Testosterone Therapy for Sarcopenia: A Comprehensive Evidence-Based Guide
"Explore evidence-based insights on testosterone therapy for sarcopenia, including mechanisms, clinical trials, lifestyle synergy, and personalized treatment strategie
SARCOPENIA
DR T S DIDWAL MD
11/18/202513 min read
What if the secret to keeping your muscles strong as you age isn’t just lifting weights, but also optimizing the very hormones that tell your muscles to grow? Testosterone isn’t just a male sex hormone—it’s a molecular conductor orchestrating muscle repair, strength, and metabolism. Understanding its role could be the difference between healthy aging and frailty
Clinical Pearls
Patient Selection is Critical: Testosterone therapy benefits primarily men with documented hypogonadism (total testosterone <300 ng/dL) and sarcopenia; routine use in eugonadal men is not recommended.
Lifestyle Synergy Matters: Exercise, especially resistance training, and adequate protein intake enhance testosterone’s muscle-building effects; therapy alone is insufficient.
Molecular Impact: Testosterone alters gene expression in muscle tissue, promoting protein synthesis and reducing inflammation, providing a mechanistic basis for functional improvements.
Monitor for Risks: Cardiovascular events, polycythemia, prostate issues, and sleep apnea require regular medical supervision during therapy.
Integrated Approach is Key: Combining lifestyle interventions, personalized hormone evaluation, and careful monitoring produces the best outcomes for sarcopenia management.
Understanding Sarcopenia: More Than Just Aging Muscles
Before we explore testosterone's role, let's establish what we're dealing with. Sarcopenia isn't just about losing muscle mass—it's a multifaceted condition that involves decreased muscle strength, reduced physical performance, and ultimately, a loss of independence. Think of it as your muscles going into early retirement without your permission.
The condition affects approximately 10% of adults over 60, though this number climbs significantly higher in those over 80. Beyond the obvious physical limitations, sarcopenia increases fall risk, impairs metabolic health, and diminishes quality of life. It's particularly concerning because it often occurs alongside other chronic conditions, creating a perfect storm of health challenges.
The Testosterone-Muscle Connection: Understanding the Biology
1. Introduction: Why Testosterone Matters in Muscle Aging
Age-associated testosterone decline (1–2%/year after 30)
Link to muscle mass, strength, power, and physical performance
Sarcopenia as partly a “hormonal deficiency state”
2. Physiology of Testosterone in Skeletal Muscle
Testosterone → androgen receptor → anabolic signaling
Activation of satellite cells
Upregulation of mTOR/PI3K–Akt pathway
Effects on mitochondrial biogenesis
Anti-catabolic effects (reduces ubiquitin–proteasome pathway)
Influence on Type I and Type II muscle fibers
Testosterone + exercise synergy
3. Age-Related Testosterone Decline and Sarcopenia Pathophysiology
Decline in total T, free T, bioavailable T
Rising SHBG with age → reduced hormonal action at tissue level
Interaction with inflammation, insulin resistance, and frailty
Why “normal ranges” may not reflect functional deficiency in older adults
What the Latest Research Tells Us: A Study-by-Study Breakdown
Study 1: Testosterone as a Function-Promoting Therapy
Main Focus: This review by Dos Santos & Storer, 2022 examines testosterone therapy as a treatment strategy for sarcopenia in aging men and those with chronic diseases.
Key Findings:
Testosterone's Role: Testosterone deficiency contributes significantly to muscle loss in aging men and patients with chronic conditions like HIV, cancer, and chronic kidney disease
Treatment Benefits: Testosterone replacement therapy (TRT) has been shown to:
Increase lean muscle mass
Improve muscle strength
Enhance physical function and mobility
Potentially improve the quality of life
Mechanism: Testosterone promotes muscle protein synthesis, increases muscle fiber size, and may reduce inflammation that contributes to muscle wasting
Important Considerations:
Benefits are most pronounced when combined with resistance exercise
Not all men with sarcopenia have low testosterone
Treatment requires careful patient selection and monitoring
Potential cardiovascular and prostate-related risks need evaluation
Clinical Relevance: The authors suggest testosterone therapy should be considered as part of a comprehensive approach to sarcopenia management, particularly in hypogonadal men, but emphasize the need for individualized treatment decisions based on risk-benefit analysis.
Study 2: The Molecular Story—How Testosterone Changes Muscle at the Genetic Level
The 2025 groundbreaking study by Viola and colleagues took us inside the muscle cells themselves, examining how testosterone modulates the muscle transcriptomic profile during lifestyle therapy in older men with obesity and hypogonadism (Viola et al., 2025). Translation? They looked at which genes get turned on or off when testosterone is combined with lifestyle changes.
This study enrolled older men (ages 65 and above) with both obesity and clinically confirmed hypogonadism. Participants received either testosterone therapy or a placebo while all engaged in a comprehensive lifestyle intervention including diet and exercise.
Key Findings:
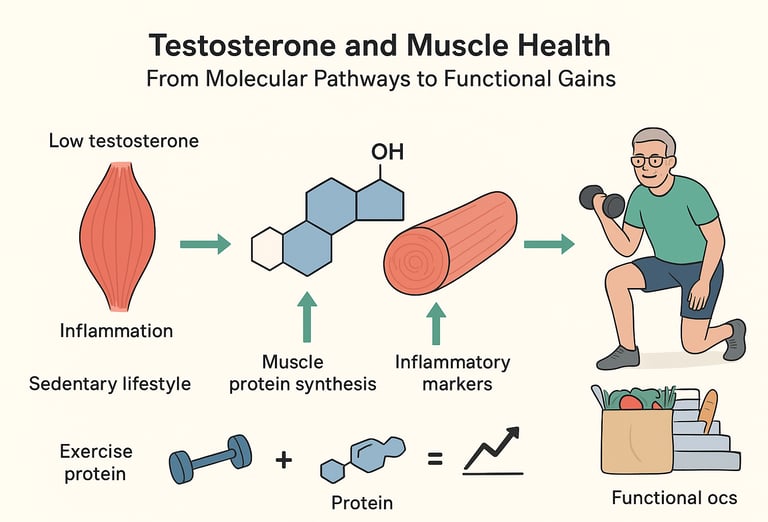
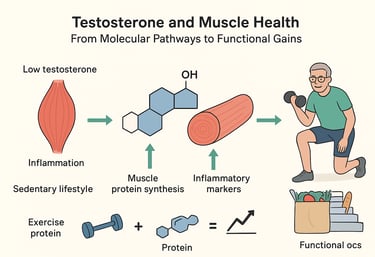
Testosterone fundamentally altered gene expression patterns in muscle tissue, affecting pathways involved in muscle growth, metabolism, and inflammation
The combination of testosterone therapy with lifestyle modifications produced superior results compared to lifestyle changes alone
Molecular changes included upregulation of genes associated with muscle protein synthesis and downregulation of inflammatory markers
The transcriptomic changes correlated with measurable improvements in muscle function
Key Takeaway: Testosterone doesn't work in isolation—it literally rewrites the molecular instruction manual your muscles follow. When combined with proper diet and exercise, it creates a synergistic effect at the cellular level. This study provides the "why" behind the clinical observations we see.
Study 3: The Sedentary Lifestyle Connection
Huang and colleagues (2025) took a different approach, examining how sedentary behavior relates to sarcopenia prevalence, with testosterone playing a mediating role alongside systematic inflammation and vitamin D levels. This nationwide cross-sectional study included thousands of participants, providing robust population-level data.
Key Findings:
A sedentary lifestyle was significantly associated with increased sarcopenia prevalence
Lower testosterone levels partially mediated this relationship—meaning that sitting too much appears to lower testosterone, which in turn contributes to muscle loss
Systematic inflammation and vitamin D deficiency also played mediating roles
The relationship formed a complex web: sedentary behavior → lower testosterone/higher inflammation/lower vitamin D → increased sarcopenia risk
Key Takeaway: Your couch is not your friend when it comes to maintaining testosterone and muscle mass. This study reinforces that physical activity isn't just about burning calories—it's about maintaining the hormonal and metabolic environment your muscles need to thrive. The good news? This is a modifiable risk factor.
Study 4: The Systematic Review—What Does All the Evidence Say?
When you want to know what the scientific consensus is, you turn to systematic reviews and meta-analyses. Parahiba and colleagues (2020) conducted exactly this type of comprehensive analysis, examining the effect of testosterone supplementation on sarcopenic components in middle-aged and elderly men.
The researchers pooled data from multiple randomized controlled trials, analyzing outcomes including muscle mass, muscle strength, and physical performance.
Key Findings:
Testosterone supplementation significantly increased lean body mass in men with low testosterone levels
Improvements in muscle strength were observed, though the magnitude varied across studies
Physical performance measures showed modest improvements
The greatest benefits were seen in men with documented hypogonadism and lower baseline testosterone levels
Side effects were generally manageable but required monitoring
Key Takeaway: The meta-analysis confirms that testosterone can improve body composition and strength in the right candidates, but it's not a panacea. Patient selection matters enormously—not everyone with sarcopenia needs or will benefit from testosterone therapy.
Study 5: Life's Crucial 9 and the Testosterone Connection
The American Heart Association's Life's Essential 8 (recently updated to "Life's Crucial 9") provides a roadmap for cardiovascular health. You and Chen (2025) investigated whether these same factors relate to sarcopenia, with testosterone playing a mediating role.
Life's Crucial 9 includes: diet quality, physical activity, nicotine exposure, sleep health, body mass index, blood lipids, blood glucose, blood pressure, and cardiovascular health history.
Key Findings:
Better adherence to Life's Crucial 9 metrics was associated with lower sarcopenia prevalence
Testosterone levels partially mediated this relationship—meaning that healthier lifestyle factors appear to work partly through maintaining better testosterone levels
The protective effect against sarcopenia wasn't entirely explained by testosterone, suggesting multiple mechanisms at play
This reinforces that cardiovascular health and musculoskeletal health are intimately connected
Key Takeaway: The same lifestyle factors that protect your heart also protect your muscles, partly through maintaining healthier testosterone levels. This study beautifully illustrates how interconnected body systems are—you can't optimize one in isolation.
Study 6: The Current Treatment Landscape
Finally, McGuigan's 2025 perspective article provides crucial context on where we currently stand with sarcopenia treatment (McGuigan, 2025). While acknowledging the potential of emerging pharmacotherapies, including testosterone, the author emphasizes the primacy of exercise and dietary interventions.
Key Findings:
Exercise training, particularly resistance training, remains the gold standard treatment for sarcopenia
Nutritional optimization, especially adequate protein intake, is essential
While pharmacotherapies, including testosterone show promise, they should be considered adjunctive rather than primary treatments
The evidence base for exercise and nutrition is more robust and consistent than for any single pharmacological intervention
Key Takeaway: Don't put the pharmaceutical cart before the lifestyle horse. Exercise and proper nutrition must form the foundation of any sarcopenia treatment plan, with medications like testosterone considered as potential additions for appropriate candidates.
Who Might Benefit from Testosterone Therapy?
Based on the collective research, testosterone therapy for sarcopenia appears most beneficial for:
Men with confirmed hypogonadism (testosterone levels typically below 300 ng/dL)
Older adults with both low testosterone and sarcopenia
Patients with chronic diseases that contribute to both hormone deficiency and muscle loss
Individuals already engaged in exercise and proper nutrition who need additional support
Men with obesity-related hypogonadism, when combined with lifestyle interventions
Conversely, testosterone therapy is unlikely to help—and may carry unnecessary risks—for men with normal testosterone levels who have sarcopenia from other causes.
Clinical Context: Delivery Forms, Dosing Principles, and Monitoring in Hormone Therapy
Forms of Testosterone Delivery
Testosterone replacement can be administered through several pharmaceutical routes, each with its own pharmacokinetics and clinical considerations. These are the commonly used delivery forms in clinical practice:
Transdermal gels and creams:
Provide steady absorption through the skin, mimicking physiological secretion. They require daily application and carry a small risk of skin transfer to others.Transdermal patches:
Offer consistent serum levels but may cause local skin irritation in some patients.Intramuscular injections (short- or long-acting esters):
One of the most widely used forms. Short-acting esters create peaks and troughs, while long-acting formulations offer more stable levels.Subcutaneous pellets:
Implanted pellets offer long-duration, steady release (typically 3–6 months).Oral testosterone (limited use):
Some new formulations are available, but traditional oral testosterone (e.g., methyltestosterone) has hepatic considerations and is less commonly used.Buccal formulations:
Applied to the gum; less commonly used but avoid hepatic first-pass metabolism.
Each method differs in:
Stability of serum testosterone levels
Convenience
Cost
Side-effect profile
Monitoring intervals
General Dosing Principles: TRT
Without specifying any actual dosages, here are the scientific principles that clinicians use when adjusting therapy:
Aim for physiological replacement, not supraphysiological levels.
The target is to restore testosterone to a normal healthy range appropriate for age—not to exceed it.Start low and titrate based on laboratory parameters and clinical response.
TRT is typically individualized according to:Serum testosterone levels
SHBG
Free testosterone calculations
Symptom changes
Consider the pharmacokinetics of the delivery method.
For example, long-acting IM injections maintain stable levels, while short-acting ones may require dose adjustments to avoid peaks and troughs.Account for SHBG variability.
Men with high SHBG may require higher total testosterone levels to achieve adequate free testosterone.
The Exercise and Nutrition Foundation: Non-Negotiable First Steps
Let's be crystal clear: no amount of testosterone replacement therapy can compensate for a sedentary lifestyle and poor nutrition. The research consistently shows that:
Resistance Training is the single most effective intervention for sarcopenia. Progressive resistance exercise stimulates muscle protein synthesis, improves strength, and enhances functional capacity—all without the potential side effects of hormone therapy. Aim for 2-3 sessions per week targeting all major muscle groups.
Adequate Protein Intake is essential for maintaining and building muscle. Current recommendations suggest 1.2-1.5 grams of protein per kilogram of body weight daily for older adults, distributed across meals to optimize muscle protein synthesis. Think high-quality sources: lean meats, fish, eggs, dairy, legumes, and if needed, protein supplements.
Overall Diet Quality matters tremendously. The studies emphasize that following patterns like the Mediterranean diet—rich in fruits, vegetables, whole grains, healthy fats, and lean proteins—supports both healthy testosterone levels and muscle health through multiple mechanisms.
Physical Activity Beyond the Gym counts too. Breaking up sedentary time, incorporating walking, and staying generally active throughout the day all contribute to maintaining the hormonal and metabolic environment muscles need.
Understanding the Risks: What You Need to Know
Testosterone therapy isn't without potential downsides. Documented risks include:
Cardiovascular events: Some studies have raised concerns about increased risk of heart attack and stroke, though the evidence remains debated
Prostate health: Potential acceleration of prostate cancer growth (though not causation), necessitating regular monitoring
Polycythemia: Increased red blood cell production, which can thicken blood
Sleep apnea: Worsening of existing sleep-disordered breathing
Mood changes: Including increased aggression or mood swings in some individuals
Fertility effects: Suppression of sperm production
Skin reactions: Acne and oily skin at application sites
These risks underscore why testosterone therapy requires medical supervision with regular monitoring of testosterone levels, blood counts, lipid panels, and prostate-specific antigen (PSA).
The Personalized Medicine Approach
One size definitely doesn't fit all when it comes to treating sarcopenia. The research points toward a personalized approach that considers:
Individual Hormone Levels: Not just total testosterone, but also free testosterone and sex hormone-binding globulin (SHBG)
Underlying Health Conditions: Chronic diseases, obesity, metabolic syndrome, and other factors that might influence treatment decisions
Baseline Muscle Status: Severity of sarcopenia, strength deficits, and functional limitations
Lifestyle Factors: Current diet, exercise habits, sleep quality, and stress levels
Treatment Goals: Whether the priority is functional independence, athletic performance, or general health maintenance
Personal Risk Profile: Cardiovascular risk factors, prostate health, and other individual considerations
The most sophisticated approach involves using biomarkers beyond just testosterone—including inflammatory markers, vitamin D levels, and potentially even genetic factors—to guide treatment decisions.
Future Directions: What's on the Horizon?
The field of sarcopenia treatment is evolving rapidly. Emerging areas of investigation include:
Selective Androgen Receptor Modulators (SARMs): These compounds aim to provide testosterone's muscle-building benefits with fewer side effects, though they remain investigational.
Combination Therapies: Research is exploring optimal combinations of hormones, nutrients, and exercise protocols tailored to individual needs.
Precision Medicine Approaches: Using genetic testing and advanced biomarkers to predict who will respond best to different interventions.
Novel Delivery Methods: New testosterone formulations that provide more stable hormone levels with less frequent administration.
Targeting Molecular Pathways: Based on transcriptomic research like the Viola study, therapies might eventually target specific genetic pathways involved in muscle maintenance.
Frequently Asked Questions (FAQs)
Q: Can testosterone therapy reverse sarcopenia completely?
A: Not typically. While testosterone replacement therapy can improve muscle mass and strength in men with low testosterone, it works best as part of a comprehensive approach including exercise and nutrition. Complete reversal is rare, but significant functional improvements are possible.
Q: How long does it take to see results from testosterone therapy?
A: Most studies show measurable changes in body composition within 3-6 months, with continued improvements up to 12 months. However, functional improvements may become noticeable sooner—often within 6-8 weeks.
Q: Is testosterone therapy safe for older men?
A: It can be, but requires careful patient selection and monitoring. Men with certain cardiovascular conditions, untreated sleep apnea, or prostate cancer should not receive testosterone therapy. Regular medical supervision is essential.
Q: What testosterone level is considered "low" for sarcopenia treatment?
A: Generally, total testosterone below 300 ng/dL is considered low, though symptoms matter more than any single number. Some guidelines suggest considering treatment when levels are below 350 ng/dL with symptoms.
Q: Can women with sarcopenia benefit from testosterone therapy?
A: The research reviewed here focused on men. Women's testosterone physiology differs significantly, and while some studies suggest potential benefits, the evidence is less robust and requires careful consideration of side effects like virilization.
Q: Does exercise alone work as well as testosterone therapy?
A: For men with normal testosterone levels, exercise—particularly resistance training—may work equally well or better. For men with confirmed hypogonadism, the combination of exercise plus testosterone therapy typically produces superior results.
Q: What's the best type of testosterone therapy for sarcopenia?
A: Options include injections, gels, patches, and pellets. The research doesn't strongly favor one delivery method over others for muscle-building purposes. The choice often depends on patient preference, cost, and ability to maintain stable hormone levels.
Q: Can lifestyle changes alone increase testosterone naturally?
A: Yes, to some degree. Weight loss, resistance training, adequate sleep, stress management, and proper nutrition (especially sufficient vitamin D and healthy fats) can modestly increase testosterone levels naturally.
Your Next Steps: A Call to Action
If you're concerned about sarcopenia or wondering whether testosterone therapy might be right for you, here's what to do:
Get Properly Evaluated: Schedule a comprehensive assessment with your healthcare provider, including hormone testing, body composition analysis, and functional assessments. Don't self-diagnose or self-treat.
Optimize Your Lifestyle First: Before considering any pharmacological intervention, ensure you're doing the foundational work—resistance training 2-3 times weekly, consuming adequate protein (1.2-1.5 g/kg body weight), getting quality sleep, and managing stress.
Reduce Sedentary Time: Break up prolonged sitting, incorporate regular movement throughout your day, and aim for at least 150 minutes of moderate-intensity activity weekly.
Monitor Your Progress: Track not just weight or muscle size, but functional outcomes—can you climb stairs more easily? Carry groceries without difficulty? Maintain balance more confidently?
Have Informed Conversations: Discuss the evidence reviewed here with your healthcare team. Ask about potential benefits, risks, monitoring protocols, and whether you're an appropriate candidate for testosterone therapy.
Consider the Complete Picture: Remember that maintaining muscle health involves optimizing multiple factors—hormones, yes, but also inflammation control, vitamin D status, protein intake, resistance training, and overall metabolic health.
Stay Informed: The science of sarcopenia treatment is evolving rapidly. Stay connected with evidence-based resources and be willing to adjust your approach as new information emerges.
Conclusion: The Path Forward
Sarcopenia represents one of the most significant challenges of aging, affecting independence, quality of life, and overall health outcomes. The relationship between testosterone and muscle health is complex, nuanced, and highly individual. While testosterone therapy shows genuine promise for appropriately selected patients—particularly those with confirmed hypogonadism—it's not a universal solution.
The research reviewed here consistently points toward a comprehensive, personalized approach that prioritizes lifestyle interventions while judiciously incorporating pharmacological options when indicated. The molecular insights from transcriptomic studies reveal that testosterone's effects go far beyond simple muscle growth, fundamentally altering cellular programs in ways that support muscle health.
Perhaps most importantly, the evidence emphasizes that prevention is easier than reversal. Maintaining a physically active lifestyle, consuming adequate high-quality protein, managing body weight, and supporting overall metabolic health throughout adulthood may prevent or delay sarcopenia more effectively than any treatment can reverse it once established.
Whether you're a healthcare provider guiding treatment decisions or an individual navigating your own health journey, the message is clear: take sarcopenia seriously, address modifiable risk factors early, and approach treatment comprehensively rather than seeking single-solution magic bullets.
Your muscles have carried you through life—now it's time to carry them into healthy aging. The science shows us how, and the choice to act is yours.
About the Author: This article synthesizes current research on testosterone therapy for sarcopenia to provide evidence-based insights for healthcare professionals and patients. Always consult qualified healthcare providers before making treatment decisions.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Individual circumstances vary, and treatment decisions should always be made in consultation with qualified healthcare professionals.
Related Articles
Hormone Therapy and Sarcopenia: Testosterone, HGH, and Muscle Mass | DR T S DIDWAL
Vitamin D Deficiency and Sarcopenia: The Critical Connection | DR T S DIDWAL
How to Prevent Sarcopenia: Fight Age-Related Muscle Loss and Stay Strong | DR T S DIDWAL
Who Gets Sarcopenia? Key Risk Factors & High-Risk Groups Explained | DR T S DIDWAL
Sarcopenia: The Complete Guide to Age-Related Muscle Loss and How to Fight It | DR T S DIDWAL
Best Exercises for Sarcopenia: Strength Training Guide for Older Adults | DR T S DIDWAL
Best Supplements for Sarcopenia: Vitamin D, Creatine, and HMB Explained | DR T S DIDWAL
References
Dos Santos, M. R., & Storer, T. W. (2022). Testosterone treatment as a function-promoting therapy in sarcopenia associated with aging and chronic disease. Endocrinology and Metabolism Clinics of North America, 51(1), 187–204. https://doi.org/10.1016/j.ecl.2021.11.012
Huang, J., Li, Q., Dou, Y., Li, J., Liu, L., Xu, Y., Yang, N., & Jiang, Z. (2025). The association between sedentary lifestyle and the prevalence of sarcopenia with the mediation role of systematic inflammation index, 25-hydroxyvitamin D, and testosterone: A nationwide cross-sectional study. Clinical Nutrition ESPEN, 66, 530–538. https://doi.org/10.1016/j.clnesp.2025.02.022
McGuigan, A. (2025). Continue to treat sarcopenia with exercise and diet while potential pharmacotherapies are under investigation. Drugs & Therapy Perspectives, 41, 94–100. https://doi.org/10.1007/s40267-025-01141-9
Parahiba, S. M., Ribeiro, É. C. T., Corrêa, C., Bieger, P., Perry, I. S., & Souza, G. C. (2020). Effect of testosterone supplementation on sarcopenic components in middle-aged and elderly men: A systematic review and meta-analysis. Experimental Gerontology, 142, 111106. https://doi.org/10.1016/j.exger.2020.111106
Viola, V., Samanta, T., Nava, M. L. D., Celli, A., Armamento-Villareal, R., Nguyen, N. H. L., Colleluori, G., Barnouin, Y., Napoli, N., Qualls, C., Kaipparettu, B. A., & Villareal, D. T. (2025). Testosterone modulation of muscle transcriptomic profile during lifestyle therapy in older men with obesity and hypogonadism. Journal of Cachexia, Sarcopenia and Muscle, 16(1), e13697. https://doi.org/10.1002/jcsm.13697
You, B., & Chen, Z. (2025). Association between Life's Crucial 9 and sarcopenia: The mediating role of testosterone partially. Medicine, 104(37), e44569. https://doi.org/10.1097/MD.0000000000044569