Sarcopenia in Diabetes: Managing Muscle Loss with Chronic Disease
"Discover how type 2 diabetes accelerates muscle loss and learn evidence-based strategies to prevent, manage, and even reverse diabetic sarcopenia. Explore the latest research on exercise, nutrition, and metabolic interventions to preserve strength, independence, and metabolic health."
SARCOPENIA
Dr. T.S. Didwal, M.D.
11/20/202512 min read
What if the muscle loss you’re experiencing isn’t just ‘aging,’ but a silent consequence of your diabetes? Recent research shows that type 2 diabetes doesn’t just affect your blood sugar—it accelerates the breakdown of your muscles, creating a hidden metabolic trap that worsens both conditions. Understanding and reversing diabetic sarcopenia isn’t optional—it’s central to maintaining strength, independence, and healthy metabolism as you age."
Clinical Pearls:
Bidirectional Risk: Diabetes increases sarcopenia risk by up to 30%, and sarcopenia in turn worsens glycemic control.
Early Detection is Key: Functional decline often precedes noticeable muscle loss; routine screening for grip strength, gait speed, and muscle mass is essential.
Resistance Training Reigns: Progressive resistance exercises are the single most effective intervention to restore muscle mass and improve insulin sensitivity.
Nutrition is Non-Negotiable: Adequate protein intake (1.2–1.5 g/kg/day) distributed across meals, combined with vitamin D optimization, significantly enhances muscle recovery.
Multifactorial Management: Successful intervention requires addressing insulin resistance, inflammation, mitochondrial dysfunction, hormonal imbalances, and myokine dysregulation, not just exercise alone.
Understanding the Muscle-Diabetes Connection
Let's start with the basics. Sarcopenia refers to the progressive loss of skeletal muscle mass, strength, and function. While it typically affects older adults, when combined with type 2 diabetes mellitus (T2DM), it creates what researchers now recognize as a unique metabolic syndrome.
Think of your muscles as your body's metabolic powerhouse. They're not just there to help you lift groceries or climb stairs—they're actively involved in regulating your blood sugar. When diabetes enters the picture, this powerhouse starts to deteriorate faster than it should, creating what scientists call diabetic sarcopenia or type 2 diabetes mellitus-related sarcopenia (T2DM-RS).
Why This Matters More Than You Think
The relationship between diabetes and muscle loss isn't just coincidental—it's bidirectional and potentially devastating. According to Ortez Toro (2025), individuals with diabetes face a 30% higher risk of developing sarcopenia compared to their non-diabetic counterparts. But here's the kicker: sarcopenia also increases your risk of developing diabetes in the first place.
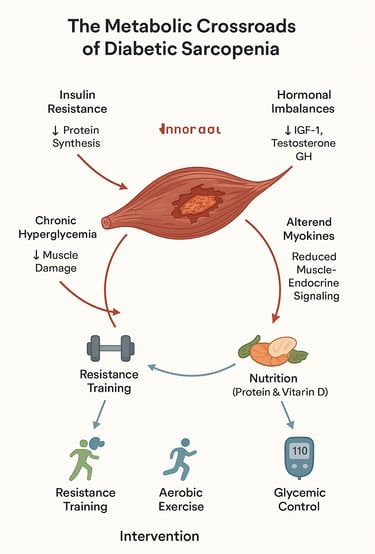
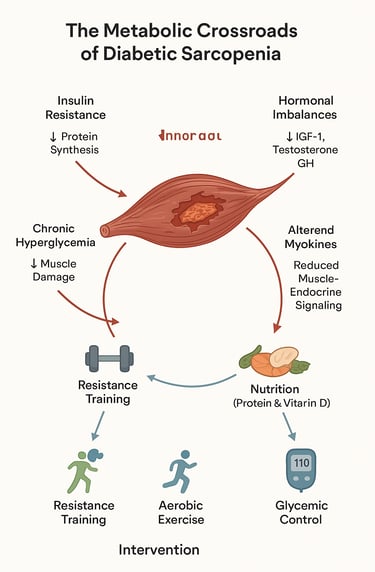
This creates what researchers describe as a "metabolic crossroads" where muscle loss and glycemic dysregulation feed into each other, progressively worsening both conditions (Ortez Toro, 2025).
The Science Behind T2DM-Related Sarcopenia: A Distinct Condition
Not Your Average Muscle Loss
One of the most groundbreaking insights from recent research is that T2DM-related sarcopenia isn't simply regular sarcopenia happening in people with diabetes. Liu et al. (2024) make a compelling case that it's actually a distinct type of muscle atrophy with its own unique characteristics.
Key Takeaways from :
T2DM-RS has different pathological mechanisms compared to age-related sarcopenia or disuse atrophy
The condition involves specific molecular pathways related to insulin resistance and chronic inflammation
Mitochondrial dysfunction plays a central role in diabetic muscle loss
Traditional sarcopenia interventions may not be sufficient without addressing the underlying diabetic metabolic dysfunction
The researchers emphasize that T2DM-RS results from a complex interplay of metabolic dysregulation, chronic inflammation, oxidative stress, and hormonal imbalances that are specific to the diabetic state (Liu et al., 2024). This means that managing this condition requires more than just standard muscle-building exercises—it demands a comprehensive approach targeting the diabetic pathology itself.
The Metabolic Crossroads Explained
Ortez Toro (2025) provides an excellent framework for understanding how diabetes and sarcopenia intersect. The study identifies several critical mechanisms:
Key Takeaways:
Insulin resistance in muscle tissue impairs protein synthesis and accelerates protein breakdown
Chronic hyperglycemia (high blood sugar) creates advanced glycation end-products (AGEs) that damage muscle proteins
Systemic inflammation in diabetes releases cytokines that promote muscle degradation
Diabetic complications like neuropathy and vascular disease reduce physical activity, leading to disuse atrophy
The prevalence of sarcopenia in diabetes populations ranges from 15% to 30%, depending on diagnostic criteria
The research emphasizes that this isn't just about having two conditions simultaneously—it's about how they amplify each other's harmful effects. Diabetes makes sarcopenia worse, and sarcopenia makes diabetes harder to control
Clinical Implications and Diagnostic Challenges
Sathyakumar (2025) provides crucial insights into the clinical reality of managing T2DM-related sarcopenia in practice. This study highlights several important considerations for both patients and healthcare providers.
Key Takeaways
Early diagnosis is critical but often missed because muscle loss develops gradually
Standard diabetes management doesn't automatically address sarcopenia risk
Screening for muscle loss should be integrated into routine diabetes care
Both muscle mass and muscle function must be assessed for accurate diagnosis
The condition significantly increases risk of falls, fractures, and loss of independence
Sathyakumar emphasizes that diabetic sarcopenia represents a major public health concern that's currently underrecognized in clinical practice. The study advocates for systematic screening protocols in diabetes clinics to identify at-risk individuals before significant functional decline occurs.
The Pathophysiology: Why Diabetes Destroys Muscle
Understanding the "why" behind diabetic sarcopenia helps us appreciate why targeted interventions are so crucial. Multiple interconnected mechanisms are at play:
1. Insulin Resistance: The Master Disruptor
In healthy muscle tissue, insulin acts as a key regulator of protein metabolism, promoting protein synthesis and inhibiting breakdown. But in diabetes, muscle cells become resistant to insulin's signals. Chen et al. (2023) explain that this insulin resistance creates an imbalance in protein turnover, where breakdown exceeds synthesis.
Key Takeaways :
Insulin resistance directly impairs the mTOR pathway, which is essential for muscle protein synthesis
The PI3K/Akt signaling pathway becomes dysfunctional in diabetic muscle
Chronic hyperglycemia induces oxidative stress that damages muscle fibers
AGEs accumulation in muscle tissue leads to increased stiffness and reduced function
The condition creates a vicious cycle: muscle loss reduces glucose disposal capacity, worsening insulin resistance
The researchers note that skeletal muscle is responsible for approximately 80% of insulin-mediated glucose disposal in the body. When muscle mass decreases, this metabolic capacity diminishes, creating a feedback loop that perpetuates both conditions
2. Chronic Inflammation and Oxidative Stress
Diabetes creates a state of chronic low-grade inflammation throughout the body. Pro-inflammatory cytokines like TNF-α and IL-6 not only worsen insulin resistance but also directly promote muscle protein breakdown through the ubiquitin-proteasome system.
Liu et al. (2024) describe how this inflammatory milieu creates "inflammaging"—a persistent inflammatory state that accelerates biological aging processes, including muscle deterioration.
3. Mitochondrial Dysfunction
Your muscles are packed with mitochondria—the cellular powerhouses that generate energy. In diabetes, these mitochondria become dysfunctional, producing less ATP (energy) and more reactive oxygen species (free radicals). This double whammy reduces muscle function while simultaneously damaging muscle proteins (Liu et al., 2024).
4. Hormonal Imbalances
Diabetes affects multiple hormone systems beyond insulin. Reduced levels of growth hormone, testosterone, and IGF-1 (insulin-like growth factor 1) all contribute to impaired muscle protein synthesis and accelerated loss (Chen et al., 2023).
5. Altered Myokine Secretion
Muscles aren't just passive tissues—they're endocrine organs that secrete signaling molecules called myokines. In diabetic sarcopenia, the pattern of myokine secretion becomes dysfunctional, reducing the muscle's ability to maintain itself and communicate properly with other organs (Liu et al., 2024).
Breaking the Cycle: Therapeutic Lifestyle Interventions
Here's the good news: while T2DM-related sarcopenia is serious, it's not inevitable, and it's certainly not irreversible. Marcotte-Chénard et al. (2023) provide a comprehensive review of evidence-based lifestyle interventions that can prevent and even reverse diabetic muscle loss.
Key Takeaways from Marcotte-Chénard et al. (2023):
Combined resistance training and aerobic exercise is the most effective non-pharmaceutical intervention
Protein supplementation can enhance muscle protein synthesis when combined with exercise
Optimal protein intake for individuals with T2DM-related sarcopenia is 1.2-1.5 g/kg body weight per day
Vitamin D supplementation shows promise for improving muscle strength in deficient individuals
Lifestyle interventions must be sustained long-term to maintain benefits
Resistance Training: Your Best Defense
The gold standard for combating sarcopenia is progressive resistance training. This means exercises that challenge your muscles against resistance—think weight lifting, resistance bands, or bodyweight exercises.
Marcotte-Chénard et al. (2023) review multiple studies showing that resistance training:
Increases muscle mass and strength in people with T2DM
Improves insulin sensitivity and glycemic control
Enhances mitochondrial function
Reduces systemic inflammation
Improves physical function and quality of life
The recommended protocol? At least 2-3 sessions per week, targeting all major muscle groups, with progressive overload (gradually increasing resistance over time).
Aerobic Exercise: The Metabolic Booster
While resistance training builds muscle, aerobic exercise (like walking, cycling, or swimming) improves cardiovascular health, insulin sensitivity, and overall metabolic function. Marcotte-Chénard et al. (2023) emphasize that combining both types of exercise produces superior results compared to either alone.
The sweet spot? 150 minutes per week of moderate-intensity aerobic activity, spread throughout the week, in addition to your resistance training sessions.
High-Intensity Interval Training (HIIT): Time-Efficient Effectiveness
For those pressed for time, HIIT offers remarkable benefits. This involves short bursts of intense exercise alternated with recovery periods. Studies cited by Marcotte-Chénard et al. (2023) show that HIIT can improve muscle quality, insulin sensitivity, and cardiorespiratory fitness in as little as 20-30 minutes per session, 2-3 times per week.
Nutritional Strategies: Feeding Your Muscles
Exercise alone isn't enough—you need to feed your muscles appropriately. Chen et al. (2023) and Marcotte-Chénard et al. (2023) both emphasize the critical role of nutrition:
Protein: The building block of muscle. Aim for 1.2-1.5 g/kg of body weight daily, distributed across all meals. For a 70 kg (154 lb) person, that's 84-105 grams per day.
Timing: Consume protein soon after resistance training (within 1-2 hours) to maximize muscle protein synthesis.
Quality: Choose high-quality protein sources rich in essential amino acids, particularly leucine (found in meat, dairy, eggs, and legumes).
Vitamin D: Deficiency is common in people with diabetes and correlates with sarcopenia risk. Consider supplementation if deficient (Marcotte-Chénard et al., 2023).
Omega-3 Fatty Acids: May help reduce inflammation and support muscle health. Found in fatty fish, walnuts, and flaxseeds.
Blood Sugar Control: The Foundation
None of these interventions will work optimally if your diabetes remains poorly controlled. Chen et al. (2023) emphasize that maintaining HbA1c levels below 7% is crucial for preventing the metabolic damage that drives muscle loss.
This means:
Consistent medication adherence
Regular blood glucose monitoring
Working closely with your healthcare team
Maintaining a balanced, diabetes-appropriate diet
Emerging and Potential Therapeutic Strategies
Beyond lifestyle modifications, researchers are investigating various pharmacological and nutraceutical approaches:
Pharmacological Approaches
Metformin: The first-line diabetes medication may have protective effects on muscle through AMPK activation, though more research is needed.
GLP-1 Receptor Agonists: These newer diabetes medications may help preserve muscle mass during weight loss, though careful monitoring is needed.
Vitamin D Supplementation: Shows promise for improving muscle strength and function in deficient individuals (Marcotte-Chénard et al., 2023).
Antioxidant Supplementation: Compounds like coenzyme Q10, alpha-lipoic acid, and resveratrol are being investigated for their potential to reduce oxidative stress and inflammation.
Cautions About Weight Loss Medications
It's important to note that rapid weight loss—whether through lifestyle changes or medications—can accelerate muscle loss if not managed properly. Chen et al. (2023) emphasize that any weight loss strategy must be combined with resistance training and adequate protein intake to preserve muscle mass.
Practical Implementation: Your Action Plan
Step 1: Get Assessed
Body composition analysis (DEXA scan or bioimpedance)
Grip strength testing
Gait speed assessment
Chair stand test
Blood tests (including vitamin D levels)
Step 2: Start Moving (Safely)
Start slowly with medical clearance
Work with a physical therapist or exercise physiologist initially
Begin with bodyweight exercises and light resistance
Monitor blood sugar before and after exercise
Stay hydrated and carry fast-acting carbohydrates for hypoglycemia
Step 3: Optimize Your Nutrition
Calculate your protein needs (1.2-1.5 g/kg body weight)
Distribute protein across all meals
Don't fear carbohydrates—choose complex, fiber-rich options
Include anti-inflammatory foods (fatty fish, berries, leafy greens)
Consider meeting with a registered dietitian specializing in diabetes
Step 4: Build Your Routine
Monday: Resistance training (full body)
Tuesday: Moderate-intensity aerobic exercise
Wednesday: Rest or gentle activity
Thursday: Resistance training (full body)
Friday: Aerobic exercise or HIIT
Weekend: Active leisure (walking, cycling, swimming)
Step 5: Monitor and Adjust
Regular blood sugar monitoring
Periodic HbA1c checks
Functional assessments (how easily can you perform daily activities?)
Body composition changes
Strength improvements
Frequently Asked Questions
Q: How do I know if I have diabetic sarcopenia?
A: Warning signs include difficulty rising from a chair without using your arms, reduced grip strength, unexplained falls, slower walking speed, and progressive difficulty with daily activities. Formal diagnosis requires assessment of muscle mass (via DEXA scan or similar), muscle strength (grip strength test), and physical performance (gait speed, chair stands). Ask your doctor about screening if you have diabetes and are over 50 or experiencing any of these symptoms.
Q: Can I reverse diabetic sarcopenia, or is it permanent?
A: The good news is that significant improvements are possible with appropriate intervention. Marcotte-Chénard et al. (2023) show that consistent resistance training combined with adequate protein intake can increase muscle mass and strength even in older adults with T2DM. However, Liu et al. (2024) emphasize that because this is a distinct metabolic condition, interventions must address both the muscle loss and the underlying diabetic pathology. Complete reversal may not always be possible, but meaningful functional improvements certainly are.
Q: How much protein do I really need?
A: Research suggests 1.2-1.5 grams per kilogram of body weight daily (Marcotte-Chénard et al., 2023). For a 70 kg (154 lb) person, that's 84-105 grams per day. Distribute this across all meals (20-30 grams per meal) for optimal muscle protein synthesis. Choose high-quality sources rich in essential amino acids, particularly leucine.
Q: Will resistance training affect my blood sugar?
A: Yes—usually in a good way! Resistance training improves insulin sensitivity and can help lower blood sugar levels. However, Chen et al. (2023) note that you should monitor your glucose before and after exercise, especially initially, as adjustments to your diabetes medications may be needed. Always carry fast-acting carbohydrates during exercise in case of hypoglycemia.
Q: I have diabetic neuropathy in my feet. Can I still exercise?
A: Absolutely, though you'll need to modify your approach. Liu et al. (2024) emphasize that diabetic complications require careful planning but don't disqualify you from intervention. Consider seated resistance exercises, swimming, or stationary cycling which are gentler on your feet. Work with a physical therapist or exercise specialist familiar with diabetes to create a safe program. Inspect your feet daily and wear proper footwear.
Q: What's the single most important thing I can do?
A: If we had to choose one intervention, it would be resistance training combined with adequate protein intake. However, Chen et al. (2023) and Sathyakumar (2025) stress that optimal blood glucose control is the foundation—without it, no intervention will work optimally. So realistically, the most important thing is a comprehensive approach that addresses both muscle health and metabolic control simultaneously.
Q: Should I be taking any supplements?
A: The evidence is strongest for vitamin D if you're deficient—many people with diabetes are (Marcotte-Chénard et al., 2023). Beyond that, focus on getting nutrients from whole foods. Some research supports omega-3 fatty acids and certain antioxidants, but these should complement, not replace, the core interventions of exercise and nutrition. Always discuss supplements with your healthcare provider, as some may interact with diabetes medications.
Q: How long before I see results?
A: Functional improvements (feeling stronger, moving better) can occur within 4-8 weeks of starting a consistent exercise program. Measurable increases in muscle mass typically take 8-12 weeks or longer. Marcotte-Chénard et al. (2023) emphasize that these interventions must be maintained long-term—think lifestyle change, not quick fix. The improvements will continue as long as you maintain the program.
Q: Can medications help?
A: Currently, no medications are specifically approved for treating sarcopenia. However, optimal management of your diabetes with appropriate medications is crucial. Chen et al. (2023) discuss emerging research on various compounds, but lifestyle interventions remain the cornerstone of treatment. Never discontinue or modify diabetes medications without consulting your healthcare provider.
Q: Is this condition common?
A: Yes, more than you might think. Ortez Toro (2025) reports that sarcopenia prevalence in diabetes populations ranges from 15-30%, with individuals with diabetes facing a 30% higher risk compared to those without diabetes. However, it's significantly underdiagnosed because it develops gradually and screening isn't routinely performed in diabetes clinics (Sathyakumar, 2025).
Final Thoughts
The intersection of sarcopenia and diabetes represents one of the most significant yet underrecognized health challenges of our time. As Liu et al. (2024) eloquently demonstrate, this isn't just two conditions coexisting—it's a distinct metabolic syndrome that demands our attention and action.
But here's the empowering truth: you're not powerless. The research from Marcotte-Chénard et al. (2023), Chen et al. (2023), Ortez Toro (2025), and Sathyakumar (2025) consistently shows that evidence-based lifestyle interventions can prevent, slow, and even reverse diabetic muscle loss.
Your muscles are remarkable organs capable of regeneration and adaptation throughout your entire life. With the right stimulus—resistance exercise—and the right fuel—adequate protein and optimal blood glucose control—they can rebuild and strengthen even after years of diabetes.
The question isn't whether intervention works. The science is clear: it does. The question is whether you'll take action.
Your future self—stronger, more independent, with better diabetes control and higher quality of life—is waiting for you to make that decision. Why not start today?
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Individual circumstances vary, and treatment decisions should always be made in consultation with qualified healthcare professionals.
Related Articles
Resistance Training for Sarcopenia: A Beginner's Workout Plan | DR T S DIDWAL
Sarcopenia & Cardiovascular Disease: How Poor Muscle Mass Predicts Mortality | DR T S DIDWAL
Vitamin D Deficiency and Sarcopenia: The Critical Connection | DR T S DIDWAL
How to Prevent Sarcopenia: Fight Age-Related Muscle Loss and Stay Strong | DR T S DIDWAL
Who Gets Sarcopenia? Key Risk Factors & High-Risk Groups Explained | DR T S DIDWAL
Sarcopenia: The Complete Guide to Age-Related Muscle Loss and How to Fight It | DR T S DIDWAL
Best Exercises for Sarcopenia: Strength Training Guide for Older Adults | DR T S DIDWAL
Best Supplements for Sarcopenia: Vitamin D, Creatine, and HMB Explained | DR T S DIDWAL
References
Chen, H., Huang, X., Dong, M., Wen, S., Zhou, L., & Yuan, X. (2023). The association between sarcopenia and diabetes: From pathophysiology mechanism to therapeutic strategy. Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy, 16, 1541–1554. https://doi.org/10.2147/DMSO.S410834
Liu, Z., Guo, Y., & Zheng, C. (2024). Type 2 diabetes mellitus related sarcopenia: A type of muscle loss distinct from sarcopenia and disuse muscle atrophy. Frontiers in Endocrinology, 15, 1375610. https://doi.org/10.3389/fendo.2024.1375610
Marcotte-Chénard, A., Oliveira, B., Little, J. P., & Candow, D. G. (2023). Sarcopenia and type 2 diabetes: Pathophysiology and potential therapeutic lifestyle interventions. Diabetes & Metabolic Syndrome, 17(9), 102835. c
Ortez Toro, J. J. (2025). Diabetes and sarcopenia: Unraveling the metabolic crossroads of muscle loss and glycemic dysregulation. Endocrines, 6(3), 47. https://doi.org/10.3390/endocrines6030047
Sathyakumar, S. (2025). Type 2 diabetes and sarcopenia. Apollo Medicine, 22(3), 249–256. https://doi.org/10.1177/09760016251326660