Metabolically Healthy Obesity: Why "Healthy" Doesn't Mean Safe
Recent research and the 2025 ESC consensus debunk the myth of "safe" obesity. Learn about the true cardiovascular risks (subclinical atherosclerosis) and new management strategies.
OBESITY
Dr. T.S. Didwal, M.D.
12/2/202512 min read
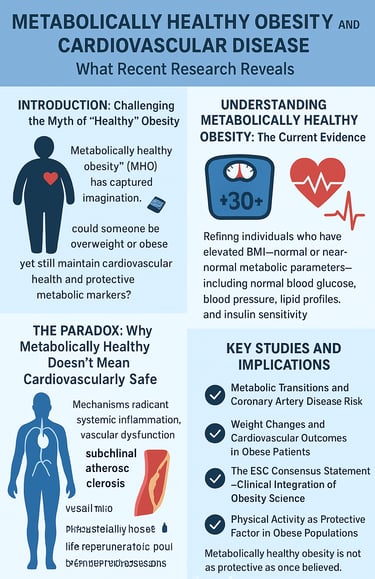
For years, the concept of metabolically healthy obesity (MHO) has captured the imagination of both patients and researchers alike. The idea is seductive: could someone be overweight or obese yet still maintain cardiovascular health and protective metabolic markers? While this notion offers hope to millions struggling with weight management, emerging evidence suggests the reality is far more complicated. Recent research indicates that even individuals classified as metabolically healthy obese face significant risks for incident cardiovascular disease—and this distinction carries profound implications for how we approach obesity management and cardiovascular prevention strategies.
The relationship between obesity and cardiovascular disease represents one of modern medicine's most pressing public health challenges. According to recent comprehensive research, the traditional view that obesity with favorable metabolic profiles represents a "safe" phenotype requires substantial reconsideration. This blog post synthesizes cutting-edge research to explore what we now know about metabolically healthy obesity, why it may not be as protective as once believed, and what individuals and healthcare providers should do about it.
Clinical Pearls
1. Your Labs Are Great, But They Aren't a Shield.
The Science: While your metabolic markers (blood sugar, lipids) are currently normal, the latest research shows that MHO does not confer cardiovascular immunity. Excess body fat itself is an independent risk factor, and the apparent "protection" can mask underlying issues like subclinical atherosclerosis (plaque buildup) and chronic vascular dysfunction.
The Takeaway: We must look beyond simple lab results. Favorable metabolic markers are a wonderful starting point, but they are not a green light to skip proactive prevention.
2. Metabolic Health is a Moving Target, Not a Fixed Status.
The Science: Large cohort studies (like the one with 69,272 participants) confirm that MHO is often a transitional state. Many individuals classified as MHO progress to metabolically unhealthy obesity over time, at which point cardiovascular risk accelerates dramatically.
The Takeaway: Time is not on your side. Proactive, modest intervention now can stabilize your favorable metabolic state and prevent the progression to higher-risk categories in the future.
3. Exercise Protects Your Heart, Even Without Major Weight Loss.
The Science: Physical activity provides independent cardiovascular benefits. Regular exercise improves vascular endothelial function and reduces systemic inflammation, offering protection regardless of whether the number on the scale moves much.
The Takeaway: Don't let weight loss be your only goal for activity. Consistent movement is a direct medicine for your heart and blood vessels. Aim for 150 minutes of moderate activity weekly.
4. Modest Weight Reduction Offers Major Cardiovascular Returns.
The Science: You do not need to reach an "ideal" BMI to see significant benefits. Evidence overwhelmingly shows that even 5% to 10% weight reduction produces measurable improvements in cardiovascular outcomes and risk reduction.
The Takeaway: Focus on small, sustainable victories. Losing just 5% of your body weight is an achievable, powerful health goal that directly protects your heart.
5. We Must Treat the Obesity, Not Just the Blood Test.
The Science: Leading bodies, such as the ESC, now recommend against using the MHO label to delay treatment. Because obesity is a chronic disease with systemic effects, comprehensive management—including a discussion of new agents like GLP-1 receptor agonists (if appropriate)—should be offered to all patients with obesity.
The Takeaway: Let's partner to manage your weight proactively. We have advanced, effective tools available now that treat the underlying metabolic condition, offering you the best chance for long-term health.
Understanding Metabolically Healthy Obesity: The Current Evidence
Metabolically healthy obesity describes individuals who maintain elevated body mass index (BMI)—typically above 30 kg/m²—while demonstrating normal or near-normal metabolic parameters. These typically include normal blood glucose, blood pressure, lipid profiles, and insulin sensitivity. For decades, this classification suggested a protective phenotype, a potential safe harbor from obesity-related complications.
However, recent research fundamentally challenges this reassuring narrative. In a landmark clinical cohort study examining 69,272 individuals, researchers investigated the critical question: what happens when metabolically healthy individuals transition into different metabolic health categories? The findings proved startling. (Shuey et al., 2025) Transitions in metabolic health status significantly affected risk of coronary artery disease—not just for those becoming unhealthier, but for those remaining metabolically healthy yet obese. This suggests that metabolic health classification may represent merely a snapshot, potentially missing underlying cardiovascular vulnerability.
The European Society of Cardiology's recent clinical consensus statement on obesity and cardiovascular disease emphasizes that metabolic health should not be interpreted as protection against cardiovascular complications. (Koskinas et al., 2025) Rather, excess adipose tissue itself—regardless of traditional metabolic markers—represents an independent risk factor for cardiovascular events. This distinction is crucial because it suggests that weight reduction, not just metabolic optimization, remains essential for cardiovascular protection.
The Paradox: Why Metabolically Healthy Doesn't Mean Cardiovascularly Safe
One of the most important discoveries emerging from recent literature involves what researchers call the "obesity paradox"—the counterintuitive observation that some metabolically healthy obese individuals do develop cardiovascular disease despite favorable metabolic profiles. Why does this happen?
Recent advances in obesity research highlight several mechanisms that explain this apparent paradox. First, traditional metabolic markers may not capture the full spectrum of metabolic dysfunction. While glucose tolerance and lipid profiles appear normal, other pathological processes continue silently. These include systemic inflammation, vascular dysfunction, impaired endothelial function, and adipose tissue dysfunction. Advanced imaging and biomarker studies reveal that metabolically healthy obese individuals often demonstrate subclinical atherosclerosis—plaque buildup that hasn't yet caused symptoms but represents real cardiovascular disease developing beneath the surface.
Second, the volume and distribution of adipose tissue itself poses problems, independent of traditional metabolic markers. (Janić et al., 2025) Visceral adiposity—fat deposits around internal organs—produces inflammatory cytokines and adipokines that promote atherosclerosis and vascular dysfunction. Even without dyslipidemia or hyperglycemia, this pathological adipose tissue remodeling creates a pro-inflammatory, pro-thrombotic environment conducive to cardiovascular events.
Third, metabolic health classifications capture a single moment in time. The aforementioned 69,272-participant study demonstrated that metabolic health status frequently transitions. (Shuey et al., 2025) Many individuals classified as metabolically healthy obese progress toward metabolic dysfunction, at which point cardiovascular risk escalates dramatically. Conversely, even those maintaining metabolic health while obese show cumulative cardiovascular damage with time. This suggests that metabolic health status represents a moving target rather than a stable, protective phenotype.
What the Latest Research Shows: Key Studies and Implications
Study 1: Metabolic Transitions and Coronary Artery Disease Risk
The large clinical cohort study examining 69,272 participants provides crucial epidemiological evidence. (Shuey et al., 2025) Researchers tracked individuals across different metabolic health categories, distinguishing between those who remained metabolically healthy obese, those who transitioned to metabolic dysfunction, and various other categories. The key finding: individuals transitioning from metabolic health to metabolic dysfunction experienced substantially elevated coronary artery disease risk. However, critically, even those remaining metabolically healthy obese showed elevated risk compared to normal-weight metabolically healthy individuals.
Key Takeaway: Simply maintaining favorable metabolic markers while obese does not eliminate cardiovascular risk. The presence of excess adiposity itself, even without metabolic dysfunction, increases disease susceptibility.
Study 2: Weight Changes and Cardiovascular Outcomes in Obese Patients
Another prospective cohort study examined 454 obese patients with existing cardiovascular disease, analyzing the relationship between weight changes and subsequent cardiovascular events. (Zhang et al., 2025) The results delivered an important message: weight reduction correlated with improved cardiovascular outcomes, while weight gain associated with worse prognosis. Notably, weight reduction benefits occurred across the metabolic health spectrum—even metabolically healthy obese patients showed cardiovascular advantages from weight loss.
This finding directly challenges the notion that metabolically healthy obesity requires no intervention. Instead, it suggests that weight reduction should remain a primary therapeutic goal regardless of current metabolic status.
Key Takeaway: Among individuals with existing cardiovascular disease, weight loss improves outcomes and reduces cardiovascular event risk, indicating that metabolic health status should not dissuade practitioners from recommending weight reduction.
Study 3: The ESC Consensus Statement—Clinical Integration of Obesity Science
The European Society of Cardiology's 2025 consensus statement represents the most comprehensive contemporary synthesis of obesity and cardiovascular disease evidence available to clinicians. (Koskinas et al., 2025) This authoritative document emphasizes several critical points:
Obesity represents a chronic disease requiring comprehensive management, not merely a cosmetic concern. The statement stresses that metabolic health phenotypes should not guide clinical decision-making regarding obesity management. Rather, all individuals with obesity—regardless of metabolic profile—merit lifestyle interventions, consideration of pharmacotherapy, and, in appropriate cases, bariatric surgery. The document explicitly recommends that clinicians avoid falsely reassuring patients that metabolically favourable profiles protect against cardiovascular disease.
The consensus statement further highlights that cardiovascular risk reduction requires multifaceted approaches, including medical optimization of blood pressure, cholesterol, and glucose metabolism alongside weight management. (Koskinas et al., 2025) Emerging pharmacological agents specifically developed for weight management, including GLP-1 receptor agonists, demonstrate cardiovascular benefits independent of their weight-reducing properties, suggesting that metabolically active medications offer advantages beyond simple weight reduction.
Key Takeaway: Leading cardiovascular organizations now explicitly recommend against metabolic health-based stratification when managing obesity. Comprehensive management applying consistent principles across metabolic phenotypes represents best practice.
Study 4: Physical Activity as a Protective Factor in Obese Populations
Recent research examining obesity management emphasizes that physical activity provides cardiovascular benefits even without substantial weight loss. Studies demonstrate that obese individuals engaging in regular physical activity show improved vascular function, reduced inflammation, and decreased cardiovascular event rates compared to sedentary obese individuals, even among those maintaining similar body weights.
This finding carries important implications: while weight reduction remains beneficial, clinicians should not make physical activity recommendations contingent on weight loss success. Independent cardiovascular protective effects occur through improved metabolic profile, reduced systemic inflammation, improved vascular endothelial function, and favorable psychological impacts.
Key Takeaway: Physical activity should be recommended universally to obese individuals regardless of weight loss success, given its independent cardiovascular benefits.
Study 5: Comprehensive Intervention Outcomes—Weight Control and Cardiovascular Events
A recent umbrella review synthesizing systematic reviews and meta-analyses examined whether weight control interventions reduce cardiovascular outcomes. The analysis included hundreds of studies collectively examining hundreds of thousands of participants. The conclusions proved definitive: structured weight loss interventions reduce cardiovascular event risk and mortality. Benefits emerged across intervention types, including lifestyle modification, pharmacological therapy, and bariatric surgery.
Notably, even modest weight reductions of 5-10% produced measurable cardiovascular benefits, suggesting that individuals need not achieve ideal body weight to realize cardiovascular protection. This finding offers realistic, achievable targets for many patients.
Key Takeaway: Evidence overwhelmingly supports weight management interventions for cardiovascular disease reduction. Modest weight loss produces meaningful cardiovascular benefits; perfection regarding ideal body weight remains unnecessary.
Study 6: Obesity, Cardiovascular Risk Assessment, and Management Framework
Recent literature emphasizes that comprehensive cardiovascular risk assessment in obese populations requires consideration of multiple factors beyond traditional metabolic markers. Advanced assessments may include vascular imaging (carotid intima-media thickness, coronary calcium scoring), biomarkers of inflammation and vascular dysfunction (high-sensitivity C-reactive protein, NT-proBNP), and functional assessments (exercise capacity, heart rate variability).
Furthermore, managing obesity-related cardiovascular complications requires addressing not just weight itself but associated conditions including hypertension, dyslipidemia, diabetes, sleep apnea, and cardiac dysfunction. Integrated approaches addressing multiple pathways prove more effective than single-target interventions.
Key Takeaway: Comprehensive cardiovascular risk assessment incorporating functional and biomarker-based evaluations alongside traditional metabolic markers provides superior risk stratification in obese populations.
The Bottom Line: Why Metabolically Healthy Obesity Remains a Concern
After reviewing current evidence, several conclusions emerge clearly:
Metabolically healthy obesity should not be considered "safe" from a cardiovascular perspective. While individuals demonstrating favorable metabolic profiles show lower absolute cardiovascular risk than those with metabolic dysfunction, they still carry elevated risk compared to normal-weight individuals with similar metabolic profiles. The apparent health of metabolic markers masks underlying pathological processes including subclinical atherosclerosis, systemic inflammation, and vascular dysfunction.
Metabolic status represents a dynamic state rather than a fixed category. Many individuals classified as metabolically healthy obese progress toward metabolic dysfunction over time. This progression accelerates cardiovascular risk development, emphasizing the importance of early preventive intervention.
Weight reduction benefits all obese individuals, regardless of current metabolic status. Recent studies demonstrate cardiovascular advantages from weight loss even among metabolically healthy obese individuals, refuting any argument that such individuals require no intervention.
Comprehensive management approaches prove superior to status-based strategies. Rather than categorizing patients as "safe" if metabolically healthy, clinicians should offer all obese individuals integrated approaches addressing weight, physical activity, cardiovascular risk factors, and comorbid conditions.
Practical Implications for Patients and Providers
For Patients
If you've been told that you're "metabolically healthy" despite obesity, this research carries important messages. First, that classification does not mean your cardiovascular health is fully protected. Second, this should not discourage you but rather motivate appropriate preventive action. The good news: evidence clearly demonstrates that weight reduction, physical activity, and comprehensive cardiovascular risk management work. Even modest changes produce measurable benefits.
Consider working with your healthcare team to develop a comprehensive plan incorporating:
Structured weight loss programs combining dietary modification, physical activity, and behavioral support. Even 5-10% weight reduction produces cardiovascular benefits.
Regular physical activity, ideally 150 minutes weekly of moderate-intensity aerobic activity plus resistance training. Benefits occur independent of weight loss.
Comprehensive metabolic and cardiovascular assessment, including traditional risk factors plus advanced markers and imaging when appropriate.
Treatment of associated conditions, including hypertension, dyslipidemia, and sleep disorders.
Consideration of pharmacological interventions if lifestyle modifications prove insufficient, particularly newer agents like GLP-1 receptor agonists, demonstrating cardiovascular benefits.
For Healthcare Providers
The recent ESC consensus statement and supporting literature provide clear guidance: metabolic health phenotypes should not guide obesity management decisions. All obese patients warrant comprehensive intervention offers regardless of current metabolic profile. This includes:
Systematic assessment of cardiovascular risk incorporating both traditional factors and novel biomarkers/imaging when appropriate, especially in asymptomatic individuals.
Universal recommendations for physical activity, even without weight loss expectations, give independent cardiovascular benefits.
Consideration of pharmacological therapy alongside lifestyle modification. Growing evidence supports pharmacological agents, particularly GLP-1 receptor agonists and newer combinations, for cardiovascular risk reduction.
Bariatric surgery referral for appropriate candidates, particularly those with BMI >40 or ≥35 with significant comorbidities, given demonstrated cardiovascular benefits.
Avoidance of false reassurance based on metabolic health classifications. Clear communication that metabolic health does not eliminate obesity-related cardiovascular risk remains important.
Addressing Common Questions: FAQ
Q: If I'm metabolically healthy and obese, do I really need to lose weight?
A: Yes. While your current metabolic profile appears favorable, research demonstrates that excess adiposity itself poses cardiovascular risks independent of traditional metabolic markers. Moreover, metabolic health often transitions to dysfunction over time. Weight reduction provides measurable cardiovascular benefits regardless of current metabolic status.
Q: How much weight do I need to lose to see cardiovascular benefits?
A: You don't need to achieve ideal body weight. Research shows that even 5-10% weight reduction produces measurable cardiovascular improvements. This modest, achievable goal should serve as initial target for most individuals.
Q: Is exercise really helpful if I don't lose weight?
A: Absolutely. Physical activity provides cardiovascular benefits independent of weight loss, improving vascular function, reducing inflammation, and decreasing cardiovascular event risk. Exercise should be recommended universally regardless of weight loss success.
Q: My metabolic markers are all normal. Should I still take medications for weight loss?
A: Recent evidence supports considering weight loss medications like GLP-1 receptor agonists for obese individuals with cardiovascular disease risk factors, even those with favorable metabolic profiles. These medications provide cardiovascular benefits independent of weight loss mechanisms. Discuss with your healthcare provider whether you're a candidate.
Q: Does bariatric surgery make sense if I'm metabolically healthy?
A: For appropriate candidates—typically those with BMI >40 or ≥35 with significant comorbidities—bariatric surgery demonstrates cardiovascular benefits independent of current metabolic status. If you're interested, discuss whether you meet criteria with your healthcare team.
Q: How often should I have my cardiovascular risk assessed?
A: Annual assessment remains reasonable for most obese individuals. More frequent assessment may be warranted if risk factors develop or metabolic status changes. Advanced imaging (coronary calcium scoring) or biomarker assessment may help identify subclinical disease in select individuals.
Key Takeaways
Here's what you need to remember about metabolically healthy obesity and cardiovascular disease:
Metabolic health does not equal cardiovascular safety. Metabolically healthy obese individuals remain at elevated cardiovascular disease risk compared to normal-weight individuals, and may develop cardiovascular complications despite favorable metabolic markers.
Subclinical atherosclerosis occurs frequently in metabolically healthy obese individuals, representing real disease despite lack of symptoms or metabolic markers indicating dysfunction.
Weight reduction benefits all obese individuals regardless of metabolic status. Modest weight loss (5-10%) produces meaningful cardiovascular benefits.
Physical activity provides independent cardiovascular protection separate from weight loss effects, emphasizing its universal recommendation.
Metabolic status transitions over time, with many metabolically healthy individuals progressing toward dysfunction. Early preventive intervention remains important.
Comprehensive management approaches addressing weight, physical activity, cardiovascular risk factors, and comorbidities prove superior to single-target strategies or status-based approaches.
Advanced risk assessment incorporating biomarkers and imaging may identify subclinical disease in asymptomatic individuals and guide intervention intensity.
Call to Action
If you're living with obesity—whether metabolically healthy or not—don't wait. Schedule a comprehensive cardiovascular risk assessment with your healthcare provider today. Discuss your personal risk profile and develop an individualized management plan incorporating the evidence-based strategies outlined above. Even if your metabolic markers appear favorable, remember that proactive preventive action now prevents cardiovascular disease tomorrow.
Healthcare providers: Use this evidence to confidently counsel patients that metabolic health does not confer cardiovascular immunity. Offer comprehensive intervention regardless of metabolic phenotype. The ESC consensus statement and supporting literature provide strong guidance for evidence-based obesity management in cardiovascular medicine.
The research is clear: metabolically healthy obesity requires serious attention from both patients and healthcare providers. By understanding the true cardiovascular risks, embracing evidence-based management strategies, and taking decisive preventive action, we can substantially reduce obesity-related cardiovascular disease burden.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Individual circumstances vary, and treatment decisions should always be made in consultation with qualified healthcare professionals.
Related Articles
The BMI Paradox: Why "Normal Weight" People Still Get High Blood Pressure | DR T S DIDWAL
Breakthrough Research: Leptin Reduction is Required for Sustained Weight Loss | DR T S DIDWAL
How Insulin Resistance Accelerates Cardiovascular Aging | DR T S DIDWAL
What’s New in the 2025 Blood Pressure Guidelines? A Complete Scientific Breakdown | DR T S DIDWAL
The Metabolic Triad: Why Diabetes, Obesity & CVD Are One Epidemic | DR T S DIDWAL
References
Chen, X., Zhang, X., Xiang, X., et al. (2025). Effects of weight control interventions on cardiovascular outcomes: An umbrella review of systematic reviews and meta-analyses. International Journal of Obesity, 49, 1911–1920. https://doi.org/10.1038/s41366-025-01860-z
Janić, M., Janež, A., El-Tanani, M., & Rizzo, M. (2025). Obesity: Recent advances and future perspectives. Biomedicines, 13(2), 368. https://doi.org/10.3390/biomedicines13020368
Koskinas, K. C., Van Craenenbroeck, E. M., Antoniades, C., Blüher, M., Gorter, T. M., Hanssen, H., Marx, N., McDonagh, T. A., Mingrone, G., Rosengren, A., & Prescott, E. B. (2025). Obesity and cardiovascular disease: An ESC clinical consensus statement. European Journal of Preventive Cardiology, 32(3), 184–220. https://doi.org/10.1093/eurjpc/zwae279
Perone, F., Spadafora, L., Pratesi, A., Nicolaio, G., Pala, B., Franco, G., Ruzzolini, M., & Ambrosetti, M. (2024). Obesity and cardiovascular disease: Risk assessment, physical activity, and management of complications. International Journal of Cardiology. Cardiovascular Risk and Prevention, 23, 200331. https://doi.org/10.1016/j.ijcrp.2024.200331
Shuey, M. M., Levinson, R. T., Vogel, M. E., Farber-Eger, E., Huang, S., Harrel, F. E., Jr., Hasty, A. H., Brown, J. D., Silver, H. J., Koethe, J. R., Beckman, J. A., Brown, N. J., Niswender, K. D., Cox, N. J., & Wells, Q. S. (2025). Risk of coronary artery disease associated with transitions in metabolic health in a clinical cohort of 69,272. Journal of the American Heart Association, e037597. https://doi.org/10.1161/JAHA.124.037597
Zhang, J., Schutte, R., & Pierscionek, B. (2025). Association of weight change with cardiovascular events and all-cause mortality in obese participants with cardiovascular disease: A prospective cohort study. Heart (British Cardiac Society), 111(10), 454–461. https://doi.org/10.1136/heartjnl-2024-324383