Beyond the Clock: Five Core Dimensions of Sleep Health and Disease Risk
Are you tracking the wrong sleep metrics? Explore the five dimensions of sleep health—regularity, quality, timing, efficiency, and duration—and how they impact your risk for heart disease and mortality based on 2025 research
DIABETES
Dr. T.S. Didwal, M.D.(Internal Medicine)
1/6/202614 min read

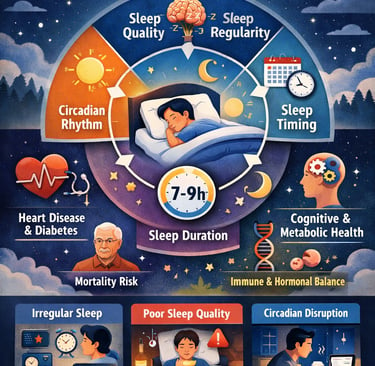
For years, good sleep has been defined by a simple number: 7–9 hours per night. But emerging research shows that this narrow focus misses a much bigger—and far more important—picture. Many people wake up feeling unrefreshed despite sleeping “enough,” while others function well on slightly shorter sleep. Why? Because sleep health is not just about duration; it is multidimensional.
Recent large-scale studies now demonstrate that sleep quality, regularity, and timing may matter as much as—or even more than—how long you sleep. A landmark scientific statement from the American Heart Association emphasizes that irregular sleep schedules, poor sleep quality, and circadian misalignment independently increase the risk of cardiovascular disease, diabetes, obesity, and premature mortality, even when total sleep duration is adequate (St-Onge et al., 2025). Supporting this shift, a major UK Biobank study involving over 60,000 adults found that sleep regularity was a stronger predictor of mortality risk than sleep duration itself (Windred et al., 2024).
In parallel, mechanistic research reveals how irregular or fragmented sleep disrupts circadian rhythms, impairing glucose metabolism, hormonal balance, immune function, and cognitive performance (Hartstein et al., 2025). Together, these findings signal a paradigm shift: sleep consistency and quality are not optional—they are central to long-term health.
This article explores why how you sleep may matter more than how long you sleep—and what that means for your heart, metabolism, and longevity.
Clinical pearls
1. The "Anchor" Principle: Regularity Trumps Duration
While we’ve long obsessed over getting 7–9 hours, the Sleep Regularity Index (SRI) is now considered a superior predictor of longevity. A person who sleeps 6 hours consistently every night often has better metabolic and cardiovascular profiles than a "weekend warrior" who fluctuates between 6 and 9 hours.
The Pearl: Your body’s internal clock (circadian rhythm) thrives on predictability. Keeping your wake-up time within a 30-minute window every day is the single most effective way to "anchor" your biology.
2. Efficiency Over "In-Bed" Time
Spending 10 hours in bed to get 7 hours of sleep creates a psychological association between the bed and wakefulness (or anxiety). Clinical research shows that high Sleep Efficiency—the ratio of time spent asleep versus time in bed—is a key marker of sleep health.
The Pearl: If you aren't asleep within 20 minutes, get out of bed. Use the bed only for sleep and intimacy to reinforce the neural pathway that Bed = Sleep.
3. Protect the "Slow-Wave" Physical Repair
Deep sleep (Non-REM Stage 3) is when your body clears metabolic waste from the brain via the glymphatic system and repairs muscle tissue. Fragmented sleep—caused by alcohol, late-night meals, or noise—shears off these deep sleep cycles even if your total "hours" look normal on a tracker.
The Pearl: Alcohol is a "sleep thief." It may help you fall asleep faster, but it acts as a sedative that destroys sleep architecture, specifically suppressing the restorative deep sleep stages.
4. Light is a Biological Signal, Not Just a Convenience
The Hartstein (2025) research emphasizes that our "master clock" is set by light. Morning light exposure suppresses melatonin and sets a timer for its release 14–16 hours later. Conversely, blue light at night creates "circadian misalignment," tricking the brain into thinking it’s mid-day.
The Pearl: View sunlight within 30 minutes of waking. This simple act of "optical signaling" aligns your hormones and makes falling asleep at night a biological inevitability rather than a struggle.
5. Subjective Satisfaction is a Valid Clinical Metric
The Harvard Health synthesis (2025) reminds us that Sleep Satisfaction—how you feel—is often as predictive of health outcomes as objective data. If your wearable says you slept 8 hours but you feel unrefreshed, there may be underlying "micro-arousals" (often from sleep apnea or periodic limb movements) that the tracker is missing.
The Pearl: Don't let your sleep tracker gaslight you. If you feel chronically fatigued despite "good" numbers, it’s a clinical signal to investigate sleep quality (obstructions or disturbances) rather than just increasing quantity.
Rethinking What Makes Good Sleep : Why Sleep Quality and Regularity Matter More Than Hours in Bed
What Is Multidimensional Sleep Health?
Traditional sleep research focused heavily on sleep duration—the number of hours you spend asleep. However, this single metric doesn't capture the full picture of sleep health. Recent evidence shows that sleep is a complex, multidimensional behavior involving several key components:
Sleep duration (how long you sleep)
Sleep quality (how well you sleep)
Sleep regularity (consistency of sleep-wake timing)
Sleep timing (when you sleep relative to your circadian rhythm)
Sleep efficiency (time asleep vs. time in bed)
Alertness during waking hours (daytime functioning)
Each of these dimensions contributes independently to health outcomes, meaning you can't compensate for poor sleep quality or irregular sleep patterns simply by spending more time in bed.
Study #1: American Heart Association's Scientific Statement on Multidimensional Sleep Health
Overview and Key Findings
In January 2025, the American Heart Association (AHA) published a landmark scientific statement redefining how we should think about sleep and cardiometabolic health (St-Onge et al., 2025). This comprehensive review synthesized decades of research to establish that sleep health is multidimensional and each dimension has distinct effects on heart disease risk, diabetes, obesity, and metabolic syndrome.
The Six Dimensions of Sleep Health According to the AHA
The AHA identified six critical dimensions:
Regularity: Consistent sleep-wake schedules across weekdays and weekends
Satisfaction/Quality: Feeling rested and experiencing restorative sleep
Alertness: Maintaining wakefulness during desired waking hours
Timing: Sleeping during biologically appropriate times (aligned with circadian rhythms)
Efficiency: High percentage of time in bed actually spent asleep
Duration: Appropriate amount of sleep (typically 7-9 hours for adults)
Why This Matters for Your Heart Health
The AHA statement emphasizes that poor sleep quality and irregular sleep patterns are independent risk factors for:
Cardiovascular disease
Hypertension (high blood pressure)
Type 2 diabetes
Obesity
Metabolic syndrome
Importantly, improving just one dimension (like sleeping longer) while neglecting others (like sleep regularity or quality) may not provide the cardiovascular benefits you'd expect.
Sleep health should be assessed across multiple dimensions, not just duration. Healthcare providers should screen patients for sleep irregularity, poor sleep quality, and circadian misalignment—not just insufficient sleep—when evaluating cardiometabolic risk.
Study #2: Sleep Regularity as a Stronger Predictor of Mortality Than Duration
Groundbreaking Findings from the UK Biobank Study
Perhaps the most striking finding in recent sleep research comes from Windred et al. (2024), who analyzed data from over 60,000 participants in the UK Biobank study. Their conclusion? Sleep regularity is a stronger predictor of mortality risk than sleep duration.
The Sleep Regularity Index (SRI)
The researchers developed a Sleep Regularity Index that measures how consistent your sleep-wake patterns are from day to day. Higher scores indicate more regular sleep schedules.
Shocking Results
Participants with irregular sleep patterns had:
Significantly higher all-cause mortality risk compared to regular sleepers
Increased risk of death from cardiovascular disease
Higher cancer mortality rates
Even more surprisingly, these associations persisted regardless of sleep duration. In other words, you could sleep 8 hours every night, but if your bedtime and wake time vary widely from day to day, your mortality risk remains elevated.
Social Jetlag and Weekend Sleep-In Effects
Many people maintain regular sleep schedules during the workweek but shift their sleep timing dramatically on weekends—a phenomenon called "social jetlag." This study suggests that even weekend irregularity can have cumulative negative effects on health and longevity.
Consistency matters more than quantity. Going to bed and waking up at similar times every day—yes, even on weekends—may be one of the most important things you can do for long-term health and longevity.
Study #3: Sleep Irregularity and Circadian Rhythmicity
Understanding Your Internal Clock
Hartstein et al. (2025) published an important review examining how sleep irregularity disrupts circadian rhythms—the 24-hour internal biological clock that regulates not just sleep-wake cycles, but also hormone release, metabolism, immune function, and countless other physiological processes.
The Circadian Disruption Cascade
When your sleep schedule varies significantly from day to day, your circadian system struggles to synchronize with environmental cues. This circadian misalignment triggers a cascade of negative effects:
Metabolic dysregulation: Impaired glucose metabolism and insulin sensitivity
Hormonal imbalances: Disrupted cortisol, melatonin, and growth hormone rhythms
Inflammation: Increased inflammatory markers associated with chronic disease
Cognitive impairment: Reduced attention, memory, and executive function
The Modern Lifestyle Challenge
Our modern 24/7 society—with artificial lighting, shift work, electronic devices, and social obligations—makes circadian disruption increasingly common. The researchers note that irregular sleep patterns essentially create a state of chronic circadian desynchrony, similar to perpetual jetlag.
Practical Implications
Hartstein and colleagues emphasize that interventions targeting sleep regularity and circadian alignment—such as consistent sleep schedules, strategic light exposure, and properly timed meals—may be more effective than simply encouraging longer sleep duration.
Your circadian rhythm thrives on predictability. Irregular sleep patterns create biological confusion that extends far beyond feeling tired, affecting metabolism, immunity, and long-term health outcomes.
Study #4: It's Not Just How Long, But How You Sleep
Beyond the Clock: Sleep Architecture Matters
Arora and Moreno (2025) make a compelling case that the quality and structure of sleep—what scientists call "sleep architecture"—is just as important as duration. Their research highlights that two people can both sleep 8 hours, but experience vastly different health outcomes based on how they sleep.
What Is Sleep Architecture?
Sleep architecture refers to the cyclical pattern of sleep stages throughout the night:
Non-REM Stage 1: Light sleep transition
Non-REM Stage 2: Deeper sleep with memory consolidation
Non-REM Stage 3: Deep sleep (slow-wave sleep) crucial for physical restoration
REM Sleep: Dreaming sleep important for emotional processing and learning
Healthy sleep involves cycling through these stages 4-6 times per night in a predictable pattern.
Sleep Disruption vs. Sleep Deprivation
The study distinguishes between:
Sleep deprivation: Insufficient sleep duration
Sleep disruption: Fragmented sleep with frequent awakenings and disrupted sleep architecture
Many people experience sleep disruption even while spending adequate time in bed. Conditions like sleep apnea, insomnia, restless leg syndrome, and environmental factors (noise, light, temperature) can fragment sleep and prevent progression through normal sleep cycles.
Health Consequences of Poor Sleep Quality
Arora and Moreno document how disrupted sleep architecture contributes to:
Cognitive deficits: Impaired memory consolidation and learning
Mood disorders: Increased risk of depression and anxiety
Metabolic problems: Altered appetite hormones (leptin and ghrelin)
Immune dysfunction: Reduced resistance to infections
Cardiovascular strain: Elevated blood pressure and heart rate variability
Sleep quality trumps quantity. Focus on creating conditions for uninterrupted, restorative sleep with proper progression through all sleep stages, not just maximizing time in bed.
Study #5: Harvard Health's Synthesis on Sleep Dimensions
Translating Research into Practice
In a comprehensive review for Harvard Health Publishing, Corliss (2025) synthesized recent sleep research into practical guidance for patients and clinicians, emphasizing the multidimensional approach to sleep health.
The ReST Framework
Corliss introduces a helpful acronym—ReST—to remember the key dimensions:
Regularity: Consistent sleep-wake schedules
Satisfaction/Quality: Feeling refreshed upon waking
Timing: Sleeping during biologically appropriate hours
Sleep Satisfaction: The Subjective Component
An often-overlooked dimension is sleep satisfaction—how you feel about your sleep. This subjective measure captures aspects that objective metrics might miss:
Feeling refreshed and restored upon waking
Sleeping without excessive effort or struggle
Feeling satisfied with sleep quality
Research shows sleep satisfaction independently predicts health outcomes, even controlling for objective sleep measures.
The 24-Hour Perspective
Corliss emphasizes viewing sleep health within a 24-hour framework that includes:
Daytime alertness and functioning
Physical activity patterns and timing
Light exposure throughout the day
Meal timing and evening eating habits
Evening wind-down routines
This holistic perspective recognizes that what you do during waking hours profoundly impacts nighttime sleep, and vice versa.
Optimal sleep health requires attention to multiple dimensions simultaneously. No single intervention—whether medication, supplements, or lifestyle changes—will be effective if it addresses only one dimension while ignoring others.
Integrating the Research: What This Means for You
The Five Pillars of Sleep Health
Based on these five studies, we can identify five essential pillars of healthy sleep:
1. Prioritize Sleep Regularity
Go to bed and wake up at consistent times every day, including weekends
Aim for variation of less than 30 minutes in sleep-wake timing
Minimize social jetlag by maintaining weekday schedules on weekends
2. Optimize Sleep Quality
Create a sleep environment conducive to uninterrupted sleep
Address sleep disorders like sleep apnea or insomnia with professional help
Minimize sleep fragmentation from noise, light, or temperature disturbances
Allow sufficient time for complete sleep cycles (90-120 minutes each)
3. Align with Your Circadian Rhythm
Sleep during hours that match your biological clock (typically nighttime)
Get bright light exposure early in the day
Dim lights and reduce blue light exposure in evening hours
Avoid shift work patterns when possible
4. Maintain Adequate Duration
While not the only factor, sleep duration still matters
Most adults need 7-9 hours of sleep per night
Individual needs vary; focus on feeling rested and alert during the day
5. Assess Daytime Functioning
Monitor your alertness and energy throughout the day
Evaluate cognitive performance and mood
Note any excessive daytime sleepiness (may indicate sleep disorders)
Moving Beyond Sleep Tracking Obsession
Interestingly, these studies suggest we should be less obsessed with sleep duration numbers and more attentive to consistency, quality, and how we feel. Your sleep tracker showing 7.5 hours might look "insufficient," but if those hours are regular, high-quality, well-timed, and leave you feeling refreshed, you're likely doing better than someone with irregular 8.5-hour nights.
Common Sleep Myths Debunked by This Research
Myth 1: "I Can Catch Up on Sleep This Weekend"
Reality: The Windred et al. (2024) study shows that irregular sleep patterns increase mortality risk regardless of average duration. "Catching up" on weekends creates social jetlag and disrupts your circadian rhythm. Consistent sleep schedules are more beneficial than variable schedules with the same average duration.
Myth 2: "As Long as I Get 8 Hours, I'm Fine"
Reality: All five studies demonstrate that sleep duration alone is insufficient. You can sleep 8 hours with poor quality, fragmented architecture, or at circadian-misaligned times and still experience negative health outcomes. Quality, regularity, and timing matter equally or more.
Myth 3: "I'm a Night Owl, So Late Sleep Is Fine for Me"
Reality: While chronotypes (natural preferences for sleep timing) vary, the Hartstein et al. (2025) review shows that sleeping severely misaligned with solar day-night cycles can disrupt circadian biology regardless of chronotype. Most people benefit from sleeping during predominantly dark hours.
Myth 4: "Sleep Problems Only Affect How Tired I Feel"
Reality: The AHA statement (St-Onge et al., 2025) makes clear that poor sleep health is an independent risk factor for cardiovascular disease, diabetes, obesity, and other serious conditions. Sleep problems have far-reaching effects beyond daytime fatigue.
Practical Action Steps: Improving Your Multidimensional Sleep Health
Step 1: Establish a Consistent Sleep Schedule
Choose a bedtime and wake time you can maintain 7 days per week
Set a sleep schedule alarm to remind you when to start winding down
Gradually adjust your schedule by 15-30 minutes if major changes are needed
Track your sleep regularity for 2-3 weeks to establish baseline
Step 2: Optimize Your Sleep Environment
Keep bedroom temperature cool (60-67°F / 15-19°C)
Eliminate or minimize light (use blackout curtains if necessary)
Reduce noise (consider white noise machines or earpurlings)
Invest in a comfortable mattress and pillows
Reserve your bed for sleep and intimacy only (no work or screens)
Step 3: Build a Wind-Down Routine
Start relaxation activities 60-90 minutes before bedtime
Dim household lighting in evening hours
Avoid screens or use blue-light filters after sunset
Try relaxation techniques: meditation, reading, gentle stretching
Avoid caffeine after early afternoon and alcohol near bedtime
Step 4: Align with Circadian Rhythms
Get bright light exposure within 30-60 minutes of waking
Spend time outdoors during daylight hours when possible
Exercise regularly but avoid intense workouts close to bedtime
Time your largest meals to earlier in the day
Avoid bright lights and stimulating activities in evening
Step 5: Address Sleep Disorders
If you experience:
Loud snoring or breathing pauses (possible sleep apnea)
Difficulty falling asleep or staying asleep 3+ nights per week (insomnia)
Uncomfortable sensations in legs at night (restless leg syndrome)
Excessive daytime sleepiness despite adequate time in bed
Consult a sleep medicine specialist for evaluation. Untreated sleep disorders prevent optimization of other sleep dimensions.
Step 6: Monitor Subjective Sleep Quality
How refreshed you feel upon waking
Your energy levels throughout the day
Your mood and emotional regulation
Your cognitive performance (focus, memory, decision-making)
These subjective measures are valuable indicators of sleep health beyond any objective metrics.
Special Considerations for Different Life Stages
Young Adults and College Students
Young adults often experience irregular sleep schedules due to academic and social demands. However, this demographic may face consequences decades later. Prioritize sleep regularity even when total sleep time is constrained.
Parents of Young Children
Parents often face sleep disruption that's unavoidable in the short term. Focus on:
Maintaining consistent wake times even when nighttime sleep is fragmented
Taking brief strategic naps when possible (20-30 minutes)
Tag-teaming with partners to ensure one person gets consolidated sleep
Being patient—this phase is temporary
Shift Workers
Shift workers face unique challenges with circadian misalignment. Strategies include:
Keeping the same sleep schedule even on days off when possible
Using bright light therapy strategically
Creating a very dark sleep environment during daytime sleep
Considering melatonin supplementation under medical guidance
Older Adults
Older adults often experience changes in sleep architecture and earlier circadian timing. Focus on:
Adjusting bedtime earlier if natural circadian shift occurs
Maintaining sleep regularity despite potential for earlier wake times
Addressing age-related sleep disorders (sleep apnea becomes more common)
Staying physically active during the day
Frequently Asked Questions (FAQs)
Q1: How much does sleep regularity matter compared to sleep duration?
A: Research by Windred et al. (2024) found that sleep regularity is a stronger predictor of mortality than sleep duration. While adequate sleep duration remains important, maintaining consistent bed and wake times appears to be even more critical for long-term health outcomes.
Q2: Can I catch up on lost sleep during weekends?
A: Unfortunately, "catch-up sleep" may do more harm than good. Sleeping in on weekends creates social jetlag and irregular sleep patterns that increase mortality risk (Windred et al., 2024). It's better to maintain consistent sleep schedules throughout the week, even if that means accepting slightly shorter sleep on some nights.
Q3: What if I naturally feel better with irregular sleep times?
A: While individual preferences exist, the research is clear that irregular sleep patterns disrupt circadian biology regardless of subjective feelings (Hartstein et al., 2025). Long-term health consequences accumulate even if you don't feel immediately impaired. Consistency benefits everyone, though chronotype influences optimal sleep timing.
Q4: How can I improve my sleep quality, not just duration?
A: Focus on:
Creating an optimal sleep environment (dark, cool, quiet)
Screening for sleep disorders like sleep apnea
Establishing a consistent wind-down routine
Avoiding sleep fragmenting behaviors (alcohol, late meals, screen time)
Ensuring sufficient time for complete sleep cycles (Arora & Moreno, 2025)
Q5: Do sleep trackers help with multidimensional sleep health?
A: Sleep trackers can be useful for monitoring sleep regularity and identifying patterns, but many have limited accuracy for sleep stage assessment. Use them as general guides while also paying attention to subjective sleep quality and daytime functioning, which may be equally or more informative (Corliss, 2025).
Q6: What are the most important sleep dimensions for heart health?
A: According to the American Heart Association (St-Onge et al., 2025), all six dimensions contribute to cardiometabolic health, but regularity, timing, and quality appear particularly important. Irregular sleep and circadian misalignment increase cardiovascular disease risk independent of duration.
Q7: Can improving sleep regularity reduce my risk of early death?
A: Yes. The UK Biobank study found that individuals with more regular sleep patterns had significantly lower all-cause mortality, cardiovascular mortality, and cancer mortality (Windred et al., 2024). Improving sleep regularity is one of the most impactful changes you can make for longevity.
Q8: How long does it take to see health benefits from improving sleep?
A: Some benefits appear quickly—improved mood, cognitive function, and energy within days to weeks. However, benefits for metabolic health, cardiovascular risk, and mortality accrue over months to years of sustained healthy sleep patterns. Consistency is key.
Call to Action: Start Your Sleep Health Transformation Today
The science is clear: optimal sleep goes far beyond simply getting 8 hours. To truly optimize your health, longevity, and daily functioning, you need to address all dimensions of sleep health—regularity, quality, timing, efficiency, and satisfaction.
Your 7-Day Sleep Health Challenge
Ready to transform your sleep? Try this week-long challenge:
Day 1-2: Track your current sleep patterns, including bedtime, wake time, and how you feel each morning.
Day 3-4: Choose a consistent bedtime and wake time you can maintain all week, including weekends. Set reminder alarms.
Day 5-6: Optimize your sleep environment—make your bedroom darker, cooler, and quieter. Remove screens from the bedroom.
Day 7: Establish a wind-down routine starting 60 minutes before your chosen bedtime. Dim lights, avoid screens, and practice relaxation.
When to Seek Professional Help
If you've optimized your sleep behaviors but still experience:
Persistent daytime sleepiness
Difficulty falling or staying asleep most nights
Loud snoring or breathing pauses during sleep
Uncomfortable leg sensations preventing sleep
Schedule an appointment with a sleep medicine specialist. Many treatable sleep disorders interfere with multidimensional sleep health.
Author’s Note
Sleep is often discussed in terms of hours alone, yet decades of clinical experience and an expanding body of research tell a far more complex story. As a physician and medical educator, I have repeatedly encountered patients who “sleep enough” by conventional standards but continue to struggle with fatigue, cardiometabolic disease, cognitive decline, and reduced quality of life. This disconnect prompted a deeper look into the emerging science of multidimensional sleep health.
The evidence reviewed in this article reflects a major shift in sleep medicine—from a narrow focus on duration to a broader understanding that sleep regularity, quality, timing, and circadian alignment are equally critical determinants of health. Landmark studies from 2024–2025, including the American Heart Association scientific statement and large population cohorts, now clearly demonstrate that irregular or poor-quality sleep independently increases the risk of cardiovascular disease, metabolic disorders, and premature mortality.
This article was written to bridge the gap between cutting-edge sleep research and practical, patient-centered guidance. My goal is to help readers move beyond clock-watching and toward a more meaningful, sustainable approach to sleep—one that supports long-term heart health, metabolic resilience, cognitive performance, and longevity.
Good sleep is not merely about more hours in bed; it is about sleeping regularly, restoratively, and in harmony with our biology.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Individual circumstances vary, and treatment decisions should always be made in consultation with qualified healthcare professionals.
Related Articles
The Sleep Switch is Real: Scientists Isolate the Brain Circuit That Dictates Muscle Mass and Fat Loss | DR T S DIDWAL
Sleep & Hypertension: Duration, Quality, and Blood Pressure | DR T S DIDWAL
References
Arora, T., & Moreno, C. R. C. (2025). Sleep and sleep disorders: Much more than how long you sleep, what truly matters is how you sleep. Scientific Reports, 15, 38097. https://doi.org/10.1038/s41598-025-25612-1
Corliss, J. (2025, August 1). The many dimensions of a good night's sleep. Harvard Health Publishing. https://www.health.harvard.edu/heart-health/the-many-dimensions-of-a-good-nights-sleep
Hartstein, L. E., Grandner, M. A., & Diniz Behn, C. (2025). Sleep irregularity and circadian rhythmicity: Implications for health and well-being. Current Sleep Medicine Reports, 11, 5. https://doi.org/10.1007/s40675-025-00318-y
St-Onge, M.-P., Aggarwal, B., Fernandez-Mendoza, J., Johnson, D., Kline, C. E., Knutson, K. L., Redeker, N., & Grandner, M. A. (2025). Multidimensional sleep health: Definitions and implications for cardiometabolic health: A scientific statement from the American Heart Association. Circulation: Cardiovascular Quality and Outcomes. https://doi.org/10.1161/HCQ.0000000000000139
Windred, D. P., Burns, A. C., Lane, J. M., Saxena, R., Rutter, M. K., Cain, S. W., & Phillips, A. J. K. (2024). Sleep regularity is a stronger predictor of mortality risk than sleep duration: A prospective cohort study. Sleep, 47(1), zsad253. https://doi.org/10.1093/sleep/zsad253