High Cholesterol Isn’t Just LDL: The New Science of Heart Risk
High cholesterol treatment is changing in 2025. Learn why remnant cholesterol matters, how to manage statin intolerance, and what new guidelines mean for your heart health and longevity.
METABOLISM
Dr. T.S. Didwal, M.D.(Internal Medicine)
1/4/202610 min read
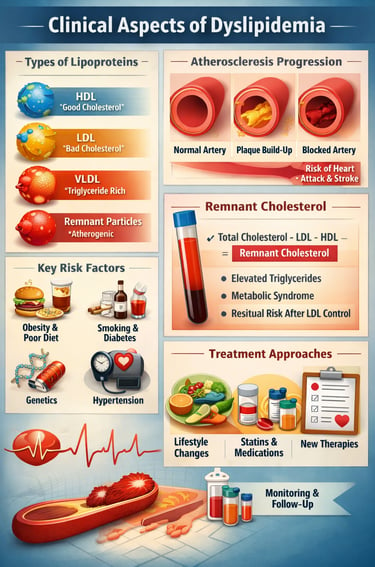

Dyslipidemia—an imbalance in blood lipids such as LDL-cholesterol, triglycerides, and HDL—remains a central driver of atherosclerotic cardiovascular disease (ASCVD) worldwide. While lowering LDL-cholesterol is still foundational, recent 2025 evidence highlights that many patients continue to face residual cardiovascular risk despite achieving LDL targets (Zuin & Bilato, 2025). This has shifted clinical focus toward a broader understanding of atherogenic dyslipidemia, including elevated triglycerides, low HDL, and particularly remnant cholesterol.
Remnant cholesterol, derived from triglyceride-rich lipoproteins, has emerged as an independent predictor of heart attack and stroke, especially in people with metabolic syndrome, type 2 diabetes, and obesity (Kamrani et al., 2025). Importantly, it can be calculated easily from a routine lipid panel, making it a practical tool for everyday clinical care.
Modern guidelines from the ESC/EAS and AACE now emphasise personalised lipid management, combining lifestyle measures with targeted pharmacotherapy, such as statins, ezetimibe, PCSK9 inhibitors, bempedoic acid, and newer RNA-based therapies, including inclisiran (Patel et al., 2025).
For patients, the key message is reassuring: cholesterol management is no longer “one-number-fits-all.” By addressing the entire lipid profile—not just LDL—clinicians can better reduce cardiovascular risk, improve long-term outcomes, and tailor therapy to individual needs.
Clinical pearls
1. Beyond the "Bad" Cholesterol: The Remnant Factor
While LDL is often called the "bad" cholesterol, it isn't the only villain. Remnant cholesterol—the leftovers from triglyceride-rich particles—is highly inflammatory and directly contributes to plaque buildup. Even if your LDL is at goal, high remnants can mean you are still at risk.
Pearl: If your triglycerides are high, your "residual risk" is likely high too. Calculate your remnants by subtracting your HDL and LDL from your Total Cholesterol.
2. The "Lower is Better" and "Earlier is Better" Rule
Atherosclerosis is a cumulative disease, much like sun damage to the skin. The 2025 guidelines emphasize that the duration of exposure to high cholesterol matters just as much as the level itself.
Pearl: Think of cholesterol management like a retirement fund: the earlier you start "investing" in low levels, the greater the compound interest in the form of a healthy heart later in life.
3. Statins are the Foundation, Not the Ceiling
Statins remain the "gold standard" because they stabilize existing plaques, making them less likely to rupture and cause a heart attack. However, we now know that many patients require a combination approach.
Pearl: Adding a second or third non-statin medication (like ezetimibe or a PCSK9 inhibitor) is not a sign of "failing" treatment; it is a precision strategy to hit targets that statins alone sometimes cannot reach.
4. Genetic Risk Isn’t a Guarantee, But It Is a Roadmap
With the rise of genetic testing in 2025, we can now identify patients with Familial Hypercholesterolemia (FH) or high Lipoprotein(a) levels. These conditions are "silent" and often don't respond to diet alone because the liver is genetically programmed to overproduce cholesterol.
Pearl: If you have a family history of early heart disease (before age 55 in men or 65 in women), ask for a Lipoprotein(a) test—it is a one-time genetic blood test that could change your entire treatment plan.
5. Metabolic Health and Lipids are Inseparable
Dyslipidemia rarely travels alone. It is often part of "Metabolic Syndrome," involving high blood sugar, belly fat, and high blood pressure. New 2025 therapies, such as GLP-1 receptor agonists, are showing that improving your body’s insulin use can have a "halo effect" on your lipid profile.
Pearl: Focus on "Functional Medicine"—improving your metabolic health through movement and fiber intake doesn't just lower numbers; it changes the actual quality and size of your cholesterol particles.
Modern Dyslipidemia Management: 2025 Guidelines & Recent Advances in Lipid-Lowering Therapy
1. Evolving Paradigms: The 2019 ESC/EAS Guidelines vs. 2025 Updates
Understanding the 2019 Foundation
The 2019 ESC/EAS dyslipidemia guidelines established LDL-cholesterol as the primary target for lipid-lowering therapy. They introduced risk stratification categories and recommended specific LDL targets based on cardiovascular risk profiles. This framework emphasized intensive statin therapy and, when necessary, additional lipid-lowering drugs.
What's Changed in 2025?
The 2025 focus update represents a meaningful evolution in clinical thinking. Rather than simply lowering one number, the updated approach considers:
Multiple lipid parameters beyond LDL-cholesterol
Individual patient factors including age, comorbidities, and treatment tolerance
Residual cardiovascular risk that remains despite LDL lowering
Novel biomarkers and their clinical significance
Real-world treatment challenges in achieving and maintaining targets
According to Zuin and Bilato (2025), these evolving paradigms recognize that LDL-cholesterol reduction, while essential, doesn't account for all atherogenic dyslipidemia patterns. The update encourages clinicians to view lipid management as a dynamic, patient-centred process rather than a rigid protocol.
Key Clinical Implications:
Reassess patients on statin therapy who remain at risk despite LDL control
Consider non-traditional lipid markers when standard targets are achieved
Adapt treatment based on individual responses and tolerability
Integrate lifestyle modifications with pharmacologic approaches more strategically
2. Remnant Cholesterol: The Rising Star in Cardiovascular Risk Assessment
What is Remnant Cholesterol?
Remnant cholesterol represents lipid particles that remain after triglyceride-rich lipoproteins release their triglycerides. These particles—including VLDL remnants and chylomicron remnants—carry cholesterol and contribute significantly to atherosclerosis development, yet they've historically received less clinical attention than LDL.
Why Should Clinicians Care?
Kamrani, Imannezhad, Rezaee, and colleagues (2025) conducted a comprehensive analysis comparing remnant cholesterol with low-density lipoprotein cholesterol in cardiovascular risk assessment. Their findings in Scientific Reports demonstrate that:
Remnant cholesterol shows superior predictive value for cardiovascular events in certain patient populations
Traditional LDL measurements may underestimate true atherogenic burden in patients with elevated triglycerides
Remnant lipoprotein particles demonstrate independent associations with atherosclerotic cardiovascular disease
Measuring remnant cholesterol could improve risk stratification accuracy
Clinical Significance
This research suggests a paradigm shift: clinicians should no longer ignore the triglyceride-rich remnant particles. For patients presenting with:
Elevated triglycerides despite statin therapy
Metabolic syndrome features
Persistent cardiovascular risk despite "controlled" LDL
...assessing remnant cholesterol levels may reveal hidden atherogenic risk requiring intensified treatment.
Remnant cholesterol can be calculated as: Total cholesterol − LDL-cholesterol − HDL-cholesterol. This simple calculation from standard lipid panels provides actionable information for risk assessment without requiring specialized testing.
3. AACE Clinical Practice Guideline: Comprehensive Pharmacologic Management for American Patients
Overview of the 2025 AACE Guideline
The American Association of Clinical Endocrinology released a comprehensive clinical practice guideline specifically addressing pharmacologic management of dyslipidemia in adults. Authored by Patel, Wyne, Afreen, and colleagues (2025), this guideline provides American practitioners with evidence-based recommendations tailored to the U.S. healthcare context.
Major Recommendations
The AACE guideline emphasizes:
Risk-Based Treatment Initiation: Decisions should reflect individual cardiovascular risk rather than arbitrary age cutoffs
Statin Therapy as Foundation: Statins remain first-line agents, with dosing intensified based on risk category
Non-Statin Agents Integration: Strategic use of ezetimibe, PCSK9 inhibitors, inclisiran, bempedoic acid, and other agents
Combination Therapy: Many patients benefit from multi-drug regimens addressing different lipid pathways
Special Populations: Distinct approaches for diabetes, chronic kidney disease, and other comorbidities
Drug Classes Highlighted
Statins (high-intensity options for maximum LDL reduction)
Ezetimibe (reduces intestinal cholesterol absorption)
PCSK9 inhibitors (dramatically lower LDL through receptor pathway enhancement)
Inclisiran (long-acting PCSK9 suppression via RNA interference)
Bempedoic acid (inhibits urate and lipid synthesis; particularly valuable for statin-intolerant patients)
GLP-1 receptor agonists (emerging evidence for lipid and cardiometabolic benefits)
Fibrates and ezetimibe combinations (triglyceride and remnant particle management)
Rather than sequential, step-wise therapy, the AACE approach advocates individualized combination regimens designed from treatment initiation, significantly improving the likelihood of achieving lipid targets and reducing cardiovascular event risk.
4. Global Evidence: Insights from Recent International Research
Chinese Population Study on Dyslipidemia and Cardiovascular Risk
Gao et al. (2025) published findings in the Zhonghua Liuxingbingxue Zazhi (Chinese Journal of Epidemiology) examining dyslipidemia prevalence and its cardiovascular correlates in Chinese populations. Their research contributes important data on:
Geographic and ethnic variations in lipid metabolism and disease patterns
How lifestyle factors influence lipid profiles differently across populations
Optimal LDL targets for diverse demographic groups
Public health implications for cardiovascular disease prevention
Key Takeaway: Lipid management strategies must account for ethnic and genetic diversity. One-size-fits-all targets may not serve all populations equally, supporting the move toward personalized medicine.
Systematic Review: Recent Advances in Dyslipidemia Management
Huang, et al.(2025) conducted a comprehensive systematic review published in Cureus, synthesizing recent advances across the dyslipidemia management landscape. This review identified:
Emerging pharmacotherapies with promising efficacy profiles
Combination strategy innovations that address multiple lipid abnormalities
Lifestyle intervention updates supported by recent evidence
Biomarker evolution beyond traditional lipid panels
Technology integration (digital health, genetic testing) in modern lipid management
Key Takeaway: The dyslipidemia management field is rapidly expanding with novel agents, refined strategies, and evidence-based approaches. Staying current with these advances is essential for optimizing patient outcomes.
5. Understanding Atherogenic Dyslipidemia and Residual Risk
Beyond LDL: The Bigger Picture
Even when LDL-cholesterol is optimally controlled with current medications, many patients continue experiencing cardiovascular events. This phenomenon—called residual cardiovascular risk—reflects the limitations of focusing exclusively on LDL reduction.
Atherogenic dyslipidemia patterns include:
Elevated triglycerides and triglyceride-rich lipoproteins
Reduced HDL-cholesterol
Increased remnant cholesterol particles
Small, dense LDL particles
High lipoprotein(a) levels
Recent research demonstrates that these non-traditional lipid markers independently predict atherosclerotic cardiovascular disease risk. Patients with "controlled" LDL but atherogenic dyslipidemia patterns remain vulnerable to events unless their complete lipid profile is addressed.
6. Personalized Approaches to Dyslipidemia Management
While guidelines provide essential frameworks, optimal dyslipidemia management increasingly requires individualization based on:
Patient Factors:
Genetic predisposition (familial hypercholesterolemia status)
Comorbidities (diabetes, metabolic syndrome, chronic kidney disease)
Medication tolerance (statin side effects, allergies)
Lifestyle capacity (ability to implement dietary/exercise modifications)
Age and life expectancy
Clinical Factors:
Baseline lipid profile characteristics
Rate of lipid changes on therapy
Presence of atherosclerotic disease
Other cardiovascular risk factors
Treatment goal achievement
The 2025 Precision Medicine Approach
Risk Stratification using validated tools
Lipid Panel Analysis assessing all relevant particles, not just LDL
Genetic Testing when familial conditions are suspected
Lifestyle Assessment and realistic goal-setting
Pharmacotherapy Selection matching agents to specific dyslipidemia patterns
Monitoring and Adjustment ensuring optimal tolerability and efficacy
7. Practical Clinical Scenarios
Scenario 1: The Statin-Tolerant Patient with Suboptimal Control
Patient Profile: 55-year-old on moderate-intensity statin with LDL of 95 mg/dL (goal <70), triglycerides 180 mg/dL, HDL 35 mg/dL
2025 Recommendation:
Intensify statin therapy
Add ezetimibe (reduces LDL further)
Consider fibrate or PCSK9 inhibitor depending on predominant risk pattern
Address remnant cholesterol directly through combination therapy
Expected Outcome: More comprehensive lipid control, reduced residual risk
Scenario 2: The Statin-Intolerant Patient
Patient Profile: 68-year-old with myalgia on all statins, LDL 180 mg/dL, high cardiovascular risk
2025 Recommendation:
Trial bempedoic acid (statins not required)
Add ezetimibe for additive LDL reduction
Consider inclisiran if additional lowering needed
Optimize with PCSK9 inhibitor if targets still not met
Expected Outcome: Effective LDL reduction without muscular side effects
Scenario 3: The Metabolic Syndrome Patient
Patient Profile: 52-year-old with diabetes, elevated triglycerides (280 mg/dL), low HDL, LDL 95 mg/dL
2025 Recommendation:
High-intensity statin baseline
Triglyceride-focused therapy with GLP-1 agonist (dual cardiometabolic benefit)
Consider fibrate if triglycerides remain elevated
Monitor remnant cholesterol specifically
Lifestyle modifications addressing insulin resistance
Expected Outcome: Comprehensive cardiometabolic risk reduction
8. Frequently Asked Questions
Q1: Should I Stop Taking My Statin if LDL is Controlled?
A: No. Statins provide benefits beyond LDL reduction, including anti-inflammatory effects and plaque stabilization. The 2025 guidelines recommend continuing statin therapy even at LDL goal, unless specific side effects occur requiring dosage adjustment.
Q2: What is Remnant Cholesterol, and Why Should I Care?
A: Remnant cholesterol consists of particles from triglyceride-rich lipoproteins. Recent research shows it predicts cardiovascular risk independently. If your triglycerides are elevated despite statin therapy, your remnant cholesterol may warrant attention and intensified treatment.
Q3: Are PCSK9 Inhibitors Right for Everyone?
A: No. PCSK9 inhibitors are most beneficial for patients with:
Familial hypercholesterolemia
Inadequate LDL control on statins
Very high cardiovascular risk
Statin intolerance requiring alternative agents
Cost and injection/infusion requirements also factor into decision-making.
Q4: How Often Should Lipid Panels Be Repeated?
A: Guidelines recommend:
Initial assessment: Baseline and 4-12 weeks after treatment changes
Maintenance: Annually for stable patients at goal
More frequent monitoring: If adjusting medications, assessing adherence, or targeting aggressive LDL levels
Q5: Can Lifestyle Changes Alone Control Dyslipidemia?
A: For mild dyslipidemia, lifestyle modifications (diet, exercise, weight loss, smoking cessation) may suffice. However, most patients with significant dyslipidemia require pharmacotherapy in addition to lifestyle measures. The 2025 approach emphasizes combining both strategies.
Q6: What's the Role of Genetic Testing in Dyslipidemia?
A: Genetic testing helps identify familial hypercholesterolemia and other inherited lipid disorders, enabling earlier, more aggressive treatment. It's particularly valuable in:
Young patients with very high LDL
Family histories of premature coronary disease
Guidance for relatives' screening
Q7: Are Newer Drugs Like Inclisiran and Bempedoic Acid Worth the Cost?
A: These agents offer specific advantages: inclisiran requires injections twice yearly (improved adherence), and bempedoic acid helps statin-intolerant patients. Cost-effectiveness depends on individual circumstances, insurance coverage, and treatment alternatives available.
9. The Bottom Line: What Patients and Providers Should Know
For Patients
Cholesterol management is individualized. Your lipid targets and medications should reflect your specific risk profile, not generic guidelines.
More than LDL matters. While LDL-cholesterol remains important, triglycerides, HDL, and remnant cholesterol also significantly influence cardiovascular risk.
Medication adherence is crucial. Taking your prescribed lipid-lowering medications consistently is essential—and often more important than dietary perfection.
Lifestyle modifications are complementary. Diet, exercise, and weight loss should accompany—not replace—prescribed medications for most patients.
Regular monitoring ensures optimal control. Periodic lipid panel checks confirm you're reaching targets and allow medication adjustments as needed.
For Healthcare Providers
Adopt 2025 guidelines flexibly. The ESC/EAS updates and AACE guideline provide frameworks, not rigid prescriptions. Individualize based on patient circumstances.
Assess remnant cholesterol. Calculate and interpret this simple yet underutilized metric to uncover hidden atherogenic risk.
Embrace combination therapy. Many patients benefit from multi-drug approaches addressing different lipid pathways rather than sequential monotherapy intensification.
Consider novel agents strategically. PCSK9 inhibitors, inclisiran, and bempedoic acid offer powerful options for patients achieving suboptimal control or experiencing statin intolerance.
Monitor beyond LDL-cholesterol. Assess triglycerides, HDL, Lipoprotein(a), and particle concentrations when available, especially in metabolic syndrome and diabetes.
Leverage lifestyle interventions. While pharmacotherapy is essential, comprehensive cardiovascular risk reduction requires integrated lifestyle counseling.
10. Looking Forward: The Future of Dyslipidemia Management
The 2025 research landscape suggests several emerging trends:
RNA interference therapies (like inclisiran) will expand treatment options with improved dosing schedules
Genetic risk stratification will increasingly guide treatment intensity selection
Lipoprotein(a) management will transition from risk marker to therapeutic target
GLP-1 receptor agonists will play expanding roles in dyslipidemia management, particularly for metabolic syndrome
Artificial intelligence may help predict individual treatment responses and optimize personalized regimens
Digital health tools will improve medication adherence and lipid monitoring accessibility
Author’s Note
Cholesterol management is no longer about chasing a single number. Advances in lipid science now show that cardiovascular risk is shaped by the entire lipid profile, including triglycerides, remnant cholesterol, and individual treatment response. This article was written to bridge the gap between evolving 2025 clinical guidelines and real-world patient care—highlighting why some individuals remain at risk despite “normal” LDL levels and how newer therapies offer more personalized solutions. My aim is to empower both patients and clinicians with clear, evidence-based insights that move beyond outdated, one-size-fits-all approaches and toward smarter, safer, and more effective cardiovascular prevention.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Individual circumstances vary, and treatment decisions should always be made in consultation with qualified healthcare professionals.
Related Articles
hsCRP Explained: What Inflammation Means for Your Heart | DR T S DIDWAL
What’s New in the 2025 Blood Pressure Guidelines? A Complete Scientific Breakdown | DR T S DIDWAL
Low-Fat vs. Low-Carb: Which Diet is Best for Weight Loss? | DR T S DIDWAL
5 Steps to Reverse Metabolic Syndrome: Diet, Habit, & Lifestyle Plan | DR T S DIDWAL
The Role of Cholesterol in Health and Disease: Beyond the "Bad" Label | DR T S DIDWAL
Lowering Cholesterol with Food: 4 Phases of Dietary Dyslipidemia Treatment | DR T S DIDWAL
The Best Dietary Fat Balance for Insulin Sensitivity, Inflammation, and Longevity | DR T S DIDWAL
References
Gao, Y., Luo, Q. Q., Wang, C. T., Chen, X. M., & Xu, G. Z. (2025). Zhonghua liu xing bing xue za zhi = Zhonghua liuxingbingxue zazhi, 46(5), 921–928. https://doi.org/10.3760/cma.j.cn112338-20241012-00628
Huang, J. X. F., Yousaf, A., Moon, J., Ahmed, R., Upkal, K., & Pemminati, S. (2025). Recent advances in the management of dyslipidemia: A systematic review. Cureus, 17(3), e81034. https://doi.org/10.7759/cureus.81034
Kamrani, F., Imannezhad, M., Rezaee, A., et al. (2025). Emerging importance of remnant cholesterol compared with low-density lipoprotein cholesterol in cardiovascular risk assessment. Scientific Reports, 15, 44094. https://doi.org/10.1038/s41598-025-27681-8
Patel, S. B., Wyne, K. L., Afreen, S., Belalcazar, L. M., Bird, M. D., Coles, S., Marrs, J. C., Peng, C. C., Pulipati, V. P., Sultan, S., & Zilbermint, M. (2025). American Association of Clinical Endocrinology Clinical Practice Guideline on Pharmacologic Management of Adults With Dyslipidemia. Endocrine Practice: Official Journal of the American College of Endocrinology and the American Association of Clinical Endocrinologists, 31(2), 236–262. https://doi.org/10.1016/j.eprac.2024.09.016
Zuin, M., & Bilato, C. (2025). Evolving paradigms in the management of dyslipidemia: Comparison between the 2019 ESC/EAS guidelines and the 2025 focus update. Internal and Emergency Medicine. https://doi.org/10.1007/s11739-025-04234-5