How to Preserve Muscle During GLP-1 Weight Loss Therapy: Protein & Exercise Tips
GLP-1 weight loss therapy can reduce muscle mass. Discover evidence-based protein and exercise strategies to maintain lean muscle and strength
OBESITY
Dr. T.S. Didwal, M.D.(Internal Medicine)
1/31/202611 min read

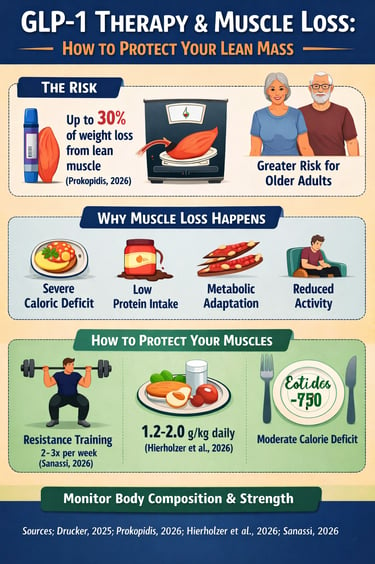
GLP-1 receptor agonists, including semaglutide and tirzepatide, have transformed the landscape of weight management and type 2 diabetes care, delivering unprecedented results in appetite suppression and rapid fat loss (Drucker, 2025). Millions of patients benefit from these medications, yet emerging research reveals a critical yet often overlooked consequence: significant lean muscle loss during aggressive weight reduction (Prokopidis, 2026). Studies indicate that up to 30% of total weight loss on GLP-1 therapy may come from lean muscle, a phenomenon that can compromise metabolic health, physical strength, and long-term functional capacity (Hierholzer et al., 2026).
Older adults are particularly vulnerable, experiencing disproportionate declines in muscle strength relative to younger populations, underscoring the need for age-specific monitoring strategies (Prokopidis, 2026). Fortunately, muscle loss is not inevitable. Evidence strongly supports integrating resistance training and optimized protein intake alongside GLP-1 therapy to preserve lean mass while achieving sustainable weight reduction (Sanassi, 2026). Emerging dual agonists combining GLP-1 and GIP receptor activity may offer modest improvements in muscle retention, but lifestyle interventions remain the dominant factor (Hierholzer et al., 2026).
Understanding the mechanisms behind GLP-1-induced muscle catabolism—including caloric restriction, reduced protein intake, and metabolic adaptation—enables patients and healthcare providers to implement targeted prevention strategies (Drucker, 2025; Prokopidis, 2026). By prioritizing resistance exercise, maintaining moderate caloric deficits, and monitoring body composition, individuals can achieve the dual goals of effective weight loss and muscle preservation. This knowledge is crucial for anyone considering GLP-1 therapy, ensuring metabolic health, functional strength, and long-term quality of life.
Clinical Pearls
1. Prioritize Protein Density Over Meal Volume
Why It Matters: GLP-1 medications reduce appetite, making it hard to eat large meals (Drucker, 2025).
Practical Tip: Focus on protein-rich foods first—chicken, fish, tofu, or Greek yogurt. Eating protein early ensures your muscles get the amino acids needed for repair and growth, even if you feel full quickly.
2. Track Strength, Not Just Weight
Why It Matters: Older adults may lose functional strength faster than total muscle mass (Prokopidis, 2026).
Practical Tip: Monitor your lifting performance or daily functional strength. Difficulty standing from a chair or carrying groceries signals muscle loss, even if the scale shows progress.
3. Use the Anabolic Window
Why It Matters: Post-workout nutrition enhances muscle protein synthesis during caloric deficits.
Practical Tip: Eat a protein-rich snack or meal within 90 minutes after exercise to maximize muscle repair and retention.
4. Treat Resistance Training as Metabolic Armor
Why It Matters: Lean mass drives your resting metabolic rate; losing muscle slows metabolism and risks weight regain.
Practical Tip: Incorporate 2–3 weekly resistance sessions with compound movements to protect your metabolic “engine.”
5. Slow and Steady Wins
Why It Matters: Rapid weight loss increases muscle breakdown.
Practical Tip: Aim for 1–2 pounds of weight loss per week to preserve lean mass and avoid catabolism.
6. Stay Hydrated for Muscle Function
Why It Matters: GLP-1s may reduce thirst cues, and dehydration impairs muscle contractility.
Practical Tip: Drink water consistently to support workouts, recovery, and muscle fullness.
Preserve Muscle While Losing Weight: The Hidden Challenge of GLP-1 Therapy
What Are GLP-1 Agonists and How Do They Work?
Glucagon-like peptide-1 (GLP-1) receptor agonists represent a breakthrough in obesity pharmacotherapy and type 2 diabetes treatment. These medications mimic the natural GLP-1 hormone, which regulates appetite, blood sugar, and metabolic rate.
According to Drucker (2025), in his comprehensive review published in Nature Reviews Drug Discovery, GLP-1-based therapies have expanded far beyond their initial diabetes applications to address obesity, cardiovascular disease, and emerging indications in neurological conditions. The therapeutic versatility of GLP-1 agonists stems from their multiple mechanisms of action, including appetite suppression, increased satiety, improved insulin sensitivity, and cardiovascular protection.
Key Mechanisms of GLP-1 Action:
Appetite regulation through central nervous system signaling, gastric emptying delays that prolong satiety, blood sugar optimization via enhanced pancreatic beta-cell function, and weight reduction through decreased caloric intake. However, this potent appetite suppression comes with a potential cost: users may struggle to consume adequate dietary protein, leading to unintended muscle catabolism.
The Muscle Loss Problem: What Recent Research Reveals
Study 1: Prokopidis (2026) – Muscle Strength Changes Beyond Mass Reductions
Prokopidis, K. (2026) published groundbreaking research in the British Journal of Pharmacology examining glucagon-like peptide-1 receptor agonists and their effects on muscle strength in older adults—a particularly vulnerable population.
The research highlighted that muscle strength loss extends beyond simple muscle mass reduction. Older adults using GLP-1 agonists experienced disproportionate strength decrements compared to younger populations, suggesting age-dependent vulnerabilities in muscle quality and contractile function. This distinction is critical: you can maintain body weight while losing functional muscle power, creating metabolic vulnerability and fall risk in aging populations.
Key Takeaway:
GLP-1 therapy poses greater risk for muscle strength decline in older adults than in younger patients, requiring age-stratified monitoring and intervention strategies. The decline in muscle quality—not just quantity—affects functional capacity and independence.
Study 2: Hierholzer, Benson, Ewida, & Ahmed (2026) – Pipeline Solutions and Limitations
Hierholzer et al. (2026) conducted an in-depth analysis published in Biochimica et Biophysica Acta – Molecular Basis of Disease, specifically examining mitigation strategies for lean muscle loss associated with GLP-1 and dual GLP-1/GIP agonists.
The research identified both pharmaceutical approaches in development and practical limitations of current interventions:
• Emerging pharmaceutical solutions include targeted anabolic agents, myostatin inhibitors, and combination therapies designed to preserve lean mass during GLP-1 therapy
• Current limitations of single-agent approaches mean standalone GLP-1 medications cannot fully prevent muscle atrophy without lifestyle modifications
• Dual agonists (combining GLP-1 and GIP receptor signaling) show modest improvements in muscle preservation compared to GLP-1-only medications, though the advantage remains incomplete
• Pipeline opportunities suggest future medications may specifically target muscle metabolism while maintaining weight loss efficacy
Key Takeaway:
Pharmaceutical solutions alone cannot fully mitigate GLP-1-induced muscle loss. A multimodal approach combining medications, resistance training, and protein optimization remains the gold standard until next-generation muscle-sparing GLP-1 agonists reach the market.
Study 3: Sanassi (2026) – Weight Training as a Cornerstone of GLP-1 Therapy
Lorraine A. Sanassi (2026) published practical clinical guidance in Clinical Advisor, specifically addressing the integration of weight training with GLP-1 therapy for optimal weight management.
The research demonstrated that resistance exercise serves as the most effective muscle-sparing intervention currently available for patients on GLP-1 agonists:
Progressive resistance training (2-3 sessions weekly) preserves lean mass during GLP-1-induced weight loss, with effects comparable to or exceeding pharmaceutical interventions
Protein intake optimization (1.2-2.0 grams per kilogram of body weight daily) combined with strength training creates a synergistic muscle-preservation effect
Exercise timing matters: resistance training performed during active GLP-1 therapy shows superior muscle retention compared to post-therapy initiation
Compound movements (squats, deadlifts, bench press) produce greater hormonal responses and muscle growth signals than isolation exercises
Key Takeaway:
Weight training is not optional for GLP-1 users—it's essential. The combination of resistance exercise and adequate protein consumption should be considered standard of care for any patient initiating GLP-1 therapy, particularly those at risk for sarcopenia or over age 40.
Study 4: Drucker (2025) – Comprehensive Understanding of GLP-1 Pharmacology and Future Applications
Drucker, D.J. (2025) published an authoritative review in Nature Reviews Drug Discovery, contextualizing GLP-1-based therapies within the broader landscape of modern pharmacotherapy.
Key Findings
The comprehensive review positioned GLP-1 agonists as transformative agents while acknowledging metabolic trade-offs:
GLP-1 receptor activation produces weight loss through multiple mechanisms, but inherently conflicts with muscle protein preservation when caloric deficit is severe
Metabolism optimization during GLP-1 therapy requires conscious attention to lean mass preservation, not passive assumption of weight loss quality
Future generations of GLP-1 analogs aim to decouple weight loss efficacy from muscle loss, potentially through selective tissue signaling
Patient education about nutritional needs and exercise requirements during GLP-1 therapy remains critically inadequate despite growing clinical experience
Key Takeaway:
Understanding GLP-1 pharmacodynamics reveals that muscle loss is not an unavoidable side effect—it's a consequence of poor implementation. Thoughtful patient management combining medical therapy, exercise prescription, and nutritional optimization can preserve metabolic health while achieving sustainable weight loss.
Understanding the Mechanism: Why GLP-1s Cause Muscle Loss
The muscle loss associated with GLP-1 agonists stems from several interconnected mechanisms
Severe Caloric Restriction
GLP-1 medications reduce hunger dramatically, often creating caloric deficits exceeding 30-40% of baseline intake. While effective for rapid weight loss, aggressive energy restriction triggers muscle catabolism as your body seeks protein sources for essential functions.
Reduced Protein Intake
Decreased appetite often means protein consumption drops significantly. Since muscle synthesis requires adequate amino acids, insufficient dietary protein inevitably leads to net muscle loss, even with exercise.
Metabolic Adaptation
Your body responds to severe caloric deficit by downregulating muscle protein synthesis and upregulating protein breakdown, a survival mechanism that paradoxically accelerates lean mass loss.
Reduced Physical Activity
GLP-1-induced nausea and reduced energy sometimes discourage exercise. Without resistance training stimulus, your muscles lack the signal to adapt and grow, making atrophy inevitable.
Quantifying the Risk: What the Research Says About Muscle Loss Magnitude
The four studies collectively suggest that GLP-1 users may lose 25-35% of total weight loss as lean muscle tissue, versus the ideal of 15-20% for healthy weight reduction. For a patient losing 20 pounds, this translates to 5-7 pounds of lean mass—a significant amount affecting metabolic rate, strength, and functional capacity.
Prokopidis (2026) emphasized that older adults experience even greater proportional muscle loss, sometimes approaching 40% of weight reduction, making this population particularly vulnerable.
The GIP Advantage: How Dual-Agonists Protect the Musculoskeletal Framework
While GLP-1 handles the heavy lifting for appetite suppression, the GIP (Glucose-dependent Insulinotropic Polypeptide) component in dual agonists like tirzepatide acts as a metabolic "buffer" that may better protect lean tissue through three specific pathways:
Adipose Tissue Blood Flow: GIP increases blood flow to fat stores and enhances lipid storage capacity in subcutaneous fat. By making fat metabolism more "flexible" and efficient, the body may rely less on breaking down muscle protein for emergency energy during a caloric deficit.
Bone Health Preservation: Emerging evidence suggests GIP has a bone-protective (osteogenic) effect. By maintaining bone mineral density—which is mechanically linked to muscle attachment—GIP helps preserve the overall integrity of the musculoskeletal system.
Glucagon Synergism: Unlike standalone GLP-1, GIP may help modulate the glucagon response, potentially creating a more "anabolic-friendly" hormonal environment that favors fat oxidation over muscle catabolism.
In short: GIP helps ensure the weight you lose comes from the "right" places (fat) while providing a supportive environment for the "good" places (bone and muscle).
Proven Strategies to Preserve Muscle During GLP-1 Therapy
Based on the comprehensive research evidence, here are evidence-backed strategies to maintain lean mass while using GLP-1 agonists:
Strategy 1: Prioritize Resistance Training (Essential)
Sanassi (2026) makes clear that resistance exercise is non-negotiable. Implement:
Two to three sessions weekly of progressive resistance training
Compound movements targeting major muscle groups (legs, chest, back, core)
Progressive overload (gradually increasing weight or repetitions)
Adequate rest between sessions for muscle recovery
Strategy 2: Optimize Protein Intake (Critical)
Consume 1.2-2.0 grams of protein per kilogram of body weight daily:
For a 150-pound (68 kg) person: target 82-136 grams daily
Distribute protein intake across 3-4 meals for optimal muscle protein synthesis
Prioritize complete proteins containing all essential amino acids
Consider protein supplementation if whole-food intake falls short
Strategy 3: Maintain Moderate Caloric Deficit (Not Severe)
Rather than accepting the extreme appetite suppression that GLP-1s enable:
Target 500-750 calorie deficits instead of 1,500+ calorie deficits
This requires intentional eating despite decreased hunger
Moderate weight loss rates (1-2 pounds weekly) preserve more lean mass than rapid reduction
Strategy 4: Monitor Strength and Muscle Quality
Prokopidis (2026) highlights that muscle strength assessment should accompany weight monitoring:
Track lifting performance (can you maintain your strength benchmarks?)
Measure waist circumference (indicates visceral fat loss vs. lean mass loss)
Consider body composition testing (DEXA scan, bioelectrical impedance) quarterly
Include functional assessments (stair climbing speed, sit-to-stand time)
Strategy 5: Time Nutrition Around Exercise
Consume protein and carbohydrates within 2 hours of resistance training to maximize muscle protein synthesis:
Post-workout meal: 25-40 grams protein plus carbohydrates
Pre-workout nutrition: adequate fuel without causing nausea (problem-solve individual tolerance)
Frequently Asked Questions About GLP-1 and Muscle Loss
Q1: Will I definitely lose muscle on GLP-1 agonists?
A: Not necessarily. With intentional resistance training and adequate protein intake, you can minimize lean mass loss to acceptable levels (15-20% of total weight loss). Without intervention, muscle loss becomes problematic.
Q2: Is resistance training safe if I'm experiencing GLP-1 nausea?
A: Yes, but modify intensity. Low-intensity resistance training is safe and beneficial. Timing workouts when nausea is minimal helps. Consult your healthcare provider if nausea is severe.
Q3: How much protein do I really need while on GLP-1 agonists?
A: Aim for 1.2-2.0 grams per kilogram of body weight daily. This is higher than sedentary individuals require, supporting both muscle retention and muscle repair from exercise.
Q4: Can I just take protein powder without exercise?
A: No. Protein alone cannot prevent muscle loss; you need resistance exercise to create the stimulus for muscle retention. The combination is synergistic.
Q5: Are dual GLP-1/GIP agonists better for muscle preservation?
A: Moderately. Dual agonists preserve slightly more lean mass than GLP-1-only agents, but lifestyle factors (exercise and nutrition) remain the dominant determinant of muscle retention.
Q6: When should I start resistance training if I'm beginning GLP-1 therapy?
A: Ideally, before starting, or immediately upon initiation. Early implementation allows your body to build exercise stimulus while medication is stabilizing.
Q7: Does GLP-1 therapy affect testosterone or hormones that influence muscle?
A: Not directly, though rapid weight loss and caloric restriction can impact hormonal profiles. Resistance training itself helps optimize hormonal environment for muscle preservation.
Q8: What if I cannot tolerate resistance training due to GLP-1 side effects?
A: Lower-intensity resistance work is still beneficial. Alternatively, high-protein diet alone provides modest protection. Discuss medication dose adjustment or timing changes with your provider.
Q9: How do I know if I'm losing too much muscle?
A: Monitor strength—can you maintain your lifting performance? Track waist circumference separately from weight. Consider body composition testing (DEXA) every 12 weeks.
Q10: After I stop GLP-1 therapy, will my muscle come back?
A: Muscle can be regained with continued resistance training and adequate nutrition, but it takes time (typically 3-6 months for significant gains). Prevention is easier than recovery.
Key Takeaways: Essential Points to Remember
GLP-1 agonists are effective weight loss and diabetes medications, but lean muscle loss is a real and quantifiable risk affecting metabolic health and functional capacity.
Prokopidis (2026) shows that older adults face particular vulnerability to GLP-1-induced muscle strength decline, requiring age-aware monitoring.
Hierholzer et al. (2026) reveals that pharmaceutical solutions alone cannot fully prevent muscle loss—a multimodal approach remains essential.
Sanassi (2026) demonstrates that resistance training combined with optimized protein intake is the most effective currently available muscle preservation strategy during GLP-1 therapy.
Drucker (2025) contextualizes these findings within broader GLP-1 pharmacology, emphasizing that muscle loss results from poor implementation rather than medication inevitability.
Moderate caloric deficit, consistent resistance exercise, and adequate protein consumption form the foundation of sustainable weight loss with GLP-1 agonists.
Body composition monitoring (not just weight) should be standard care for GLP-1 patients.
Future pharmaceutical developments may improve muscle preservation, but current interventions rely on lifestyle modifications.
Conclusion: Muscle Loss is Preventable, Not Inevitable
GLP-1 receptor agonists represent genuine therapeutic advances for obesity and type 2 diabetes. The emerging research synthesis reveals that lean muscle loss during GLP-1 therapy is not an unavoidable medication side effect—it's a consequence of inadequate patient management.
The convergence of evidence from Prokopidis (2026) on strength vulnerability, Hierholzer et al. (2026) on pharmaceutical limitations, Sanassi (2026) on exercise efficacy, and Drucker (2025) on pharmacological context paints a clear picture: successful GLP-1 therapy requires intentional intervention combining exercise, nutrition, and medical management.
By understanding the mechanisms of GLP-1-induced muscle loss, implementing evidence-based prevention strategies, and monitoring body composition actively, you can achieve sustainable weight loss while preserving the lean muscle essential for metabolic health, functional capacity, and quality of life.
Your weight loss journey with GLP-1 agonists doesn't have to mean muscle loss. With knowledge, commitment, and professional support, you can optimize both weight reduction outcomes and metabolic health preservation.
Author’s Note
This article synthesizes the most recent peer-reviewed research (2025–2026) on GLP-1 receptor agonists, their effects on lean muscle mass, and clinically proven strategies for muscle preservation during weight management. The content aims to bridge the gap between pharmacological advances and lifestyle interventions, emphasizing resistance training, nutrition optimization, and patient-centred monitoring as essential components of effective therapy.
This work is intended for clinicians, researchers, and informed patients seeking a deeper understanding of the mechanistic and practical aspects of GLP-1 therapy. While the information presented reflects current scientific consensus, it is not a substitute for individualized medical advice. Readers are encouraged to consult their healthcare providers before making changes to medication, exercise, or dietary regimens.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Individual circumstances vary, and treatment decisions should always be made in consultation with qualified healthcare professionals.
Related Articles
Activate Your Brown Fat: A New Pathway to Longevity and Metabolic Health | DR T S DIDWAL
Leptin vs. Adiponectin: How Your Fat Hormones Control Weight and Metabolic Health | DR T S DIDWAL
Lower Blood Pressure Naturally: Evidence-Based Exercise Guide for Metabolic Syndrome | DR T S DIDWAL
References
Drucker, D. J. (2025). GLP-1-based therapies for diabetes, obesity and beyond. Nature Reviews Drug Discovery, 24, 631–650. https://doi.org/10.1038/s41573-025-01183-8
Hierholzer, J., Benson, H., Ewida, H. A., & Ahmed, M. S. (2026). Mitigating loss of lean muscle in GLP-1 and dual GLP-1/GIP agonists: Pipeline opportunities and limitations. Biochimica et Biophysica Acta (BBA) – Molecular Basis of Disease, 1872(4), 168172. https://doi.org/10.1016/j.bbadis.2026.168172
Prokopidis, K. (2026). Glucagon-like peptide-1 receptor agonists and muscle strength changes in older adults: Risks beyond muscle mass reductions. British Journal of Pharmacology, 183, 10.1111/bph.70355. Advance online publication. https://doi.org/10.1111/bph.70355
Sanassi, L. A. (2026, January 16). Pairing weight training with GLP-1 therapy for optimal weight management. Clinical Advisor. https://www.clinicaladvisor.com/features/weight-training-and-glp-1-therapy-for-optimal-weight-management/