Sub-Specialty: Cardiovascular-Endocrine-Metabolic Medicine (Theodorakis, Nikolaou, & Krentz, 2025)
A compelling perspective in Biomolecules makes the case for establishing Cardiovascular-Endocrine-Metabolic Medicine as a dedicated clinical sub-specialty, fundamentally reshaping how medical training and practice address the cardiometabolic pandemic (Theodorakis et al., 2025).
This visionary paper argues that traditional specialty boundaries—dividing care between cardiology, endocrinology, and nephrology—create fragmented, suboptimal approaches to cardiometabolic disease. The authors propose a unified sub-specialty integrating expertise across these domains, creating clinicians uniquely equipped to manage complex cardiometabolic syndrome patients.
Key Takeaways:
Unified training in Cardiovascular-Endocrine-Metabolic Medicine produces clinicians with comprehensive understanding of disease mechanisms and therapeutic options
Integrated care models addressing cardiovascular disease, diabetes, obesity, and chronic kidney disease simultaneously yield superior outcomes
Sub-specialty recognition facilitates appropriate reimbursement, incentivizing adoption of comprehensive cardiometabolic management approaches
Standardized curricula and board certification in this field would elevate care quality across healthcare systems
Clinical Practice Transformation: Establishing Cardiovascular-Endocrine-Metabolic Medicine as a recognized specialty represents a profound shift toward truly patient-centered care addressing the full complexity of cardiometabolic disease.
Critical Themes Across 2025 Research
1. Integration Over Fragmentation
Across all recent research contributions, a unifying theme emerges: cardiometabolic disease management requires integration rather than fragmentation. Whether through novel therapeutics that work across traditional disease boundaries, multi-disciplinary care models, or the proposed new sub-specialty, the evidence overwhelmingly supports coordinated approaches.
2. Inflammation as Central Pathology
Multiple studies identify chronic inflammation as a critical mechanism linking metabolic dysfunction to cardiovascular disease. This recognition justifies therapeutic strategies targeting inflammatory pathways, from GLP-1 agonists with anti-inflammatory properties to emerging targeted anti-inflammatory compounds.
3. Personalization and Precision
Rather than one-size-fits-all approaches, contemporary research emphasizes personalized medicine strategies utilizing biomarkers, genetic information, and individual risk profiles to guide therapeutic selection. This precision-based approach maximizes efficacy while minimizing unnecessary treatment.
4. Technology as Enabler
Digital health technologies, artificial intelligence, and real-time monitoring platforms emerge as crucial enablers of superior cardiometabolic outcomes. These tools facilitate early detection, personalised adjustments to therapy, and enhanced patient engagement.
Frequently Asked Questions on Cardiometabolic Disease and 2025 Research
Q1: What exactly is cardiometabolic syndrome, and how does it differ from simply having heart disease and diabetes?
A: Cardiometabolic syndrome represents a unified pathophysiological condition where cardiovascular dysfunction and metabolic disorders arise from common underlying mechanisms—primarily insulin resistance, chronic inflammation, and endothelial dysfunction. Unlike patients who happen to have both conditions independently, cardiometabolic syndrome patients experience accelerated disease progression due to these interconnected processes amplifying each other. The 2025 research demonstrates that addressing shared mechanisms simultaneously produces superior outcomes compared to managing conditions separately.
Q2: Which novel therapeutics show the most promise for cardiometabolic disease management?
A: Recent research highlights SGLT2 inhibitors and GLP-1 receptor agonists as particularly promising, offering benefits beyond their primary indications. These novel therapeutics simultaneously improve cardiovascular outcomes, metabolic parameters, and inflammatory markers. Emerging compounds targeting specific inflammatory pathways also show considerable promise, particularly when combined with traditional medications.
Q3: Should I ask my doctor about the new Cardiovascular-Endocrine-Metabolic Medicine sub-specialty?
A: The proposal for this new clinical sub-specialty represents a vision for future practice rather than currently available training everywhere. However, research supports seeking clinicians with expertise spanning cardiology, endocrinology, and metabolism. Some academic medical centers and progressive health systems already implement integrated care models approximating this approach. Advocating for coordinated, multi-disciplinary care is appropriate regardless of formal sub-specialty recognition.
Q4: How do the 2025 cardiometabolic research findings change what I should do about my health?
A: The research collectively emphasizes that early intervention in cardiometabolic disease stages dramatically improves long-term outcomes. This means: (1) aggressive management of all cardiometabolic risk factors rather than focusing narrowly on one condition, (2) consideration of newer novel therapeutics that address multiple pathways, and (3) adoption of comprehensive lifestyle modifications addressing nutrition, physical activity, sleep, and stress. Discuss these research-supported approaches with your healthcare providers.
Q5: What role do anti-inflammatory strategies play in modern cardiometabolic management?
A: Emerging evidence across multiple 2025 studies identifies chronic inflammation as central to cardiometabolic disease progression. Beyond anti-inflammatory medications, lifestyle approaches including Mediterranean or DASH diet patterns, regular aerobic exercise, stress management, and adequate sleep all provide meaningful anti-inflammatory benefits. Some novel therapeutics specifically enhance anti-inflammatory mechanisms, and future treatments will increasingly target inflammatory pathways.
Q6: How is artificial intelligence and digital health changing cardiometabolic disease management?
A: Recent analyses emphasize that digital health integration and AI-driven risk prediction enable personalized medicine at scale. Real-time monitoring through wearable devices allows continuous assessment of cardiovascular and metabolic parameters, triggering therapeutic adjustments before complications develop. Telemedicine platforms expand access to specialists and facilitate integrated care coordination previously limited to academic centers.
Q7: Why is understanding mitochondrial dysfunction important for cardiometabolic disease?
A: Multiple 2025 studies highlight that mitochondrial dysfunction contributes fundamentally to both metabolic disorders and cardiovascular disease. Mitochondria generate cellular energy, and their impaired function drives insulin resistance, reduces energy availability in heart muscle, and promotes inflammation. Emerging therapeutics targeting mitochondrial restoration represent exciting emerging therapeutic frontiers.
Author’s Note
As a physician and researcher who has spent decades studying metabolic disease, I have witnessed firsthand how profoundly cardiometabolic disorders shape the trajectory of human health. The convergence of heart disease, diabetes, obesity, and insulin resistance is not simply a medical overlap—it is a metabolic emergency that affects every organ, every system, and every stage of life. My goal in writing this article is to translate the latest 2024–2025 scientific insights into clear, clinically meaningful guidance that empowers both healthcare professionals and patients.
This work draws on extensive analysis of contemporary peer-reviewed literature, emerging therapeutic breakthroughs, and evolving consensus from global cardiometabolic research bodies. As with my ongoing books on Type 2 Diabetes, metabolism, and strength training science, my commitment is to present evidence-based, practical, and forward-looking information that bridges the gap between research and real-world application.
The future of cardiometabolic medicine is transforming rapidly. By understanding the mechanisms driving disease—and the innovative treatments now available—we can move toward a model of prevention and care that is proactive, personalized, and truly life-changing.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Individual circumstances vary, and treatment decisions should always be made in consultation with qualified healthcare professionals.
Related Articles
Your Body Fat Is an Endocrine Organ—And Its Hormones Shape Your Heart Health | DR T S DIDWAL
hsCRP Explained: What Inflammation Means for Your Heart | DR T S DIDWAL
What’s New in the 2025 Blood Pressure Guidelines? A Complete Scientific Breakdown | DR T S DIDWAL
Low-Fat vs. Low-Carb: Which Diet is Best for Weight Loss? | DR T S DIDWAL
5 Steps to Reverse Metabolic Syndrome: Diet, Habit, & Lifestyle Plan | DR T S DIDWAL
The Role of Cholesterol in Health and Disease: Beyond the "Bad" Label | DR T S DIDWAL
Lowering Cholesterol with Food: 4 Phases of Dietary Dyslipidemia Treatment | DR T S DIDWAL
The Best Dietary Fat Balance for Insulin Sensitivity, Inflammation, and Longevity | DR T S DIDWAL
References
American College of Cardiology. (2025, January 1). Cover story | Transformative trends in CV medicine for 2025. American College of Cardiology. https://www.acc.org/latest-in-cardiology/articles/2025/01/01/42/cover-story-transformative-trends-in-cv-medicine-for-2025
Clemmensen, C., Gerhart-Hines, Z., Schwartz, T. W., & et al. (2025). Shaping the future of cardiometabolic innovation: Advances and opportunities. Nature Metabolism, 7, 1495–1497. https://doi.org/10.1038/s42255-025-01343-5
Eroglu, T., Capone, F., & Schiattarella, G. G. (2024). The evolving landscape of cardiometabolic diseases. EBioMedicine, 109, 105447. https://doi.org/10.1016/j.ebiom.2024.105447
Kim, H. (2025). Expanding the role of novel therapeutics in cardiometabolic syndrome: Beyond heart failure and diabetes. CardioMetabolic Syndrome Journal, 5(1), 9. https://doi.org/10.51789/cmsj.2025.5.e4
Ren, J., Chen, X., & Wang, X. (2025). Emerging therapeutic frontiers in cardiometabolic and inflammatory diseases. British Journal of Pharmacology, 182(20), 4737–4740. https://doi.org/10.1111/bph.70159
Theodorakis, N., Nikolaou, M., & Krentz, A. (2025). Cardiovascular-endocrine-metabolic medicine: Proposing a new clinical sub-specialty amid the cardiometabolic pandemic. Biomolecules, 15(3), 373. https://doi.org/10.3390/biom15030373