Why Your Body Resists Weight Loss: Understanding the Science of Weight Regain
Learn why your body resists weight loss. Discover how metabolic adaptation, hunger hormones, and set-point biology trigger weight regain—and what you can do about it.
OBESITY
Dr. T.S. Didwal, M.D.(Internal Medicine)
1/9/202612 min read

Why do most people regain weight—even after doing everything right?
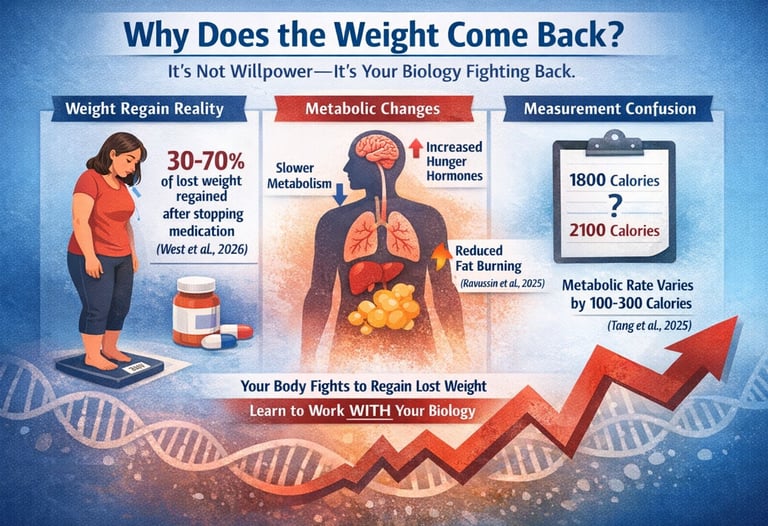
If you’ve ever lost weight only to watch it creep back, it’s not a lack of willpower. In fact, new research from 2025–2026 confirms that your body actively fights weight loss through powerful metabolic and hormonal defenses. A major BMJ meta-analysis showed that people who stop weight-management medications regain 30–70% of lost weight within a year (West et al., 2026). This isn’t a behavioral failure—it's biology.
At the same time, cutting-edge metabolic research reveals that the body’s energy systems shift dramatically after weight loss. In a Cell Metabolism study, tirzepatide preserved metabolic function and increased fat oxidation, even as participants lost significant weight (Ravussin et al., 2025). Meanwhile, liver-focused research shows that obesity disrupts the timing and resilience of the starvation-response network, making metabolic adaptation more severe (Morita et al., 2025).
Even the way we measure metabolic adaptation turns out to be inconsistent. A 2025 analysis found that predicted metabolic rate can vary by over 100–300 calories depending on the equation used (Tang et al., 2025).
These findings reshape our understanding of weight regain. The truth is simple: your biology is designed to restore lost weight—unless you learn how to work with it, not against it.
Clinical pearls
1. Your Body Isn't "Broken," It’s Highly Defensive
The 50–150 calorie drop in metabolic rate following weight loss is often called "metabolic damage," but science identifies it as adaptive thermogenesis. Think of your body like a smart home in "Power Save Mode." When it senses fewer calories coming in, it dims the lights (lowers heart rate and body temp) to survive. Understanding this helps shift the mindset from "my body is failing" to "my body is protecting me," which is essential for long-term psychological resilience.
2. The "Muscle-Metabolism" Shield
While your brain tries to lower your energy burn, resistance training acts as a biological counter-force. The Martínez-Gómez (2022) and Farhana (2025) data suggest that muscle isn't just for strength; it’s a metabolically active organ. By maintaining lean mass through high-protein intake and lifting weights, you effectively "force" your body to maintain a higher idling speed, mitigating a significant portion of the metabolic slowdown.
3. Obesity as a "Chronic" vs. "Acute" Condition
The landmark West et al. (2026) BMJ study is a game-changer for how we view medications. We don't stop taking blood pressure medication once it reaches a healthy range, yet we often expect to stop weight-loss meds once the goal weight is hit. The pearl here is continuity: because the biological pressure to regain (increased ghrelin and decreased leptin) persists indefinitely, the treatment—whether pharmacological or behavioral—must also be persistent.
4. Metabolic Flexibility: The Fat-Burning Switch
The Ravussin (2025) study on Tirzepatide highlights Metabolic Flexibility—your body’s ability to switch between burning carbs and burning fat. A healthy metabolism is like a hybrid engine. Even if you aren't on medication, you can improve this flexibility through "zone 2" cardio (steady-state) and avoiding constant snacking. This trains your mitochondria to access fat stores more efficiently, making the "maintenance" phase feel less like a constant struggle against hunger.
5. The "Equation Gap" and Self-Compassion
The Tang et al. (2025) research reveals that standard calorie calculators can be off by as much as 300 calories. If you are following a "calculated" plan and not seeing results, it’s likely the math that is wrong, not your effort.
Clinical Tip: Use calculators as a starting point, but listen to your "Bio-Feedback" (energy, sleep, and hunger) as the ultimate guide for adjusting your intake.
Weight Regain After Weight Loss: What Science Reveals About Metabolic Adaptation in 2025
Understanding the Weight Regain Phenomenon
Weight regain after successful weight loss affects up to 80% of individuals within the first year. But why does this happen? The answer lies in complex metabolic responses that extend far beyond simple willpower.
The Medication Cessation Challenge: New BMJ Findings
A comprehensive systematic review and meta-analysis published in the BMJ by West et al. (2026) examined what happens when people stop taking weight management medications. This landmark study analyzed multiple trials involving medications like GLP-1 receptor agonists (semaglutide, liraglutide) and other anti-obesity medications.
Key Takeaways from the West et al. Study:
Significant weight regain occurs within 12 months of stopping medication
The average regain ranged from 30-70% of lost weight, depending on the medication type
Metabolic changes persist even after medication cessation, contributing to regain
Behavioral interventions alone showed limited effectiveness in preventing regain post-medication
The study emphasizes the need for long-term treatment strategies rather than short-term interventions
This research highlights a critical point: weight management medications may need to be considered as long-term treatments, similar to medications for other chronic conditions like diabetes or hypertension.
Tirzepatide's Impact: Metabolic Adaptation Insights
Perhaps one of the most fascinating discoveries comes from Ravussin et al. (2025), published in Cell Metabolism. Their research on tirzepatide (a dual GIP/GLP-1 receptor agonist) challenged conventional understanding of metabolic adaptation.
Key Findings from the Ravussin Study:
Tirzepatide did not significantly impact metabolic adaptation during weight loss
The medication increased fat oxidation (the body's ability to burn fat for fuel)
Study participants showed improved metabolic flexibility compared to placebo groups
Resting metabolic rate remained relatively stable despite significant weight loss
This suggests tirzepatide may preserve metabolic function better than diet alone
This is revolutionary because it suggests that not all weight loss methods trigger the same degree of metabolic slowdown. The enhanced fat oxidation observed with tirzepatide may explain why some individuals maintain weight loss more successfully on this medication compared to traditional calorie restriction approaches.
The Liver's Role: Metabolic Networks Under Stress
Morita et al. (2025) took a different approach in their Science Signaling publication, examining how the liver's metabolic network responds to starvation and obesity at the molecular level.
Critical Insights from the Morita Study:
The starvation-responsive metabolic network shows structural robustness but temporal vulnerability
Obese mouse liver demonstrated different metabolic responses compared to healthy liver tissue
The study identified specific metabolic pathways that become dysregulated during energy restriction
Temporal dynamics of metabolic response matter—timing of meals and fasting periods affects outcomes
Metabolic flexibility is compromised in obesity, making adaptation more difficult
For patients, this research explains why individuals with obesity may experience more pronounced hunger signals, metabolic slowdown, and difficulty with weight maintenance. The liver plays a central role in glucose metabolism, lipid metabolism, and energy homeostasis—all critical factors in weight regulation.
Measuring Metabolic Adaptation: The Prediction Equation Problem
Tang et al. (2025) addressed a methodological concern that has plagued obesity research: how we measure metabolic adaptation matters significantly.
Key Points from the Tang Analysis:
Different prediction equations for calculating expected metabolic rate yield conflicting results
Metabolic adaptation measurements can fluctuate by 100-300 calories depending on the equation used
This explains inconsistencies across different weight loss studies
The study analyzed data from a weight-loss clinical trial to demonstrate these discrepancies
Researchers need standardized methods to accurately assess adaptive thermogenesis
This is crucial for both researchers and practitioners. When your healthcare provider assesses your metabolic rate, the calculation method significantly impacts treatment recommendations. The study suggests that apparent "metabolic adaptation" might sometimes be a measurement artifact rather than a true biological phenomenon.
The Comprehensive Picture: Latest Insights on Weight Regain Physiology
Van Baak and Mariman (2025) published an authoritative review in Current Obesity Reports synthesizing the latest understanding of weight regain physiology.
Major Takeaways from the van Baak & Mariman Review:
Metabolic adaptation includes decreased energy expenditure (typically 50-100 calories below predicted)
Hormonal changes persist long after weight loss, including elevated ghrelin (hunger hormone) and decreased leptin (satiety hormone)
Appetite regulation becomes dysregulated, with increased hunger and reduced fullness signals
Neuroendocrine responses create a biological pressure to regain weight
The body defends a set point weight range through multiple compensatory mechanisms
This review emphasizes that weight regain isn't about personal failure—it's about biology. The body perceives weight loss as a threat and activates multiple systems to restore lost weight, including changes in thyroid hormones, cortisol levels, and sympathetic nervous system activity.
Metabolic Adaptations: A Brief Historical Context
Martínez-Gómez and Roberts (2022) provided an essential foundation in the Journal of Strength and Conditioning Research, reviewing metabolic adaptations specifically relevant to athletes and physically active individuals.
Highlights from the Martínez-Gómez & Roberts Study:
Resting metabolic rate decreases by 5-15% beyond what's predicted by body composition changes
Thermic effect of food (calories burned during digestion) may decrease after weight loss
Exercise efficiency improves—meaning you burn fewer calories doing the same activity
Muscle protein synthesis rates may be affected during prolonged calorie restriction
Resistance training helps preserve metabolic rate during weight loss
For individuals combining exercise with dietary restriction, this research provides actionable insights. Maintaining lean muscle mass through resistance training helps counteract some metabolic adaptation, though it doesn't eliminate it entirely.
Metabolic Consequences: The Complete Picture
Farhana and Rehman (2025) offer a comprehensive overview in StatPearls, covering the full spectrum of metabolic consequences of weight reduction.
Essential Points from the Farhana & Rehman Review:
Weight loss triggers both beneficial and challenging metabolic changes
Positive effects include improved insulin sensitivity, reduced inflammation, and better lipid profiles
Negative adaptations include decreased metabolic rate, increased hunger, and reduced energy expenditure
Body composition changes influence metabolic outcomes—preserving muscle matters
Individual variability is substantial—genetic, environmental, and behavioral factors all play roles
This balanced perspective reminds us that while metabolic adaptation makes maintenance challenging, weight loss still provides significant health benefits including reduced risk of type 2 diabetes, cardiovascular disease, and certain cancers.
What This Means for Your Weight Management Journey
The Biology of Weight Regain
Your body doesn't understand that you're trying to improve your health through weight loss. From an evolutionary perspective, losing weight signals potential starvation, triggering powerful biological mechanisms designed to restore energy stores:
Reduced metabolic rate: Your body burns fewer calories at rest and during activity
Hormonal shifts: Hunger hormones increase while satiety hormones decrease
Enhanced nutrient absorption: Your digestive system becomes more efficient at extracting calories
Increased appetite: Neural signals amplify food reward and seeking behaviors
Decreased spontaneous activity: You naturally move less without realizing it
Practical Strategies Based on Current Science
1. Consider Long-Term Medication Use
The West et al. (2026) study suggests that weight management medications may need to be continued indefinitely for many patients. Discuss with your healthcare provider whether long-term pharmacotherapy is appropriate for your situation.
2. Prioritize Protein and Resistance Training
Multiple studies confirm that maintaining lean muscle mass helps preserve metabolic rate. Aim for:
0.7-1.0 grams of protein per pound of body weight daily
Resistance training 2-4 times weekly
Progressive overload to continuously challenge muscles
3. Focus on Metabolic Flexibility
The Ravussin et al. (2025) findings on enhanced fat oxidation suggest strategies that improve metabolic flexibility:
Intermittent fasting (with medical supervision)
Low-carbohydrate periods alternated with higher-carb refeeds
Regular physical activity to enhance mitochondrial function
4. Monitor Your Individual Response
Given the Tang et al. (2025) findings on measurement variability, work with professionals who use consistent, validated methods to track your metabolic rate and progress over time.
5. Plan for Maintenance from Day One
The van Baak and Mariman (2025) review emphasizes that weight maintenance requires different strategies than weight loss. Begin developing maintenance habits during the weight loss phase rather than treating maintenance as an afterthought.
6. Address the Psychological Component
Understanding that weight regain has biological drivers can reduce shame and self-blame. Work with professionals who recognize that maintaining weight loss requires ongoing support and potentially behavioral interventions alongside physiological strategies.
The Future of Weight Management
These 2025 studies collectively point toward a paradigm shift in how we approach obesity treatment and weight maintenance:
Personalized Medicine: Future treatments will likely account for individual metabolic responses, genetic profiles, and metabolic adaptation patterns.
Combination Approaches: The most effective strategies will probably combine medications (like tirzepatide or other GLP-1 agonists), behavioral support, nutritional interventions, and exercise programming.
Chronic Disease Management Model: Like diabetes or hypertension, obesity increasingly requires long-term management rather than short-term "cures."
Metabolic Health Focus: Success metrics may shift from pure weight loss to improved metabolic health markers including insulin sensitivity, inflammatory markers, and cardiovascular risk factors.
Key Takeaways
✓ Weight regain after medication cessation is common and biologically driven—typically 30-70% of lost weight returns within 12 months (West et al., 2026)
✓ Tirzepatide preserves metabolic function better than traditional dieting, particularly by enhancing fat oxidation without triggering severe metabolic adaptation (Ravussin et al., 2025)
✓ Liver metabolism plays a crucial but often overlooked role in weight regulation, with differences between healthy and obese metabolic networks (Morita et al., 2025)
✓ How we measure metabolic adaptation matters—different equations can show vastly different results, affecting treatment recommendations (Tang et al., 2025)
✓ Multiple biological systems work together to promote weight regain, including hormonal changes, reduced metabolic rate, and altered appetite signals (van Baak & Mariman, 2025)
✓ Resistance training and protein intake help preserve metabolic rate during and after weight loss (Martínez-Gómez & Roberts, 2022)
✓ Weight loss provides significant health benefits despite metabolic adaptation challenges, including improved insulin sensitivity and reduced disease risk (Farhana & Rehman, 2025)
Frequently Asked Questions
Q: Is my metabolism permanently damaged after weight loss?
A: No. While metabolic adaptation does occur and can persist, it's not permanent damage. Your metabolism adjusts based on current circumstances. With proper nutrition, exercise, and potentially medication support, you can work with these adaptations rather than against them.
Q: Will I always have to take medication to maintain weight loss?
A: Current evidence suggests many people may benefit from long-term pharmacotherapy for obesity, similar to other chronic conditions. However, individual needs vary. Some people successfully maintain losses through lifestyle changes alone, while others benefit from ongoing medication support. The West et al. (2026) study highlights this is an individual decision best made with your healthcare team.
Q: How many calories does metabolic adaptation actually cost me?
A: Research shows adaptive thermogenesis typically reduces your metabolic rate by 50-150 calories per day beyond what's predicted by your new body weight. However, the Tang et al. (2025) study shows this number can vary significantly based on how it's measured. The practical impact is that you may need to eat slightly less (or move slightly more) than calculators predict for your current weight.
Q: Can exercise prevent metabolic adaptation?
A: Exercise, particularly resistance training, helps minimize but doesn't eliminate metabolic adaptation. The Martínez-Gómez and Roberts (2022) study shows that maintaining muscle mass through strength training preserves more metabolic rate than cardio alone or no exercise. However, exercise adaptations also occur—you become more efficient and burn fewer calories doing the same activities over time.
Q: Why do I feel hungrier after losing weight?
A: The van Baak and Mariman (2025) review explains that hormonal changes after weight loss increase ghrelin (hunger hormone) and decrease leptin (satiety hormone). Your brain receives signals that you're in an energy deficit state, triggering increased appetite and food-seeking behavior. This is biology, not willpower failure.
Q: Are newer medications like tirzepatide better for preventing regain?
A: The Ravussin et al. (2025) study suggests tirzepatide may preserve metabolic function better than traditional calorie restriction, particularly by enhancing fat burning. However, the West et al. (2026) research shows that stopping any weight loss medication typically leads to regain. The medications appear effective during use, but long-term continuation may be necessary.
Q: What's the single most important thing I can do to maintain weight loss?
A: There's no single magic bullet, but research consistently emphasizes ongoing monitoring and support. The combination of continued behavioral strategies, possible pharmacotherapy, protein-rich nutrition, resistance exercise, and regular follow-up with healthcare providers shows the best outcomes. Weight maintenance requires permanent lifestyle adaptation rather than temporary changes.
Take Action: Your Next Steps
If you're struggling with weight maintenance or concerned about metabolic adaptation, here's what you can do today:
1. Schedule a Comprehensive Assessment: Work with a healthcare provider who understands current obesity medicine. Ask about having your resting metabolic rate measured and discuss whether medications like tirzepatide or other GLP-1 receptor agonists might be appropriate.
2. Build Your Support Team: Consider working with a registered dietitian specializing in weight management, a personal trainer focused on resistance training, and a therapist experienced in health behavior change.
3. Track Meaningfully: Monitor not just weight but also body composition, energy levels, hunger patterns, and metabolic health markers like fasting glucose and lipid panels.
4. Educate Yourself Further: Understanding the science behind weight regain empowers better decision-making. Consider joining support groups where evidence-based approaches are emphasized.
5. Practice Self-Compassion: Recognize that weight regain often reflects biology rather than personal failure. The latest science validates that maintaining weight loss is genuinely difficult due to powerful physiological mechanisms.
6. Think Long-Term: Shift from a "diet mindset" to a chronic disease management approach. What can you sustain for years rather than months?
Author’s Note
As clinicians, we often watch patients blame themselves for weight regain, unaware that powerful biological forces—not a lack of effort—drive this process. The emerging evidence from 2025–2026 makes one message overwhelmingly clear: weight regain is a physiological response, not a personal failure. The studies summarized here—ranging from metabolic adaptation research to analyses of medication cessation—show that the body defends its fat stores with remarkable persistence.
My goal in writing this article is to shift the narrative from shame to science. Understanding how hormones, metabolism, appetite signaling, and neural pathways change during and after weight loss empowers patients and healthcare practitioners to make informed decisions. Whether through long-term pharmacotherapy, resistance training, protein optimization, or personalized metabolic monitoring, successful weight maintenance requires a strategic, individualized, and sustained approach.
Obesity is a chronic, relapsing, multifactorial disease, not a short-term problem. I hope this article helps you view your journey with more compassion and equips you with the scientific clarity needed to work with your biology rather than against it.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Always consult qualified healthcare professionals before making changes to your weight management approach, starting medications, or modifying exercise routines.
Related Articles
Why Obesity is a Disease, Not a Lifestyle Choice: Latest Evidence-Based Insights | DR T S DIDWAL
How Insulin Resistance Accelerates Cardiovascular Aging | DR T S DIDWAL
Physical Activity, Adiposity, and Metabolic Health: What Science Reveals | DR T S DIDWAL
HIIT Benefits: Evidence for Weight Loss, Heart Health, & Mental Well-Being | DR T S DIDWAL
References
Farhana, A., & Rehman, A. (2025). Metabolic consequences of weight reduction. In StatPearls [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK572145/
Martínez-Gómez, M. G., & Roberts, B. M. (2022). Metabolic adaptations to weight loss: A brief review. Journal of Strength and Conditioning Research, 36(10), 2970–2981. https://doi.org/10.1519/JSC.0000000000003991
Morita, K., Hatano, A., Kokaji, T., Sugimoto, H., Tsuchiya, T., Ozaki, H., Egami, R., Li, D., Terakawa, A., Ohno, S., Inoue, H., Inaba, Y., Suzuki, Y., Matsumoto, M., Takahashi, M., Izumi, Y., Bamba, T., Hirayama, A., Soga, T., & Kuroda, S. (2025). Structural robustness and temporal vulnerability of the starvation-responsive metabolic network in healthy and obese mouse liver. Science Signaling, 18(883), eads2547. https://doi.org/10.1126/scisignal.ads2547
Ravussin, E., Sanchez-Delgado, G., Martin, C. K., Beyl, R. A., Greenway, F. L., O'Farrell, L. S., Roell, W. C., Qian, H. R., Li, J., Nishiyama, H., Haupt, A., Pratt, E. J., Urva, S., Milicevic, Z., & Coskun, T. (2025). Tirzepatide did not impact metabolic adaptation in people with obesity, but increased fat oxidation. Cell Metabolism, 37(5), 1060–1074.e4. https://doi.org/10.1016/j.cmet.2025.03.011
Tang, M., Wang, J., Xiang, Y., & Xu, R. (2025). Metabolic adaptation fluctuates with different prediction equations: A secondary analysis based on a weight-loss clinical trial. Frontiers in Nutrition, 12, Article 1543263. https://doi.org/10.3389/fnut.2025.1543263
van Baak, M. A., & Mariman, E. C. (2025). Physiology of weight regain after weight loss: Latest insights. Current Obesity Reports, 14, 28. https://doi.org/10.1007/s13679-025-00619-x
West, S., Scragg, J., Aveyard, P., Oke, J., Willis, L., Haffner, S., & Knight, H. (2026). Weight regain after cessation of medication for weight management: Systematic review and meta-analysis. BMJ, 392, e085304. https://doi.org/10.1136/bmj-2025-085304