Sleep & Hypertension: Duration, Quality, and Blood Pressure
Is your blood pressure high at night? Discover isolated nocturnal hypertension and why sleep quality, not just duration, is critical for cardiovascular health. 2025 data.
HEART
Dr. T.S. Didwal, M.D.
12/7/202517 min read
When was the last time you felt refreshed after a good night's sleep? If you're struggling to get quality rest, your blood pressure might be paying the price. The connection between sleep patterns and hypertension is increasingly supported by cutting-edge research, revealing that what happens between your bedtime and rising time could significantly influence your cardiovascular health.
Clinical Pearls
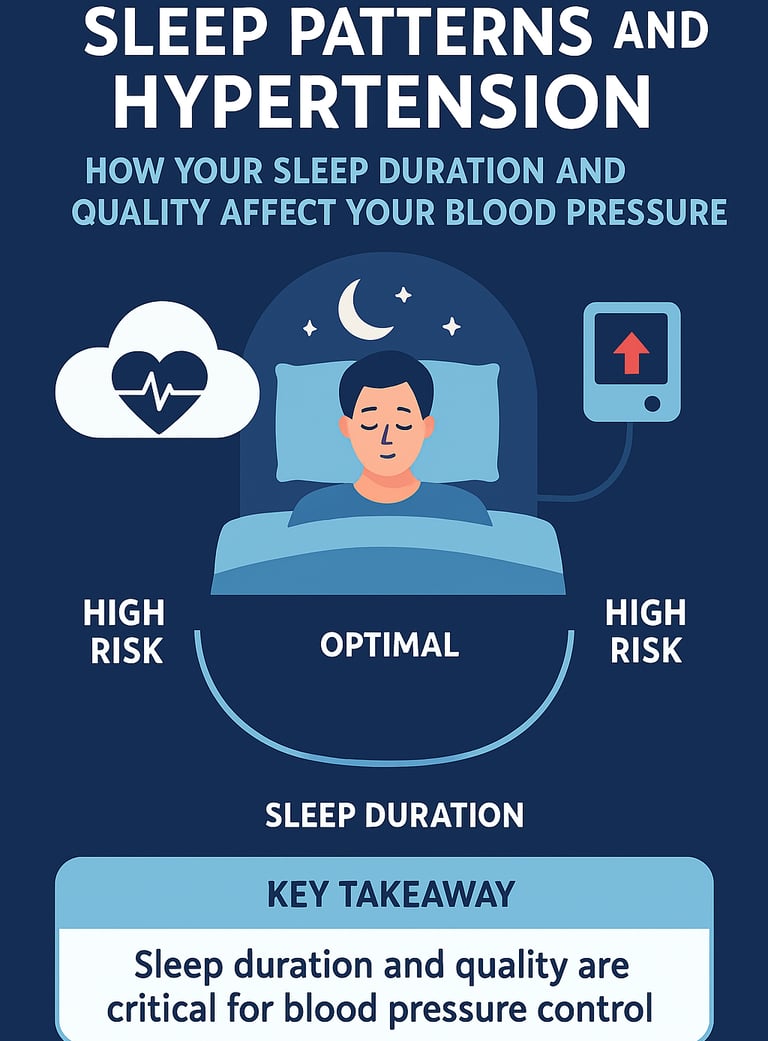
1. Focus on the 7–9 Hour "Sweet Spot" (U-Curve Risk)
The relationship between sleep duration and hypertension risk is not linear but U-shaped or J-shaped. Clinically, you must address both ends of the spectrum.
Optimal Range: Recommend 7–9 hours of sleep nightly for most adults as the protective range.
High-Risk Thresholds: Both insufficient sleep (typically under 6 hours) and excessive sleep (over 10 hours) are associated with a significantly increased risk of hypertension and cardiovascular events (Zhao et al., 2025; Yang et al., 2025).
2. Rule Out Isolated Nocturnal Hypertension with ABPM
Standard in-office blood pressure (BP) readings can be misleading. A significant percentage of patients have isolated nocturnal hypertension—elevated BP only during sleep—which is a distinct and serious cardiovascular risk factor often called a "silent killer" (Minetto et al., 2025).
Action: For patients with unexplained target organ damage, sleep complaints (like snoring or insomnia), or seemingly treatment-resistant hypertension, perform 24-hour Ambulatory Blood Pressure Monitoring (ABPM) to assess the critical nocturnal dipping pattern and detect nocturnal peaks (Hoshide & Kario, 2025).
3. Prioritize Sleep Consistency (Circadian Alignment)
It's not just the quantity (duration) or quality of sleep, but the timing and regularity that matters. Maintaining consistent bedtimes and rising times is crucial for regulating the body's circadian rhythm.
Action: Counsel patients, especially shift workers, that highly variable sleep schedules (sleep inconsistency) stress the cardiovascular system and are independently linked to higher hypertension risk, even if they average 7–9 hours (Zhang et al., 2025).
4. Sleep Quality Overcomes Duration
Poor sleep quality—characterized by fragmented sleep, frequent awakenings, or lack of proper progression through sleep stages—is an independent predictor of nocturnal blood pressure elevation.
Action: If a patient reports 8 hours of sleep but wakes unrefreshed, focus on sleep hygiene and screen for underlying sleep disorders (like obstructive sleep apnea or chronic insomnia). Poor quality sleep activates the sympathetic nervous system, preventing the necessary protective nocturnal BP drop (Minetto et al., 2025).
5. Treat Sleep Health as a Primary Cardiovascular Prevention Strategy
Sleep health promotion should be integrated into cardiovascular risk management with the same rigor as diet and exercise.
Action: Treat identified sleep disorders (apnea, insomnia) aggressively. Recognizing and addressing poor sleep patterns is a foundational step that can enhance the effectiveness of traditional hypertension treatments, rivaling pharmaceutical interventions in impact (Abdalla & Makarem, 2025).
Sleep Patterns and Hypertension: How Your Sleep Duration and Quality Affect Your Blood Pressure
Why Sleep Matters for Your Heart
High blood pressure, or hypertension, affects over one billion people worldwide and remains a leading risk factor for cardiovascular disease. While we often focus on diet and exercise, there's a critical yet frequently overlooked factor: sleep duration and quality. Recent research from 2025 demonstrates that the relationship between sleep architecture and blood pressure regulation is far more complex and significant than previously thought.
This comprehensive guide explores the latest scientific evidence on how sleep patterns influence hypertension risk, examining crucial factors like nocturnal blood pressure peaks, sleep duration thresholds, and the importance of sleep health promotion in cardiovascular prevention. Whether you're at risk for hypertension or seeking to manage existing high blood pressure, understanding these sleep-hypertension connections could transform your approach to health.
The Science Behind Sleep and Blood Pressure
Understanding Hypertension and Its Cardiovascular Impact
Hypertension, commonly called high blood pressure, occurs when the force of blood against artery walls is consistently too high, typically defined as 130/80 mmHg or higher. This condition damages blood vessels over time, increasing the risk of heart disease, stroke, and kidney disease. What makes hypertension particularly dangerous is that many people have it without symptoms—it's often called the "silent killer."
Your blood pressure naturally fluctuates throughout the day in a pattern called diurnal variation. Normally, blood pressure drops during sleep in what researchers call a "dipping" pattern. However, not everyone experiences this beneficial nighttime dip, and some people even experience elevated pressure at night—a phenomenon called nocturnal hypertension (Minetto et al., 2025).
The Sleep-Hypertension Connection: Key Mechanisms
The relationship between sleep patterns and cardiovascular health operates through several biological mechanisms. During quality sleep, your sympathetic nervous system—responsible for your "fight or flight" response—naturally calms down. This allows blood vessels to relax and blood pressure to decrease. Conversely, poor sleep or insufficient sleep duration keeps your nervous system in a heightened state, maintaining elevated blood pressure throughout the night and into the next day.
Sleep also regulates hormones that control blood pressure regulation, including cortisol and aldosterone. When you don't get enough sleep, these hormones become dysregulated, promoting sodium retention and increased vascular resistance. Additionally, sleep deprivation increases inflammation markers linked to cardiovascular disease, creating a cascading effect on your heart health.
Isolated Nocturnal Hypertension: Understanding the Hidden Risk
A groundbreaking study by Minetto, Espeche, Cerri and colleagues examined isolated nocturnal hypertension and its association with sleep duration and quality. This research provides crucial insights into a specific phenotype of hypertension that often goes undetected in standard office blood pressure readings.
Isolated nocturnal hypertension refers to elevated blood pressure during sleep without corresponding daytime elevation. This condition is particularly important because many people visit their doctor during the day when their blood pressure readings appear normal, missing this hidden cardiovascular risk factor entirely. The study emphasized that sleep quality metrics and sleep duration thresholds play pivotal roles in determining whether individuals develop this specific hypertension pattern.
The research demonstrated that individuals experiencing poor sleep quality and suboptimal sleep duration showed significantly higher rates of nocturnal blood pressure peaks (Minetto et al., 2025). The study highlighted the importance of assessing both the quantity and quality of sleep, as neither factor alone adequately predicted nocturnal hypertension development.
One critical takeaway is that isolated nocturnal hypertension may represent an important intermediate cardiovascular risk state. Patients with this condition showed increased target organ damage and cardiovascular complications despite normal daytime readings. This underscores the necessity for comprehensive 24-hour ambulatory blood pressure monitoring rather than relying solely on office measurements.
Key Takeaways from Minetto et al.:
Sleep quality is independently associated with nocturnal blood pressure elevation
Isolated nocturnal hypertension represents a distinct and clinically significant hypertension phenotype
Standard office readings may miss up to 30% of patients with nocturnal hypertension
Both quantity and quality of sleep matter for blood pressure regulation
Sleep Duration Thresholds and Hypertension Risk
The 2025 research by Zhao, Song, and Liu, published in Blood Pressure, provides groundbreaking insights into sleep duration thresholds and hypertension risk. This work challenges the one-size-fits-all approach to sleep recommendations and reveals that optimal sleep duration exists on a spectrum, with critical threshold points that define risk categories.
The study examined how different sleep duration ranges impact hypertension development, moving beyond simple categorizations of "too short" or "adequate" sleep. The researchers investigated whether there are specific sleep duration thresholds where cardiovascular risk increases substantially.
Critical Findings on Sleep Duration
The research identified optimal sleep duration ranges for hypertension prevention, suggesting that approximately 7-9 hours per night represents the sweet spot for most adults. However, the relationship between sleep duration and blood pressure isn't entirely linear. The study found that very long sleep durations (over 10 hours nightly) also correlate with increased hypertension risk, suggesting a U-shaped or J-shaped relationship (Zhao et al., 2025).
Particularly compelling was the discovery that the transition points—where risk increases—occur at specific sleep duration thresholds. Individuals sleeping significantly below or above optimal ranges showed markedly elevated cardiovascular disease risk. This nuanced finding suggests that sleep health promotion strategies should be personalized rather than universally prescriptive.
The research also highlighted that the relationship between sleep duration and hypertension becomes increasingly important with age. Younger adults showed greater adaptability to suboptimal sleep, while middle-aged and older adults demonstrated more pronounced blood pressure elevation with inadequate sleep.
Key Takeaways from Zhao et al.:
Optimal sleep duration for hypertension prevention falls between 7-9 hours nightly
Sleep duration thresholds exist where cardiovascular risk increases substantially
The relationship between sleep and blood pressure follows a U or J-shaped curve
Both insufficient and excessive sleep are associated with a higher hypertension risk
Age modifies the relationship between sleep duration and cardiovascular health
Sleep Patterns and Cardiovascular Disease: Real-World NHANES Data
Zhang, Wang, and Liu's comprehensive analysis used data from the National Health and Nutrition Examination Survey (NHANES) conducted from 2017-2020, examining associations of sleep pattern, sleep duration, bedtime, rising time and cardiovascular disease. This large-scale epidemiological study provides robust real-world evidence of how sleep patterns influence cardiovascular health across diverse populations.
The NHANES dataset included comprehensive information on sleep duration, bedtime, rising time, and various sleep quality indicators, linked to verified cardiovascular disease outcomes. The researchers analyzed these relationships across different demographic groups, accounting for numerous confounding variables.
Major Findings on Sleep Timing and Patterns
The study revealed that sleep patterns—not just duration alone—significantly influence cardiovascular risk (Zhang et al., 2025). Beyond simply sleeping 7-9 hours, the timing of sleep matters considerably. Individuals with consistent sleep schedules, including consistent bedtimes and rising times, showed better blood pressure control than those with irregular sleep patterns.
Particularly notable was the finding regarding chronotype (whether you're naturally a morning or evening person) and sleep timing. When individuals worked against their natural chronotype, sleeping at unconventional times, they exhibited higher hypertension rates even when total sleep duration was adequate. This suggests that sleep quality involves more than duration—circadian alignment plays a crucial role.
The research also demonstrated that shift workers and those with irregular sleep schedules faced substantially higher hypertension risk compared to those with consistent sleep patterns. This finding has profound implications for occupational health and workplace wellness programs.
Key Takeaways from Zhang et al.:
Sleep timing and sleep pattern consistency independently predict hypertension risk
Irregular sleep schedules and shifting bedtimes elevate cardiovascular disease risk
Circadian alignment—sleeping in sync with your natural rhythm—improves blood pressure regulation
Shift workers face particular hypertension risk requiring targeted interventions
Real-world NHANES data confirms laboratory findings about sleep patterns and cardiovascular health
Nocturnal Blood Pressure Peak Assessment: Practical Clinical Considerations
Hoshide and Kario's 2025 contribution to Hypertension Research addresses practical considerations for assessing nocturnal blood pressure peak, providing clinically actionable guidance for healthcare providers. This work focuses on the technical and practical aspects of measuring nocturnal hypertension, an increasingly recognized but still underdiagnosed condition.
The authors emphasize that proper assessment of nocturnal blood pressure requires specific methodologies and considerations that differ from standard daytime blood pressure measurement. They respond to previous recommendations, providing expert consensus on best practices for detecting nocturnal blood pressure peaks (Hoshide & Kario, 2025).
Clinical Assessment and Detection Methods
The research highlights that standard office-based blood pressure readings completely miss nocturnal hypertension. Proper assessment requires 24-hour ambulatory blood pressure monitoring (ABPM), which captures blood pressure readings throughout the day and night, revealing the critical nocturnal dipping pattern.
A crucial distinction emerges from their analysis: not all individuals with elevated nighttime readings face identical risk. The magnitude of nocturnal blood pressure peaks and the presence or absence of normal dipping patterns stratify risk differently. Some individuals might have modestly elevated nocturnal readings but maintain normal dipping, while others lose the protective dip entirely—a distinction with significant prognostic implications.
The study provides practical guidance for clinicians, including optimal timing for ambulatory blood pressure monitoring, interpretation of nocturnal blood pressure patterns, and identification of high-risk phenotypes requiring intensive intervention. The authors recommend that nocturnal hypertension assessment become standard practice for patients with apparent treatment-resistant hypertension or those with sleep complaints.
Key Takeaways from Hoshide & Kario:
24-hour ambulatory blood pressure monitoring is essential for detecting nocturnal hypertension
Nocturnal blood pressure peaks and dipping patterns carry distinct prognostic significance
Practical clinical protocols can effectively identify patients with nocturnal hypertension
Sleep-related blood pressure elevation requires specific assessment approaches
Integration of nocturnal blood pressure monitoring into routine clinical practice improves patient outcomes
Sleep Health Promotion as Cardiovascular Prevention Strategy
Abdalla and Makarem's publication in the Journal of the American College of Cardiology presents a compelling case for sleep health promotion as a primary and secondary cardiovascular disease prevention strategy. This perspective piece synthesizes emerging evidence that adequate sleep health should be considered alongside traditional risk factor modification in hypertension management (Abdalla & Makarem, 2025).
The authors argue convincingly that sleep health deserves equal attention with diet, exercise, and medication in comprehensive cardiovascular prevention programs. They present evidence that optimizing sleep duration, sleep quality, and sleep patterns can reduce cardiovascular disease risk as effectively as many pharmaceutical interventions.
Integrated Sleep Health in Cardiovascular Care
The research emphasizes that sleep health promotion isn't merely supportive to standard hypertension treatment—it's foundational to it. Patients struggling to manage blood pressure through lifestyle changes alone often have unrecognized sleep disorders or suboptimal sleep patterns undermining their efforts.
Abdalla and Makarem advocate for systematic sleep health assessment as part of routine cardiovascular evaluation. This includes screening for sleep apnea, evaluating sleep duration, assessing sleep quality, and identifying behavioral or environmental factors compromising sleep. Healthcare providers should ask patients about their sleep patterns with the same rigor typically applied to dietary habits.
The authors provide evidence-based strategies for sleep health optimization, including sleep hygiene improvements, treatment of underlying sleep disorders, and lifestyle modifications promoting better sleep quality. When integrated into comprehensive cardiovascular prevention programs, sleep health interventions significantly enhance outcomes compared to traditional approaches alone.
Key Takeaways from Abdalla & Makarem:
Sleep health deserves primary focus in cardiovascular prevention strategies
Sleep assessment should be routine in cardiovascular evaluation and hypertension management
Optimizing sleep patterns and quality rivals pharmaceutical interventions for blood pressure reduction
Sleep disorders require identification and treatment as part of comprehensive cardiovascular care
Integrated sleep health promotion enhances outcomes in hypertension prevention and management
Sleep Duration and Hypertension in Young and Middle-Aged Adults: Meta-Analysis Evidence
Yang, Hu, Wang, and colleagues conducted a comprehensive systematic review and meta-analysis examining the association of sleep duration with hypertension in young and middle-aged adults. Published in the International Journal of Cardiology: Cardiovascular Risk and Prevention, this work synthesizes evidence from multiple studies to identify robust patterns in how sleep duration influences hypertension across these critical life stages (Yang et al., 2025).
The meta-analytic approach allows identification of consistent relationships across diverse populations and study designs, providing stronger evidence than individual studies alone. The researchers included numerous high-quality studies, examining how sleep duration (both insufficient and excessive) relates to hypertension prevalence and incidence.
Age-Specific Findings on Sleep and Hypertension
The meta-analysis revealed that short sleep duration—typically defined as less than 6 hours nightly—significantly increases hypertension risk in both young and middle-aged adults. The relative risk increase was substantial, particularly in middle-aged populations where cardiovascular vulnerability increases.
Notably, the relationship between sleep duration and hypertension differed between age groups. Young adults (under 40) showed greater tolerance for occasional short sleep without hypertension development, likely reflecting superior cardiovascular compensation mechanisms. However, chronic sleep deprivation in young adults still elevated hypertension risk substantially.
Middle-aged adults (40-65 years) demonstrated the most pronounced sleep duration-hypertension associations. In this group, the benefits of consistent sleep duration optimization were most dramatic. Individuals maintaining 7-9 hours of nightly sleep showed substantially lower hypertension prevalence compared to those sleeping 6 hours or less.
The analysis also identified that the sleep duration-hypertension relationship becomes stronger with increasing age within each category, suggesting progressive loss of cardiovascular adaptability to suboptimal sleep as we age.
Key Takeaways from Yang et al.:
Short sleep duration (under 6 hours) significantly increases hypertension risk across age groups
Middle-aged adults show the most pronounced sleep duration-hypertension associations
The protective effects of adequate sleep duration accumulate over years
Young adults have greater short-term tolerance but still face risk from chronic sleep deprivation
Age-specific strategies may optimize sleep health interventions for hypertension prevention
Synthesizing the Evidence: What These Studies Tell Us Together
The six major 2025 studies on sleep patterns and hypertension present a remarkably consistent message: the relationship between sleep and blood pressure is multifaceted, significant, and crucial for cardiovascular health. No single factor—not duration alone, not quality alone, not timing alone—tells the complete story. Instead, comprehensive sleep health, encompassing duration, quality, timing, and consistency, emerges as fundamental to hypertension prevention and management.
These studies collectively demonstrate that:
Sleep duration matters, but with important nuance. The traditional recommendation of "at least 7 hours" accurately captures an important threshold, but more precisely, 7-9 hours represents an optimal range. Both significantly shorter and significantly longer sleep durations associate with elevated hypertension risk, suggesting that sleep needs aren't universally one-size-fits-all.
Sleep quality and architecture independently influence blood pressure regulation. Simply spending time in bed doesn't guarantee beneficial effects; the quality of that sleep—including proper progression through sleep stages and adequate deep sleep—matters considerably.
Sleep timing and patterns influence cardiovascular risk through circadian mechanisms. Maintaining consistent sleep schedules and sleeping in alignment with your natural chronotype optimizes blood pressure regulation.
Nocturnal blood pressure patterns carry distinct diagnostic and prognostic significance. The presence or absence of normal nocturnal dipping and the magnitude of nocturnal blood pressure peaks predict cardiovascular outcomes independent of daytime readings.
Vulnerable populations face particular importance from sleep optimization. Shift workers, young adults beginning patterns that track into middle age, and middle-aged adults experiencing cardiovascular transitions all benefit from prioritizing sleep health.
Practical Applications: Optimizing Your Sleep for Better Blood Pressure Control
Sleep Duration Optimization
Start by honestly assessing your current sleep duration. Most adults benefit from 7-9 hours nightly, but individual needs vary. Pay attention to how you feel with different sleep durations rather than rigidly adhering to targets. If you consistently feel rested with 7.5 hours and maintain that schedule, that's likely optimal for you. If you find yourself struggling to stay awake despite sleeping 8 hours, you might need more.
Consistency matters as much as duration. Rather than sleeping 5 hours on weeknights and 12 hours on weekends, maintain steady sleep schedules even across days off. This consistency supports your body's circadian rhythm regulation, optimizing blood pressure patterns throughout the day.
Improving Sleep Quality
Quality sleep requires attention to environment and habits. Keep your bedroom cool (around 65-68°F), dark, and quiet. Invest in comfortable bedding and a supportive mattress. Establish a consistent wind-down routine beginning 30-60 minutes before bed, involving relaxing activities like reading, gentle stretching, or meditation.
Limit screen exposure in the hour before sleep, as blue light suppresses melatonin production. If you use electronic devices, employ blue light filters. Avoid caffeine at least 6 hours before bed and alcohol in the evening, both of which disrupt sleep architecture.
Sleep Timing and Circadian Alignment
Identify your natural chronotype—are you naturally a morning person or night owl? While work obligations sometimes conflict with chronotype, aligning sleep timing with your natural preferences whenever possible optimizes sleep quality and blood pressure regulation. If you're a natural night owl, negotiate evening start times if possible. If you're a morning person, don't force yourself to stay up late.
Pay attention to your bedtime and rising time. Even if total sleep duration meets recommendations, dramatic day-to-day variations disrupt circadian regulation. Consistency trumps absolute timing in most cases.
Addressing Sleep Disorders
If you snore, experience gasping during sleep, wake unrefreshed despite long sleep durations, or suffer from insomnia, discuss these issues with a healthcare provider. Sleep apnea and other sleep disorders significantly elevate hypertension risk and are treatable. Diagnosis typically involves screening questionnaires followed by sleep study confirmation if indicated.
Comprehensive Lifestyle Integration
Remember that sleep health doesn't exist in isolation. Regular exercise improves sleep quality and blood pressure regulation, but intense exercise within 3 hours of bedtime can interfere with sleep onset. Morning or afternoon exercise optimizes both benefits.
Dietary patterns influence sleep. While alcohol might initially help you fall asleep, it severely disrupts sleep quality and architecture. A balanced diet rich in vegetables, whole grains, and lean proteins supports both sleep and cardiovascular health.
Stress management techniques including meditation, yoga, and deep breathing exercises improve sleep quality and directly reduce blood pressure, creating synergistic benefits.
FAQs: Common Questions About Sleep and Blood Pressure
Q: How much sleep do I really need to protect my blood pressure? A: Research suggests 7-9 hours nightly for most adults, but individual needs vary. More important than hitting a specific number is maintaining consistent sleep duration night-to-night and waking feeling refreshed. If you feel rested on 7 hours consistently, that's likely adequate for you. If you remain drowsy, you probably need more.
Q: Can poor sleep quality cause high blood pressure even if I sleep 8 hours? A: Absolutely. Spending 8 hours in bed means nothing if you're awake half that time or only partially asleep. Sleep quality—characterized by progressing through proper sleep stages—independently influences blood pressure regulation. Poor quality sleep activates your sympathetic nervous system, preventing the beneficial blood pressure dip that normally occurs during sleep.
Q: I'm a shift worker. Can I still manage my blood pressure well? A: Shift work significantly increases hypertension risk due to circadian disruption, but strategies can help. Maintain consistent sleep schedules even across shift rotations when possible. Use bright light exposure strategically to reinforce your desired sleep-wake schedule. Consult your healthcare provider about whether treatment adjustments might benefit you, and discuss workplace accommodations that might support better sleep.
Q: Does the time of day I sleep matter, or just total duration? A: Both matter, but through different mechanisms. Total sleep duration reflects the time available for physiological restoration. Sleep timing affects your circadian rhythm regulation. Ideally, your sleep aligns with both your natural chronotype and society's general pattern. Sleeping at unconventional times stresses your system even if duration is adequate.
Q: I sleep 10-11 hours nightly and still feel tired. Should I be concerned about my blood pressure? A: Sleeping excessively while remaining unrefreshed suggests possible underlying sleep disorders like sleep apnea or other conditions. Long sleep duration itself associates with increased hypertension risk in some studies. I'd recommend discussing this pattern with your doctor, who may recommend sleep evaluation. You likely need assessment rather than more sleep.
Q: Are there supplements that improve sleep quality and lower blood pressure? A: While some supplements like magnesium and melatonin show modest evidence for sleep quality improvement, they're not substitutes for healthy sleep habits. Discuss any supplements with your healthcare provider, particularly if you're on blood pressure medications, as interactions can occur. Evidence-based approaches like sleep hygiene, exercise, and stress reduction remain most effective.
Q: How quickly will improving my sleep affect my blood pressure? A: Some benefits appear within days—consistent good sleep can lower blood pressure significantly within a week. However, the magnitude of benefit depends on how much room for improvement exists and how committed you are to sustained change. Dramatic improvements often emerge over 4-8 weeks of consistent better sleep.
Q: My blood pressure is normal when I visit my doctor, but I've heard about nocturnal hypertension. How do I know if I have it? A: Normal office readings don't exclude nocturnal hypertension. If you suspect this might affect you—particularly if you have sleep complaints, family history of hypertension, or other cardiovascular risk factors—ask your doctor about 24-hour ambulatory blood pressure monitoring. This test captures readings throughout the day and night, revealing whether you have nocturnal hypertension that office readings miss.
Conclusion: Taking Action on Sleep for Your Cardiovascular Health
The evidence is clear and compelling: your sleep patterns significantly influence your blood pressure and overall cardiovascular health. The 2025 research examined throughout this guide demonstrates that optimizing sleep duration, ensuring sleep quality, maintaining consistent sleep timing, and addressing underlying sleep disorders represent powerful cardiovascular prevention strategies.
Unlike many health interventions requiring expensive medications or complicated procedures, sleep health optimization begins with free or low-cost behavioral changes: consistent bedtimes, bedroom environment optimization, screen management, and stress reduction. The barrier isn't cost or complexity—it's making sleep a priority.
If you struggle with high blood pressure, start by honestly assessing your sleep patterns. Are you consistently getting 7-9 hours? Is your sleep quality good, or are you tossing and turning, waking throughout the night, or snoring? Do you maintain consistent sleep schedules, or do your bedtimes and rising times vary wildly? Are you working against your natural chronotype?
Begin with one or two manageable changes. Perhaps establish a consistent bedtime and rising time. Or optimize your bedroom environment. Then gradually implement other recommendations. As you improve your sleep, monitor how your overall health feels—you'll likely notice benefits beyond blood pressure reduction, including improved mood, better daytime energy, and enhanced cardiovascular function.
Most importantly, discuss sleep health with your healthcare provider. They can assess whether you need screening for sleep disorders, evaluate your current blood pressure patterns through 24-hour monitoring if indicated, and help you develop a comprehensive hypertension management strategy that includes sleep optimization alongside other evidence-based approaches.
Your sleep isn't a luxury or something to sacrifice for productivity—it's medicine for your cardiovascular system. Invest in it, prioritize it, and let the science of sleep and hypertension guide you toward better health.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Individual circumstances vary, and treatment decisions should always be made in consultation with qualified healthcare professionals.
Related Articles
The BMI Paradox: Why "Normal Weight" People Still Get High Blood Pressure | DR T S DIDWAL
How Insulin Resistance Accelerates Cardiovascular Aging | DR T S DIDWAL
References
Abdalla, M., & Makarem, N. (2025). Promoting sleep health to prevent and manage systemic hypertension. Journal of the American College of Cardiology, 86(18), 1498–1500. https://doi.org/10.1016/j.jacc.2025.08.077
Hoshide, S., & Kario, K. (2025). Practical considerations for assessing nocturnal blood pressure peak: A response to Wang et al. Hypertension Research, 48, 121–123. https://doi.org/10.1038/s41440-025-02479-3
Minetto, J., Espeche, W., Cerri, G., et al. (2025). Isolated nocturnal hypertension and its association with sleep duration and quality. Journal of Human Hypertension, 39(2), 123–131. https://doi.org/10.1038/s41371-025-01099-1
Yang, L., Hu, F. X., Wang, K., Wang, Z. Z., & Yang, J. (2025). Association of sleep duration with hypertension in young and middle-aged adults: A systematic review and meta-analysis. International Journal of Cardiology: Cardiovascular Risk and Prevention, 25, 200387. https://doi.org/10.1016/j.ijcrp.2025.200387
Zhang, X., Wang, D., & Liu, J. (2025). Associations of sleep pattern, sleep duration, bedtime, rising time and cardiovascular disease: Data from NHANES (2017-2020). PLoS ONE, 20(7), e0326499. https://doi.org/10.1371/journal.pone.0326499
Zhao, Z., Song, X., & Liu, X. (2025). Reimagining cardiovascular prevention: Insights from study on sleep duration thresholds and hypertension risk. Blood Pressure, 34(1), 45–58. https://doi.org/10.1080/08037051.2025.2557404